Abstract
Objective
To obtain preliminary data on the efficacy of yoga for reducing self-reported menopausal hot flashes in a randomized study including an attention control group.
Methods
We randomized 54 women late perimenopausal (2–12 months of amenorrhea) and postmenopausal women (12 or more months of amenorrhea), aged 45–58 years, with at least 4 hot flashes per day on average, for at least 4 weeks, to one of three groups: yoga, health and wellness education (HW) classes, and a wait list (WL) control group. Yoga and HW classes consisted of weekly 90 minute classes for 10 weeks. All women completed daily hot flash diaries throughout the trial (10 weeks) to track frequency and severity of hot flashes. The mean hot flash index score is based on the number of mild, moderate, severe and very severe hot flashes.
Results
Hot flash frequency declined significantly over time for all three groups with the strongest decline during the first week. There was no overall significant difference in hot flash frequency decrease over time by treatment groups, but the yoga and HW groups followed similar patterns and both showed greater decreases than the WL group. By week 10, women in the yoga group reported a decrease of approximately 66% in hot flash frequency, 63% in HW, and 36% in the WL group. The hot flash index showed a similar pattern.
Conclusions
Results suggest that yoga can serve as a behavioral option for reducing hot flashes, but they also suggest that yoga may not offer any advantage over other types of interventions.
Keywords: vasomotor symptoms, yoga, hot flashes, menopause
Hot flashes and/or night sweats (vasomotor symptoms) are the most common and troubling symptoms associated with menopause and are experienced by 64% to 80% of women undergoing natural menopause and almost all women who undergo surgical menopause.1–3 For many women, these symptoms are frequent and severe enough to become debilitating and impact their quality of life.4–10 Hot flashes are one of the chief menopausal complaints for which women in Western societies seek medical treatment11 and are the primary reason that women begin hormone therapy (HT).12–16
HT is currently the gold standard for treatment of vasomotor symptoms. A Cochrane Database systematic review showed a 75% reduction in hot flash frequency with HT compared to placebo.17 However, findings from the Women’s Health Initiative (WHI) trial suggest that benefits of HT can be outweighed by risks, such as coronary heart disease, stroke, pulmonary embolism, breast cancer, and probable dementia.18 The wide publicity of the WHI results has heightened women’s concerns about taking HT and led to a decrease in HT use.19,20
Many women have sought alternative treatments for hot flashes including other pharmaceutical agents, herbal or dietary remedies, and behavioral therapies,21,22 but these treatments show mixed results. Pharmaceutical agents are often ineffective or have a high incidence of side effects, though some antidepressants show promising results.23 Two reviews of randomized controlled clinical trials of complementary health approaches for hot flashes did not find evidence that herbs and nutritional supplements were beneficial.24,25
Behavioral interventions involving relaxation and slow deep, abdominal breathing, however, have been found to be useful for reducing mild- to moderate-intensity hot flashes.26–28 Such breathing forms the most integral core of any yoga practice.29,30 Yoga practice involves the combination of physical postures (asanas), breathing (pranayama), and deep relaxation (savasana). Two uncontrolled studies of yoga interventions found reductions in hot flashes.31,32 Studies employing various control groups have also showed promising results, but have used very intensive yoga interventions (at least 5 days per week),33,34 did not measure daily hot flashes,33–35 combined the yoga intervention with education,33 or lacked an attention control group.36
The objective of the current study was to obtain preliminary data on the efficacy of yoga for reducing self-reported menopausal hot flashes in a randomized study that included an attention control group and measured daily hot flashes. Attention control groups are important to help understand the true impact of an active intervention. We hypothesized that women participating in a yoga intervention would achieve a greater reduction in subjective hot flash frequency and severity than women in an educational control group or a waitlist control group. As a pilot study, we also sought to examine the effect of yoga on self-reported hot flash interference, sleep, anxiety, depressive symptoms, perceived stress, and quality of life; and to track the recruitment, retention, and adherence to the protocol.
METHODS
Study Design
We conducted a randomized study consisting of three groups: yoga, health and wellness education (HW) classes, and a waitlist (WL) control group. The HW group served to control for attention, time and social aspects of the yoga intervention. The WL group controlled for the placebo effect since randomized controlled trials of estrogen therapy typically show, on average, that hot flash frequencies and hot flash scores diminish by about 20% to 30% with 4 weeks of a placebo.37 This reduction may be due to the natural decline in symptoms over time or to the placebo effect of being in a trial. It is therefore critical to have an inactive control group to assess the effect of the natural decline in symptoms.
Procedure
Eligible participants included late perimenopausal and early postmenopausal women, aged 45–58 years, with at least 4 hot flashes per day on average, for at least 4 weeks, and at least 2 months since last menses. Women were stratified on menopausal status based on the criteria developed by the Stages of Reproductive Aging Workshop (STRAW).38 Late peri-menopause was defined as 2–12 months of amenorrhea and post menopause as 12 or more months of amenorrhea. Women who had a surgical menopause were classified as postmenopausal. Women who had taken HT within the past 12 weeks were not eligible. Because hormone-modulating therapies can impact ovarian function and increase hot flashes, women taking such therapies (e.g., tamoxifen) within the past 6 months were not eligible. Women with a history of cancer needed to be at least 5 years post diagnosis and off chemotherapy for at least one year. We also excluded women who had untreated thyroid disease which can increase hot flashes, past use of yoga specifically for hot flashes, and any use of yoga or acupuncture in the past 3 months. Women who had recently initiated herbal or nutritional remedies within the past 4 weeks were excluded as these remedies may take several weeks to have an effect. We initially excluded women taking psychoactive medications, including anti-depressants and anxiolytics, as these medications may reduce hot flashes. However, because many women were taking antidepressants, we subsequently eliminated antidepressants as a criterion but required that women be on a stable dose for 3 months at enrollment. The ability to read and understand English was an additional requirement.
