Abstract
In response to health problems, individuals may strategically activate their social network ties to help manage crisis and uncertainty. While it is well-established that social relationships provide a crucial safety net, little is known about who is chosen to help during an episode of illness. Guided by the Network Episode Model, two aspects of consulting others in the face of mental illness are considered. First, we ask who activates ties, and what kinds of ties and networks they attempt to leverage for discussing health matters. Second, we ask about the utility of activating health-focused network ties. Specifically, we examine the consequences of network activation at time of entry into treatment for individuals' quality of life, social satisfaction, ability to perform social roles, and mental health functioning nearly one year later. Using interview data from the longitudinal Indianapolis Network Mental Health Study (INMHS, N = 171), we focus on a sample of new patients with serious mental illness and a group with less severe disorders who are experiencing their first contact with the mental health treatment system. Three findings stand out. First, our results reveal the nature of agency in illness response. Whether under a rational choice or habitus logic, individuals appear to evaluate support needs, identifying the best possible matches among a larger group of potential health discussants. These include members of the core network and those with prior mental health experiences. Second, selective activation processes have implications for recovery. Those who secure adequate network resources report better outcomes than those who injudiciously activate network ties. Individuals who activate weaker relationships and those who are unsupportive of medical care experience poorer functioning, limited success in fulfilling social roles, and lower social satisfaction and quality of life later on. Third, the evidence suggests that social networks matter above and beyond the influence of any particular individual or relationship. People whose networks can be characterized as having a pro-medical culture report better recovery outcomes.
Keywords: Network Episode Model, Habitus, Help-seeking, Social support, Egocentric social networks, Psychiatric disorder, Mental illness
Introduction
Research and theory on social relationships, whether network structures or social support, stand among the strongest social science contributions to the understanding of the distribution, experience, and outcomes of illness (House, Landis, & Umberson, 1988; Pescosolido & Levy, 2002; Smith & Christakis, 2008). In this literature, social interaction is framed, often implicitly, as a central mechanism linking social networks and health. Resources critical for preventing or recovering from illness flow through health discussion networks: advice, information, emotional support, affirmation and belonging, and attitudes about how to define and respond to health problems (Abbott, Bettger, Hanlon, & Hirschman, 2012; Schafer, 2013). Yet, the utility of social network resources depends on successful activation of ties that can provide access to relevant information or support (Lin, 1999). Consequently, who is mobilized through tie activation (i.e. communications about support needs, beliefs and behaviors, and decision-making) represents a critical moment in response to life's challenges (Hurlbert, Haines, & Beggs, 2000; Perry & Pescosolido, 2010; Pescosolido, 1992).
However, we know relatively little about which individuals are included in discussion networks and whether the profile of activated ties affects outcomes. Here, we address these gaps, focusing on social network activation in the early illness career. The Network Episode Model (Pescosolido,1991,1992,2006; Pescosolido, Brooks-Gardner, & Lubell, 1998) provides the theoretical platform to develop research questions about tie activation and health outcomes. The Indianapolis Network Mental Health Study provides the necessary longitudinal and hierarchical data to empirically examine them. We ask (1) how do characteristics of individuals, relationships, and networks shape which ties are activated during the early stages of an illness episode? And (2) do the properties of ties activated at the point of initial entry into treatment influence recovery outcomes nearly one year later?
Theoretical background
Social networks and the response to illness onset
While the contention that “others” form a critical part of how individuals understand and respond to illness represents an early line of inquiry in social science (e.g., Friedson, 1970, Kadushin, 1966), the Network Episode Model (NEM) explicitly theorized the role of social networks. In contrast to more static and individualistic models, the NEM sees health and illness behaviors as an embedded social process that creates an illness career. This dynamic conceptualization reflects the variety of fluid pathways that individuals and their social networks follow in response to illness (Pescosolido et al., 1998). Under these basic assumptions informal (i.e., personal or lay) and formal (i.e., professional) social networks are activated because health problems, particularly as they are more severe, exceed individuals' personal capacity for coping (Bury, 1982; Carpentier, Lesage, & White, 1999; Wellman, 2000).