Women were recruited through newspaper advertisements, radio announcements, and hospital postings and screened for initial eligibility over the telephone. Women who met initial eligibility criteria were scheduled for a baseline clinic visit. At the baseline clinic visit, informed consent was obtained and baseline questionnaires were administered. To confirm that women had a sufficient number of hot flashes for study eligibility, participants were asked to complete the Daily Diary of Hot Flashes (DDHF) on a daily basis for the next two weeks and mail it to the study coordinator. Women who met the criterion of an average of at least 4 hot flashes per day based on the DDHF were randomized to one of the three study groups. Participants assigned to the two intervention groups could begin class participation at any time within the next four weeks (women were encouraged to begin within 2 weeks). Women assigned to the WL group were told they would be contacted in 10 weeks to begin either the yoga or HW classes. Women in the WL group were subsequently randomized to yoga or education to avoid the expectation that one intervention was preferable and to provide an incentive for staying in the study.
All study participants completed questionnaires 5 weeks after baseline, at the end of trial (10 weeks after baseline), and 2 months following completion of the trial. All women completed weekly hot flash diaries throughout the trial (10 weeks). All study participants agreed not to take hormonal medications or initiate other treatments for their hot flashes during the study. The study protocol was approved by the Wake Forest School of Medicine Institutional Review Board.
Study Groups
Yoga
The study intervention consisted of 10, weekly, 90-minute Integral Yoga classes. Classes were offered on a continuous basis with rolling admission. The basic elements of most any yoga practice involve the combination of breathing (pranayama), physical postures (asanas), and deep relaxation (savasana). We chose Integral Yoga as particularly well-suited to women experiencing hot flashes largely because of the major emphasis on stress reduction and decreased likelihood of increasing heat (an undesirable effect in women with hot flashes).39 Each class was adjusted to the mixture of abilities of those present, but included the same basic elements (adapted from Satchidananda39) in the following three categories: (1) breathing (pranayama)/centering meditation (15 minutes) – centering meditation (1–2 minutes) (aligning the body in a comfortable seated position, paying attention to any physical sensations, noticing the breath) and deep 3-part breathing; (2) physical postures (asanas) (45 minutes) included: warm-up (e.g., cat pose); modified sun salutations; standing poses (e.g., Warrior I or II, King Dancer); brief deep relaxation; backward bending (e.g., Cobra, Boat pose, optional Bow pose); forward bending (e.g., head-to-knee pose, forward bend, half spinal twist); inverted poses (e.g., half shoulder stand, legs up the wall, downward-facing dog); fish pose or supine spinal twist; upright spinal twist; and yoga mudra; and (3) deep relaxation (Savasana) (30 minutes) that included Yoga Nidra and additional Pranayama (alternate nostril breathing).
In addition to the group classes, participants were asked to practice yoga at home for 15 minutes ≥ 3 times per week using a DVD videorecording produced for this study. Home practice consisted of a warm-up (circling hands and feet to warm-up the wrist and ankle joints, rotating shoulder joints, and cat/cow stretch on hands and knees into child pose to stretch the lower back), backward bend (cobra pose), forward bend (head to knee pose), inversion (modified shoulder stand), gentle twist (reclining spinal twist), deep relaxation, deep 3-part breathing, and a final period of stillness and silence.
The yoga instructor was a Registered Yoga Alliance teacher and Certified Integral Yoga instructor. In addition, we also had a consultant from the New York Integral Yoga Institute review the protocol and DVD that we made for home practice.
Health and Wellness (HW) Control Group
This group was designed to control for time, attention, and social aspects of the yoga intervention. It was designed to be “believable” for menopausal women without being efficacious for reducing hot flashes. Classes consisted of 10 weekly, 90-minute didactic educational classes on different topics: menopause, stress management (2 sessions), bone health, cardiovascular health, nutrition, financial planning, skin care, aging and long-term health planning, and cancer prevention and screening. Similar to the yoga classes, women could enter the group at any time. Women were given materials to read at home in an attempt to match the time spent in home yoga practice.
Wait List (WL) Control Group
Participants in this group did not participate in any classes for 10 weeks and were instructed not to initiate any new treatments for their hot flashes during this time. They completed weekly hot flash diaries and study questionnaires at weeks 5 and 10. We selected a waitlist control design rather than usual care because we previously learned40 that women do not like being assigned to a group that does not receive any treatment. With a waitlist control design, these women were assured of receiving some intervention, thereby enhancing recruitment and retention. The data of interest for this group were obtained during weeks 1–10 while waiting to participate in the yoga or HW classes.
Measures
The primary study outcome was frequency and severity of hot flashes, as measured by the Daily Diary of Hot Flashes (DDHF) developed by Sloan.37 The DDHF records the frequency and severity of hot flashes using a 4- point scale from mild (sensation of heat without perspiration), moderate (sensation of heat with perspiration - able to continue activity), severe (sensation of heat with sweating causing a stop activity or disrupting sleep) to very severe (sensation of heat with severe sweating, disrupting activity, requiring a change of sheets or clothes) to provide a Hot Flash Index (the sum of the number of hot flashes multiplied by severity). This diary has been used in multiple trials on hot flashes and exhibited consistency and reliability.37
Secondary study outcomes included hot flash interference, sleep quality, anxiety, depressive symptoms, perceived stress, and quality of life. The Hot Flash Related Daily Interference Scale (HFRDIS) is a 10-item psychometrically sound measure for assessing the impact of vasomotor symptoms on daily activities in nine specific domains within the past week (work, social activities, leisure activities, sleep, mood, concentration, relation with others, sexuality, and enjoyment of life) and overall quality of life.41 Item responses range from 1 not at all to 10 extremely. The global sleep quality index (GSQI) of the 19-item Pittsburgh Sleep Quality Index was used to measure sleep patterns and quality.42,43 Scores range from 0 – 16, with scores ≥5 indicating poor sleep quality and high sleep disturbances. Depressive symptoms were assessed with the Center for Epidemiological Studies Depression Scale short form (CESD-10),44 a validated self-report questionnaire that measures the frequency of 10 depressive symptoms “during the past week.” Total score ranges from 0 to 30, with higher scores indicating greater depressive symptoms. Scores ≥10 are indicative of clinically significant depressive symptoms.
The 10-item Hopkins Symptom Checklist (HSCL)45,46 assesses the presence and intensity of anxiety symptoms during the previous week. A total score of 1.55 or higher indicates moderate anxiety symptoms, and a score of 1.75 or higher indicates severe anxiety. The HSCL has been used in previous studies of treatments for menopausal symptoms.47 The 4-item Perceived Stress Scale (PSS)48,49 assessed four aspects of self-reported, perceived stress experienced over the past two weeks (from 1=never to 5=very often). Items are summed so that the total score ranges from 4–20.
Global quality of life (QOL) was assessed via a single-item 100mm visual analogue scale (VAS) where participants rate their overall quality of life along a line where 0 is the lowest possible quality of life and 100 is the highest. Health-related quality of life was measured using the MOS 36-Item Short Form Health Survey (SF-36).50 The SF-36 is one of the most widely used measures of health status consisting of 36 items measuring the following 2 components: Physical Component Score (PCS) and Mental Component Score (MCS). Scores are standardized to a mean of 50.
Statistical Analyses
Statistical analyses were performed using the SAS statistical package. This pilot study of 54 participants was conducted to examine trends and to plan a larger clinical trial. Recruitment and retention are presented in a CONSORT diagram. Reasons for drop-outs, and number of yoga or HW classes attended were tabulated. Group comparisons of baseline characteristics included χ2 and Fisher exact tests for categorical variables and analysis of variance for continuous variables. Our primary aim addressed the effect of yoga on the frequency and severity of reported hot flashes. Log-transformed data were analyzed following an intention-to-treat analysis and results were back-transformed to original units. A linear mixed model with repeated measures (PROC mixed in SAS) 51,52 was used with group, week, and group*week in the model adjusting for baseline outcome and menopausal status (peri or post). The adjusted ratio of frequency and severity of hot flashes at a specific week versus baseline values * 100, based on log-transformed data, were also plotted.
Secondary outcomes, including hot flash interference (HFRDIS), sleep quality (GSQI), depressive symptoms (CESD-10), anxiety symptoms (HSCL), perceived stress (PSS), general QOL, and mental and physical components of QOL (SF-36 MCS and PCS) were analyzed with the same methods as the primary outcome.
RESULTS
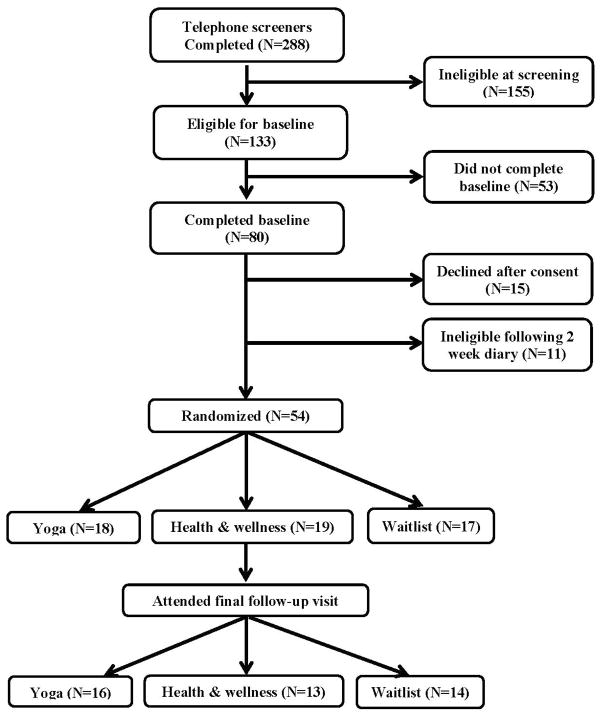
Participant data are shown in Figure 1. A total of 449 women responded to advertisements; 288 of these women completed the telephone screener, and 161 were never reached after at least 3 attempts. Of the 288 women who were screened, 133 met initial eligibility criteria, and 155 were ineligible. The primary reasons for ineligibility included: too few hot flashes (n=67), on anti-depressants (n=48) (an exclusion criterion later changed as mentioned in the Methods section), not yet perimenopausal (n=32), recent yoga practice (n=29), and recent cancer (n=26).
Figure 1.
CONSORT Diagram
Of the 133 eligible women, 80 completed baseline visits and 65 agreed to be randomized but 11 were ineligible for further participation after completion of the 2-week hot flash diary, yielding 54 women who were enrolled and randomized. At the final follow-up, 79.6% of the women remained in the study (15 Yoga, 14 HW and 14 WL). Reasons for dropping out included transportation issues (n=2), time constraints (n=2), reported inability to do yoga (n=1), and unspecified reasons (n=6).
At least 8 of 10 classes were attended by 50% of women in the yoga group and 47% of women in the HW group. At least 6 of 10 classes were attended by 61% of women in the yoga group and 63% in the HW group.
Baseline Characteristics
Baseline characteristics by group assignment are shown in Table 1. There were no differences in demographic variables among the three groups. The average number of hot flashes per day were 10.1, 8.7 and 9.1 in the WL, HW and yoga groups, respectively; 15% of the women were perimenopausal, and 40% were African American. All women in the WL group had some co-morbidities (most commonly arthritis and hypertension) which was significantly more than the other two groups (61% in both). There was a trend towards higher depressive symptoms and anxiety scores and lower MCS among women in the yoga group.
TABLE 1.