Tie activation is not necessarily a rational decision-making process. Rather, the culture of a network provides the context for activation, and the beliefs, values, and attitudes flowing through networks can either facilitate or inhibit health discussion. Contemporary work in medical sociology has increasingly incorporated cultural theory, emphasizing the importance of cultural capital and habitus in health behaviors and decision-making (Bourdieu, 1984; Kleinman, 2004; Nichter, 2008; Singh-Manoux & Marmot, 2005). At the same time, there has been growing recognition of the link between social networks and culture, meaning, and social reproduction (Emirbayer & Goodwin, 1994; Lizardo, 2006; Pachucki & Breiger, 2010).
Networks may be conduits of health-related cultural capital, including the ability to identify symptoms of illness, recognize a need for formal and informal support, and help secure access to health and social services. Networks that possess these types of health capital are probably more likely to be activated for medical advice and health discussion than those perceived as unknowledgeable or unhelpful. Likewise, individuals develop a health habitus – or an orientation toward illness, help-seeking, medical professionals, and health services – through socialization and interaction with social networks (Lo & Stacey, 2008). The degree to which a person activates both informal and formal support in response to illness onset is probably determined in part by this habitus, which shapes unconscious beliefs about courses of action that are possible and appropriate. Thus, tie activation reflects individual agency operating within the constraints of habitus, network culture, and accessible resources.
Whether done as a rational choice, as a pathway of coercion or resistance, or even in a haphazard fashion (Pescosolido et al., 1998), the linked process of tie activation represents a strategy for coping with crisis. That is, as individuals face unfamiliar challenges, periods of elevated support needs, and fundamental disruptions of identity and role performance that accompany illness, social networks become critical (Abbott et al., 2012; Lively & Smith, 2011). Individuals manage, or are managed, through health problems by lay and professional network ties who may recognize, define, or dismiss symptoms; recommend or provide health services; offer emotional or instrumental support; or attempt to regulate health behaviors, appointments, and medication compliance.
In the NEM, these interactions are theorized to have consequences – both good and bad. Social networks and illness careers form mutually dependent and reflexive pathways. Illness episodes influence social network dynamics, shaping the structure, function, and content of personal and professional communities over time. In turn, health problems are defined and treatment decisions are made in and with activated networks, influencing the trajectory of the illness career. Health discussion networks may or may not transmit pro-health care attitudes, provide information about how to obtain services, and improve access to services by helping initiate contact with the treatment system. In some cases, attempts to activate network members through discussion of mental health experiences or requests for support may be met with rejection or indifference. Further, disclosing health problems to others who are empathetic and supportive can provide emotional and instrumental supports or can elicit stigmatizing reactions, particularly in mental illness (Link, Mirotznik, & Cullen, 1991; Pescosolido et al., 2010; Wahl, 2012). The response of activated networks in the face of illness is hypothesized to have an important influence on recovery, and empirical research has provided reasonable evidence to support this link (Gallant, 2003; Pescosolido et al., 1998; Thoits, 2011).
Shopping network boutiques: tie activation for mental health problems
The functional specificity hypothesis (Cutrona & Russell, 1990; Penning, 1990; Simons, 1983–1984) posits that individuals engage in goal-directed social interaction to access different types of social resources through personal community networks. According to Wellman and Wortley (1990), most of our social ties are “boutiques” rather than “general stores,” and whether consciously or not we “shop” to obtain goods and services that we need. In other words, people tend to activate a given tie for only one or a few specialized functions rather than relying on one person to fulfill all support needs. A particular type of relationship or person may be effective for one kind of task or problem, but not another (Sandefur & Laumann, 1998).
In short, the functional specificity hypothesis emphasizes the fit between the problem or support need at hand and the skills, information, resources, and accessibility of individual ties embedded within network structures and cultures (Karp, 2001; Perry, 2012; Pescosolido et al., 1998). People can selectively draw on their diverse network resources, activating ties that are most likely to be useful for a particular purpose (Hurlbert et al., 2000; Perry & Pescosolido, 2012; Wellman & Wortley, 1990). This selective activation of ties during an acute health crisis represents a potentially influential but largely overlooked coping mechanism (Pescosolido, 1991, 1992; Wellman, 2000; Wellman & Wortley, 1989). Only very recently have targeted discussions on topics such as health services utilization, compliance, behaviors, and beliefs been linked empirically to health outcomes (Abbott et al., 2012; Perry & Pescosolido, 2010; Schafer, 2013; York Cornwell & Waite, 2012). Yet, the extent to which individuals with health problems are able to secure access – through activation of certain ties but not others – to information, treatment options, or support that facilitate recovery may, in part, explain why social network characteristics matter for wellbeing.