Baseline characteristics of study sample
| Yoga (n=18) |
Health and Wellness (n=19) |
Wait List n=17) |
p-value | |
|---|---|---|---|---|
| Mean (SE) | Mean (SE) | Mean (SE) | ||
| Demographics | ||||
| Age (yrs) | 53.5 (0.7) | 52.8 (0.7) | 53.5 (0.7) | 0.66 |
| N (%) | N (%) | N (%) | ||
| Race | 0.83 | |||
| White | 11 (65) | 12 (63) | 9 (52) | |
| African American | 6 (35) | 7 (37) | 8 (47) | |
| Education | ||||
| ≥ High School, < College | 10 (56) | 7 (37) | 7 (41) | 0.49 |
| ≥ College | 8 (44) | 12 (63) | 10 (59) | |
| Employed | 14 (78) | 13 (68) | 15 (88) | 0.43 |
| Hard to pay for basics | ||||
| Somewhat or very hard | 6 (33) | 6 (32) | 3 (18) | 0.55 |
| Not very hard at all | 12 (67) | 13 (68) | 14 (82) | |
| Income | ||||
| $10,000–$29,999 | 3 (17) | 6 (32) | 2 (12) | 0.50 |
| $30,000–$74,999 | 9 (50) | 6 (32) | 6 (35) | |
| ≥ $75,000 | 6 (33) | 7 (37) | 9 (53) | |
| Married/Partnered | 9 (50) | 12 (63) | 11 (65) | 0.65 |
| Current smoker | 0 (0) | 1 (5) | 1 (6) | 0.76 |
| Any exercise in past month | 15 (83) | 17 (89) | 12 (71) | 0.34 |
| Medical Characteristics | ||||
| Any comorbidity | 11 (61) | 11 (61) | 17 (100) | 0.01 |
| Hysterectomy | 7 (39) | 7 (37) | 8 (47) | 0.81 |
| Oophorectomy | ||||
| No | 11 (61) | 14 (74) | 12 (71) | 0.80 |
| One ovary removed | 2 (11) | 2 (11) | 3 (18) | |
| Both ovaries removed | 5 (28) | 3 (16) | 2 (12) | |
| Menopausal Status | ||||
| Peri | 3 (17) | 3 (16) | 2 (12) | 0.99 |
| Post | 15 (83) | 16 (84) | 15 (88) | |
| Mean (SE) | Mean (SE) | Mean (SE) | ||
| Years since last menstrual period | 2.9 (0.9) | 2.5 (0.7) | 3.8 (1.1) | 0.601 |
| Years with hot flashes | 1.6 (0.4) | 2.0 (0.4) | 2.2 (0.5) | 0.681 |
| Hot flashes per day | 9.1 (1.2) | 8.7 (1.2) | 10.1 (1.5) | 0.592 |
| Symptoms and Quality of life | ||||
| HFRDIS | 4.7 (0.5) | 4.1 (0.5) | 4.6 (0.6) | 0.72 |
| Sleep quality (GSQI) | 10.9 (0.9) | 8.5 (0.9) | 9.9 (0.9) | 0.15 |
| Depressive symptoms (CESD-10) | 10.8 (1.3) | 7.2 (1.2) | 7.3 (1.3) | 0.08 |
| Perceived stress (PSS) | 5.4 (0.9) | 3.5 (0.8) | 4.5 (0.9) | 0.27 |
| Hopkins Symptoms Check List | 1.6 (0.1) | 1.4 (0.1) | 1.7 (0.1) | 0.06 |
| Global quality of life (VAS) | 68.4 (5.4) | 73.0 (4.1) | 72.5 (4.1) | 0.68 |
| SF-36 MCS | 41.3 (2.4) | 50.5 (2.3) | 60.4 (2.5) | 0.01 |
| SF-36 PCS | 54.4 (1.3) | 54.1 (1.3) | 51.4 (1.4) | 0.22 |
From log-transformed data.
From log-transformed data adjusted for menopausal status
SE: Standard Error; HFRDIS, Hot Flash Related Daily Interference Scale; GSQI, Global Sleep Quality Index; CESD-10, Center for Epidemiological Studies Depression Scale, short form; PSS, Perceived Stress Scale; SF-36, MOS 36-item Short form Health Survey; MCS, Mental Component Score; PCS, physical component score.
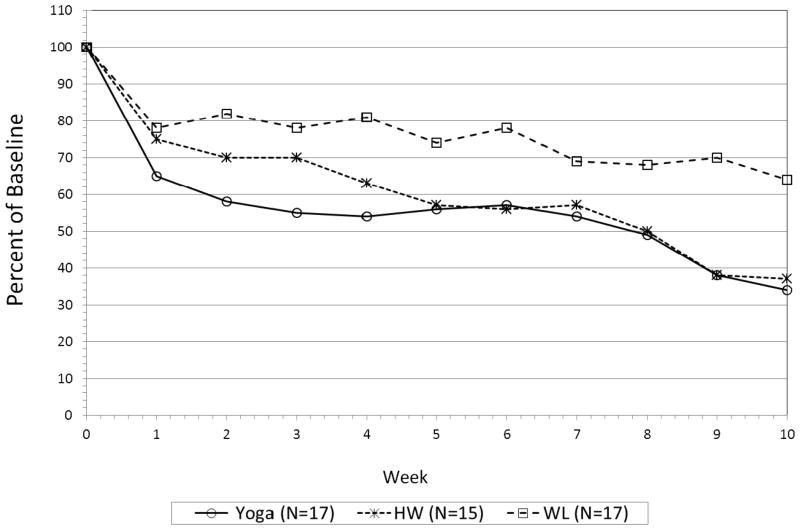
Hot Flash Change
Forty-nine of the 54 participants returned at least one follow-up diary and were included in the analyses (15 WL, 17 HW and 17 yoga). By week 10, 13 WL, 14 HW and 12 Yoga participants returned their diaries. Means for the hot flash frequency and hot flash index by week and group are shown in Table 2. Figure 2 shows percent of daily hot flashes from baseline each week. Hot flash frequency declined significantly over time for all three groups (p<0.0001) with the strongest decline during the first week. Differences in hot flash frequency over time tended to be larger between the WL and yoga group. By the third week of treatment, women in the yoga group reported a decrease of approximately 45% in hot flash frequency compared to about 22% for the WL group. The HW group showed a similar decrease to the yoga group from weeks 5 to 10. The WL group showed an initial decline of 22% at week 1, but remained fairly stable until week 7 when hot flash frequency decreased slightly more. At week 10, we found a reduction of 66% in hot flashes for the yoga and 63% for the HW group, compared to 36% in the WL group. These percentages represent a decrease in means of 6.5 hot flashes per day in the yoga group, 5.9 in the HW group and 4.2 in the WL group.
TABLE 2.
Frequency and severity index of hot flashes per day [mean (SE)] adjusted for baseline values and menopausal status, by week
| Yoga (n=18) |
Health and Wellness (n=19) |
Wait List (n=17) |
p-value | ||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Gr*Week | Group | Week | |||||
| Frequency | Week | 0.91 | 0.18 | <0.0001 | |||
| 1 | 5.7 (1.1) | 6.5 (1.3) | 6.8 (1.4) | ||||
| 2 | 5.1 (1.0) | 6.1 (1.2) | 7.2 (1.5) | ||||
| 3 | 4.8 (0.9) | 6.1 (1.2) | 6.8 (1.4) | ||||
| 4 | 4.7 (0.9) | 5.5 (1.1) | 7.1 (1.5) | ||||
| 5 | 4.9 (0.9) | 5.0 (1.0) | 6.6 (1.4) | ||||
| 6 | 5.0 (1.0) | 4.9 (1.0) | 6.8 (1.4) | ||||
| 7 | 4.7 (0.9) | 5.0 (1.0) | 6.0 (1.3) | ||||
| 8 | 4.3 (0.9) | 4.3 (0.9) | 5.9 (1.2) | ||||
| 9 | 3.3 (0.7) | 3.3 (0.7) | 6.1 (1.3) | ||||
| 10 | 3.0 (0.6) | 3.2 (0.7) | 5.5 (1.2) | ||||
| Hot Flash Index | 0.70 | 0.14 | <0.0001 | ||||
| 1 | 10.7 (2.3) | 12.6 (2.8) | 13.2 (3.1) | ||||
| 2 | 9.7 (2.1) | 11.7 (2.6) | 13.6 (3.1) | ||||
| 3 | 8.9 (2.0) | 11.2 (2.4) | 13.1 (3.0) | ||||
| 4 | 8.7 (1.9) | 10.2 (2.2) | 14.4 (3.4) | ||||
| 5 | 9.5 (2.1) | 8.8 (1.9) | 13.3 (3.2) | ||||
| 6 | 9.0 (2.0) | 8.5 (1.9) | 13.5 (3.3) | ||||
| 7 | 8.5 (1.9) | 8.7 (2.0) | 11.8 (2.8) | ||||
| 8 | 8.3 (2.0) | 7.3 (1.6) | 11.6 (2.8) | ||||
| 9 | 6.2 (1.5) | 5.2 (1.2) | 12.3 (2.9) | ||||
| 10 | 5.5 (1.3) | 5.1 (1.2) | 10.9 (2.6) | ||||
Note: Transformed back to original units from log-transformed values. Main effects p-values are from a model excluding the group*week interaction.
Figure 2.
Percent of baseline hot flash frequency over time by intervention group.
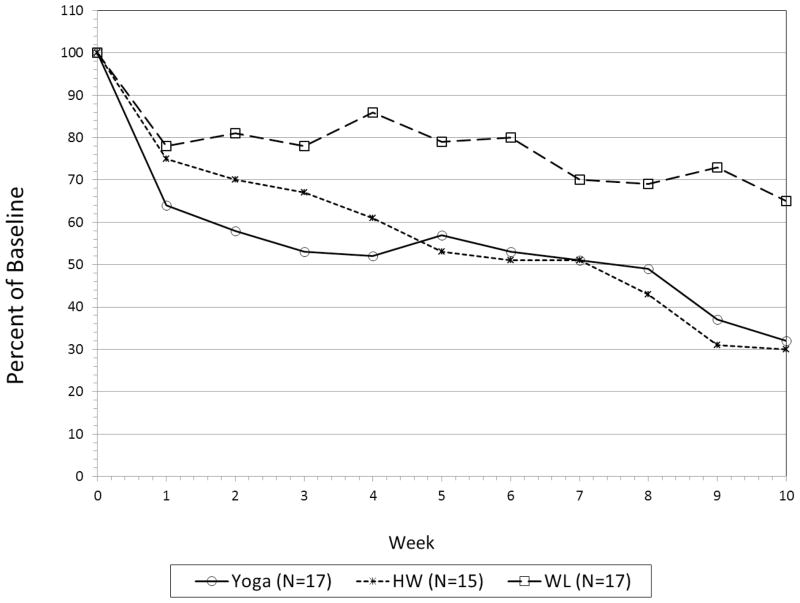
Figure 3 shows the results using the hot flash index, which takes into account both frequency and severity. This figure shows a pattern similar to that for frequency alone. There is a general decline over time and the week 10 mean hot flash index in the yoga and WL groups is half that of the WL group.
Figure 3.
Percent of baseline hot flash index over time by intervention group.
Quality of Life Outcomes
Although this small pilot study was not powered to find small differences, patterns of hot flash interference and depressive symptoms (CESD-10) did not change appreciably (Table 3). At week 10, the WL group showed better sleep quality, improved overall QOL and a tendency for less perceived stress over time, while the education group reported worse sleep quality and quality of life and more perceived stress. Sleep quality, quality of life and perceived stress did not change meaningfully in the yoga group.
TABLE 3.
Quality of life outcomes by intervention group and week, controlling for baseline values
| Yoga | Health & Wellness | Wait List | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Outcome | Week 5 (n=16) |
Week 10 (n=15) |
Week 5 (n=15) |
Week 10 (n=14) |
Week 5 (n=14) |
Week 10 (n=14) |
P-value Group *Week |
| HFRDIS | 3.15 (0.49) | 3.00 (0.51) | 2.78 (0.50) | 2.65 (0.51) | 3.67 (0.53) | 3.55 (0.53) | 0.99 |
| Sleep Quality (GSQI) | 9.39 (0.73) | 8.93 (0.75) | 8.07 (0.75) | 9.00 (0.77) | 9.28 (0.79) | 7.64 (0.79) | 0.04 |
| Depressive Symptoms (CESD10) | 8.67 (1.08) | 8.11 (1.11) | 7.71 (1.09) | 8.77 (1.11) | 8.79 (1.15) | 8.57 (1.15) | 0.53 |
| Perceived Stress (PSS) | 3.53 (0.69) | 3.68 (0.74) | 3.34 (0.68) | 4.70 (0.97) | 4.02 (0.85) | 3.11 (0.66) | 0.08 |
| Global Quality of Life | 72.37 (4.03) | 77.39 (4.22) | 80.18 (4.24) | 66.11 (4.37) | 72.4 (4.35) | 79.17 (4.35) | 0.01 |
| Hopkins Symptoms Checklist (HSCL) | 1.48 (0.07) | 1.38 (0.07) | 1.36 (0.07) | 1.32 (0.06) | 1.51 (0.07) | 1.44 (0.07) | 0.84 |
| SF36 PCS | 50.91 (1.28) | 51.17 (1.33) | 54.31 (1.31) | 52.90 (1.34) | 54.25 (1.39) | 50.61 (1.43) | 0.14 |
| SF36 MCS | 51.32 (2.14) | 52.61 (2.22) | 50.79 (2.16) | 50.29 (2.20) | 49.42 (2.29) | 52.38 (2.33) | 0.53 |
DISCUSSION
This pilot study sought to obtain data on the feasibility and preliminary efficacy of yoga as an intervention for reducing menopausal hot flashes. The physiological rationale for investigating this relationship is based on several complex hypothesized pathways, especially pathways mediated by the hypothalamic-pituitary-adrenal axis, through which yoga is hypothesized to decrease arousal in the autonomic nervous system (ANS)53 In particular, the hormonal changes that occur during menopause are thought to be associated with a narrowing of the body’s thermoregulatory zone (thermoregulation being under the control of the ANS) at which the normal physiological response to induce heating or cooling occurs. This narrowing means that hot flashes are more likely to result when body temperature increases.54 A decrease in arousal of the ANS, hypothesized to be brought about by yoga, may thus lead to improved thermoregulation.
Our 3-group design incorporated both attention (i.e. health and wellness education) and waitlist control groups. Sloan et al.37 found that a reduction of 3.5 hot flashes per day corresponded to an increase of 6 points in quality of life on a 0-100-point scale, “a conservative estimate of a minimally clinically significant change.” All three groups met this threshold.
Our results provide additional support to previous studies for the potential benefits of yoga for reducing hot flashes.33–35 Several things are worth noting about our findings. First, we found meaningful reductions in hot flashes despite attendance at the classes being suboptimal and lower than in other studies.33,34 We also found a reduction in hot flashes in the WL group, consistent with other hot flash intervention studies that have shown a substantial placebo effect.37 A particularly noteworthy finding is the similarity of results between the yoga and HW groups. Randomized trials of behavioral interventions are criticized because greater expectations are often created in the intervention group as compared with an attention control group. We purposely presented our study as one comparing two types of interventions to reduce menopausal symptoms and tried to avoid any suggestion that the yoga group was of greater interest, thus attempting to equalize expectations in both groups, a clear methodological strength of this study.
Findings from the present study are very similar to those from a previous study we conducted on acupuncture for hot flashes.40 The acupuncture study was designed similarly with respect to eligibility and outcomes. In that study, women (n=56) were randomized to one of the three groups: usual care, placebo (sham acupuncture), or standardized individual acupuncture based on Traditional Chinese Medicine principles (TA). Results showed a significant decrease in mean frequency of hot flashes similar to that of the present study. There was a 35–40% reduction in hot flashes by week 2 for both the sham and TA groups. There was no difference by treatment group (p=0.15). However, when combined, the two acupuncture groups showed a significantly greater decrease than the usual care group (p<.05).
The results of our present study in combination with the acupuncture study find similar reduction in hot flashes for women in four different treatment groups: yoga, health and wellness, true acupuncture, and sham acupuncture. Both studies controlled for treatment expectations with the inclusion of active control groups. Taken together, these findings point to the importance of including active control groups in randomized intervention studies for menopausal hot flashes. They also raise the question of why these control groups are equally effective as the presumed active intervention. The question remains as to whether the active interventions are indeed efficacious or whether their efficacy is a result of the expectations that participants have for them.
This pilot study does raise some questions about feasibility. Recruitment was challenging because we could only offer the yoga and HW classes one time during the week. Providing more options for classes would enhance both recruitment and class attendance. Also, it was initially a challenge to present the HW intervention as one to reduce hot flashes, which led us to revise our presentation of the study more generally to reduce menopausal symptoms.
The present study had several limitations. The sample size was by design underpowered to detect important differences between groups. As previously mentioned, recruitment and class attendance were challenging largely due to the inability to offer more flexible and varied class days and times.
Despite these limitations, the present study has several strengths and important findings. Our 3-group design is an important advance over studies that lack groups that control for time or attention. Though larger studies are needed, this design and our results suggest that yoga can serve as a behavioral option for reducing hot flashes, but they also suggest that yoga may not offer any advantage over other types of interventions. This message is important for women as it suggests that any number of behavioral interventions may help to reduce hot flashes.
Acknowledgments
Research supported by Grant R21AT004234 from the National Center for Complementary and Alternative Medicine, National Institutes of Health
Footnotes
Financial Disclosure/Conflicts of Interest: none
ClincalTrials.gov identifier: NCT01073397
References
- 1.Avis NE, Crawford SL, McKinlay SM. Psychosocial, behavioral, and health factors related to menopause symptomatology. Womens Health. 1997;2:103–20. [PubMed] [Google Scholar]
- 2.Williams RE, Kalilani L, DiBenedetti DB, et al. Frequency and severity of vasomotor symptoms among peri- and postmenopausal women in the United States. Climacteric. 2008;1:32–43. doi: 10.1080/13697130701744696. [DOI] [PubMed] [Google Scholar]
- 3.Woods NF, Mitchell ES. Symptoms during the perimenopause: prevalence, severity, trajectory, and significance in women’s lives. Am J Med. 2005:14–24. doi: 10.1016/j.amjmed.2005.09.031. [DOI] [PubMed] [Google Scholar]
- 4.Avis NE, Ory M, Matthews KA, Schocken M, Bromberger J, Colvin A. Health-related quality of life in a multiethnic sample of middle-aged women: Study of Women’s Health Across the Nation (SWAN) Med Care. 2003;11:1262–76. doi: 10.1097/01.MLR.0000093479.39115.AF. [DOI] [PubMed] [Google Scholar]
- 5.Daly E, Gray A, Barlow D, McPherson K, Roche M, Vessey M. Measuring the impact of menopausal symptoms on quality of life. Brit Med J. 1993:836–40. doi: 10.1136/bmj.307.6908.836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ledesert B, Ringa V, Breart G. Menopause and perceived health status among the women of the French GAZEL cohort. Maturitas. 1994;2–3:113–20. doi: 10.1016/0378-5122(94)90006-x. [DOI] [PubMed] [Google Scholar]
- 7.Fuh JL, Wang SJ, Lee SJ, Lu SR, Juang KD. Quality of life and menopausal transition for middle-aged women on Kinmen island. Qual Life Res. 2003;1:53–61. doi: 10.1023/a:1022074602928. [DOI] [PubMed] [Google Scholar]
- 8.Kumari M, Stafford M, Marmot M. The menopausal transition was associated in a prospective study with decreased health functioning in women who report menopausal symptoms. J Clin Epidemiol. 2005;7:719–27. doi: 10.1016/j.jclinepi.2004.09.016. [DOI] [PubMed] [Google Scholar]
- 9.Utian WH. Psychosocial and socioeconomic burden of vasomotor symptoms in menopause: a comprehensive review. Health Qual Life Outcomes. 2005:47. doi: 10.1186/1477-7525-3-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Williams RE, Levine KB, Kalilani L, Lewis J, Clark RV. Menopause-specific questionnaire assessment in US population-based study shows negative impact on health-related quality of life. Maturitas. 2009;2:153–9. doi: 10.1016/j.maturitas.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 11.Williams RE, Kalilani L, DiBenedetti DB, Zhou X, Fehnel SE, Clark RV. Healthcare seeking and treatment for menopausal symptoms in the United States. Maturitas. 2007;4:348–58. doi: 10.1016/j.maturitas.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 12.Johannes CB, Crawford SL, Posner JG, McKinlay SM. Longitudinal patterns and correlates of hormone replacement therapy use in middle-aged women. Am J Epidemiol. 1994;5:439–52. doi: 10.1093/oxfordjournals.aje.a117266. [DOI] [PubMed] [Google Scholar]
- 13.Kuh D, Hardy R, Wadsworth M. Social and behavioural influences on the uptake of hormone replacement therapy among younger women. BJOG. 2000;6:731–9. doi: 10.1111/j.1471-0528.2000.tb13333.x. [DOI] [PubMed] [Google Scholar]
- 14.Kuh DL, Wadsworth M, Hardy R. Women’s health in midlife: The influence of the menopause, social factors and health in earlier life. Brit J Obstet Gynaec. 1997:923–33. doi: 10.1111/j.1471-0528.1997.tb14352.x. [DOI] [PubMed] [Google Scholar]
- 15.Hunter MS, O’Dea I, Britten N. Decision-making and hormone replacement therapy: a qualitative analysis. Soc Sci Med. 1997;10:1541–8. doi: 10.1016/s0277-9536(97)00091-9. [DOI] [PubMed] [Google Scholar]
- 16.Porter M, Penney GC, Russell D, Russell E, Templeton A. A population based survey of women’s experience of the menopause. Brit J Obstet Gynaec. 1996:1025–8. doi: 10.1111/j.1471-0528.1996.tb09555.x. [DOI] [PubMed] [Google Scholar]
- 17.Maclennan AH, Broadbent JL, Lester S, Moore V. Oral oestrogen and combined oestrogen/progestogen therapy versus placebo for hot flushes. Cochrane Database Syst Rev. 2004;4:CD002978. doi: 10.1002/14651858.CD002978.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rossouw JE, Anderson GL, Prentice RL, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women’s Health Initiative randomized controlled trial. JAMA. 2002;3:321–33. doi: 10.1001/jama.288.3.321. [DOI] [PubMed] [Google Scholar]
- 19.Haas JS, Kaplan CP, Gerstenberger EP, Kerlikowske K. Changes in the use of postmenopausal hormone therapy after the publication of clinical trial results. Ann Intern Med. 2004;3:184–8. doi: 10.7326/0003-4819-140-3-200402030-00009. [DOI] [PubMed] [Google Scholar]
- 20.Tsai SA, Stefanick ML, Stafford RS. Trends in menopausal hormone therapy use of US office-based physicians, 2000–2009. Menopause. 2011;4:385–92. doi: 10.1097/gme.0b013e3181f43404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nedrow A, Miller J, Walker M, Nygren P, Huffman LH, Nelson HD. Complementary and alternative therapies for the management of menopause-related symptoms: a systematic evidence review. Arch Intern Med. 2006;14:1453–65. doi: 10.1001/archinte.166.14.1453. [DOI] [PubMed] [Google Scholar]
- 22.Kessel B, Kronenberg F. The role of complementary and alternative medicine in management of menopausal symptoms. Endocrinol Metab Clin North Am. 2004;4:717–39. doi: 10.1016/j.ecl.2004.07.004. [DOI] [PubMed] [Google Scholar]
- 23.Pachman DR, Jones JM, Loprinzi CL. Management of menopause-associated vasomotor symptoms: Current treatment options, challenges and future directions. Int J Womens Health. 2010:123–35. doi: 10.2147/ijwh.s7721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kronenberg F, Fugh-Berman A. Complementary and alternative medicine for menopausal symptoms: A review of randomized, controlled trials. Ann Intern Med. 2002:805–13. doi: 10.7326/0003-4819-137-10-200211190-00009. [DOI] [PubMed] [Google Scholar]
- 25.Huntley AL, Ernst E. A systematic review of herbal medicinal products for the treatment of menopausal symptoms. Menopause. 2003;5:465–76. doi: 10.1097/01.GME.0000058147.24036.B0. [DOI] [PubMed] [Google Scholar]
- 26.Sood R, Sood A, Wolf SL, et al. Paced breathing compared with usual breathing for hot flashes. Menopause. 2013;2:179–84. doi: 10.1097/gme.0b013e31826934b6. [DOI] [PubMed] [Google Scholar]
- 27.Freedman RR, Woodward S. Behavioral treatment of menopausal hot flushes: evaluation by ambulatory monitoring. Am J Obstet Gynecol. 1992:436–9. doi: 10.1016/s0002-9378(11)91425-2. [DOI] [PubMed] [Google Scholar]
- 28.Keefer L, Blanchard EB. Hot flash, hot topic: conceptualizing menopausal symptoms from a cognitive-behavioral perspective. Appl Psychophysiol Biofeedback. 2005;1:75–82. doi: 10.1007/s10484-005-2176-9. [DOI] [PubMed] [Google Scholar]
- 29.Farhi D. Yoga mind, body & spirit: a return to wholeness. 1. New York, New York: Holt Paperbacks and Henry Holt and Company, LLC; 2000. [Google Scholar]
- 30.Fried R, Grimaldi J. The Psychology and Physiology of Breathing: In Behavioral Medicine, Clinical Psychology and Psychiatry. New York, New York: Plenum Press; 1993. [Google Scholar]
- 31.Cohen BE, Kanaya AM, Macer JL, Shen H, Chang AA, Grady D. Feasibility and acceptability of restorative yoga for treatment of hot flushes: a pilot trial. Maturitas. 2007;2:198–204. doi: 10.1016/j.maturitas.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 32.Booth-LaForce C, Thurston RC, Taylor MR. A pilot study of a Hatha yoga treatment for menopausal symptoms. Maturitas. 2007;3:286–95. doi: 10.1016/j.maturitas.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 33.Chattha R, Raghuram N, Venkatram P, Hongasandra NR. Treating the climacteric symptoms in Indian women with an integrated approach to yoga therapy: a randomized control study. Menopause. 2008;5:862–70. doi: 10.1097/gme.0b013e318167b902. [DOI] [PubMed] [Google Scholar]
- 34.Joshi S, Khandwe R, Bapat D, Deshmukh U. Effect of yoga on menopausal symptoms. Menopause Int. 2011;3:78–81. doi: 10.1258/mi.2011.011020. [DOI] [PubMed] [Google Scholar]
- 35.Elavsky S, McAuley E. Physical activity and mental health outcomes during menopause: a randomized controlled trial. Ann Behav Med. 2007;2:132–42. doi: 10.1007/BF02879894. [DOI] [PubMed] [Google Scholar]
- 36.Carson JW, Carson KM, Porter LS, Keefe FJ, Seewaldt VL. Yoga of Awareness program for menopausal symptoms in breast cancer survivors: results from a randomized trial. Support Care Cancer. 2009;10:1301–9. doi: 10.1007/s00520-009-0587-5. [DOI] [PubMed] [Google Scholar]
- 37.Sloan JA, Loprinzi CL, Novotny PJ, Barton DL, Lavasseur BI, Windschitl H. Methodologic lessons learned from hot flash studies. J Clin Oncol. 2001;23:4280–90. doi: 10.1200/JCO.2001.19.23.4280. [DOI] [PubMed] [Google Scholar]
- 38.Soules MR, Sherman S, Parrott E, et al. Executive summary: Stages of reproductive aging workshop (STRAW) Fertil Steril. 2001:874–8. doi: 10.1016/s0015-0282(01)02909-0. [DOI] [PubMed] [Google Scholar]
- 39.Satchidananda YSS. Integral Yoga Hatha. Buckingham, Virginia: Integral Yoga Publications; 1970. [Google Scholar]
- 40.Avis NE, Legault C, Coeytaux RR, et al. A randomized, controlled pilot study of acupuncture treatment for menopausal hot flashes. Menopause. 2008;6:1070–8. doi: 10.1097/gme.0b013e31816d5b03. [DOI] [PubMed] [Google Scholar]
- 41.Carpenter JS. The Hot Flash Related Daily Interference Scale: a tool for assessing the impact of hot flashes on quality of life following breast cancer. J Pain Symptom Manage. 2001;6:979–89. doi: 10.1016/s0885-3924(01)00353-0. [DOI] [PubMed] [Google Scholar]
- 42.Owens JF, Matthews KA. Sleep disturbance in healthy middle-aged women. Maturitas. 1998;1:41–50. doi: 10.1016/s0378-5122(98)00039-5. [DOI] [PubMed] [Google Scholar]
- 43.Buysse DJ, Reynolds CF, III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;2:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 44.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) Am J Prev Med. 1994;2:77–84. [PubMed] [Google Scholar]
- 45.Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL): a self-report symptom inventory. Behav Sci. 1974;1:1–15. doi: 10.1002/bs.3830190102. [DOI] [PubMed] [Google Scholar]
- 46.Winokur A, Winokur DF, Rickels K, Cox DS. Symptoms of emotional distress in a family planning service: stability over a four-week period. Br J Psychiatry. 1984:395–9. doi: 10.1192/bjp.144.4.395. [DOI] [PubMed] [Google Scholar]
- 47.Shantha S, Brooks-Gunn J, Locke RJ, Warren MP. Natural vaginal progesterone is associated with minimal psychological side effects: a preliminary study. J Womens Health Gend Based Med. 2001;10:991–7. doi: 10.1089/152460901317193567. [DOI] [PubMed] [Google Scholar]
- 48.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;4:385–96. [PubMed] [Google Scholar]
- 49.Cohen S, Williamson GM. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The social psychology of health. Newbury Park, CA: Sage; 1988. [Google Scholar]
- 50.Ware JE, Jr, Sherbourne CD. The MOS 36-item short form health survey (SF-36): I. Conceptual framework and item selection. Med Care. 1992:473–83. [PubMed] [Google Scholar]
- 51.Jennrich RI, Schluchter MD. Unbalanced repeated-measures models with structured covariance matrices. Biometrics. 1986;4:805–20. [PubMed] [Google Scholar]
- 52.Laird NM, Ware JH. Random-effects models for longitudinal data. Biometrics. 1982;4:963–74. [PubMed] [Google Scholar]
- 53.Browne RP, Gerbarg PL. Sudarshan Kriya yogic breathing in the treatment of stress, anxiety, and depression: part I-neurophysiologic model. J Altern Complement Med. 2005;11:189–201. doi: 10.1089/acm.2005.11.189. [DOI] [PubMed] [Google Scholar]
- 54.Freedman RR. Pathophysiology and treatment of menopausal hot flashes. Semin Reprod Med. 2005;23:117–125. doi: 10.1055/s-2005-869479. [DOI] [PubMed] [Google Scholar]