In the case of mental illness in particular, onset is characterized by acute crisis and many serious problems and stressful events which may be more or less controllable (e.g., contacts with law enforcement, medication side effects, stigma; Carpentier et al., 1999; Sharfstein, 2009). Consequently, the onset of serious mental illness has been said to initiate a “network crisis” (Lipton, Cohen, Fischer, & Katz, 1981), or a period of rapid change in the structure and function of social networks as loved ones respond to elevated support needs (Perry & Pescosolido, 2012). During this time, the ability to activate skillful health discussants may be particularly critical. The largest benefits appear to accrue in situations where an individual is able to mobilize network resources that match the challenges they face (Cutrona & Russell, 1990; Horowitz et al., 2001; Krause, 1997). Key supporters of people with mental illness are heavily involved early in the illness career, brokering health services, negotiating treatment options, and acting as health advocates (Muhlbauer, 2002). In addition to facilitating successful navigation of the treatment system, effective first responders play a critical role in diffusing the most threatening and immediate problems (Carpentier et al. 1999). During this time, members of the network must often provide the kinds of assistance they would not typically offer (e.g. financial support, help with daily living, medication reminders, a safe place to stay, etc.; Pescosolido et al. 1998).
The concept of the sick role offers a structural functionalist perspective on network activation and response during illness (Parsons, 1951). When the social safety net is activated by a person experiencing a health crisis, the behavior of potential supporters is governed by a set of social roles and a sense of obligation, particularly for family members (Perry, 2011; Wellman, 2000). The normative response is to provide the needed emotional or instrumental support. Empirical research suggests that the social networks of people with mental illness are large, highly supportive, and very involved, particularly early in the illness career (Carpentier & Ducharme, 2005; Perry & Pescosolido, 2012; Salokangas, 1997). Long-standing ties based on a shared history and mutual feelings of obligation and affection are ideal candidates for activation, and these are the people most likely to come to the aid of an ill loved one (Cook, 1988; Wellman, 2000). Additionally, people may be motived to help sick individuals obtain formal support, remain in treatment, and reenter social roles because progress toward recovery reduces the burden of caregiving (Ware et al., 2009). In short, close friends and family members are both motivated and obligated to respond to support activation during a mental health crisis, even when their efforts are unreciprocated or burdensome (Carpentier & Ducharme, 2003; Wellman, 2000).
Though activating social ties is a primary strategy for coping with an episode of mental illness, social networks have a dark side; they engender costs. Because reciprocity norms guide resource exchange in most relationships, attempts to secure support elicit an implicit obligation to return the favor (Fehr, Fischbacher, & Gächter, 2002). Further, support provided may be unhelpful, sometimes exacerbating negative emotions and relationship dissatisfaction (Bolger, Zuckerman, & Kessler, 2000; Krause, 1997; Rafaeli & Gleason, 2009). Even as perceived support availability is found to be beneficial, actual exchanges often exhibit negligible, or even detrimental, effects, provoking feelings of inadequacy or dependence (Fisher, Nadler, & Whitcher-Alagna, 1982; Rafaeli & Gleason, 2009). Moreover, the types of exchanges that typically result from network activation for health discussion – advice giving, identification with feelings, and encouragement or optimism – are also sometimes the least effective at producing positive outcomes (Barbee, Derlega, Sherburne, & Grimshaw, 1998; Lehman, Ellard, & Wortman, 1986).
For those with stigmatized illness, network activation has greater costs. People with mental illness who discuss these problems with others often confront negative attitudes such as the attribution of illness to character flaws (Wahl, 2000). Likewise, the intelligence, abilities, emotions, and opinions of people with mental illness are frequently questioned, and their independence and self-sufficiency may be undermined by others' attempts to protect them from stress. Such experiences have long-term effects, including low self-esteem, social isolation, disclosure anxiety, and symptoms like depression and distrust which prolong recovery (Link et al., 1991; Wahl, 2012).
Because the stakes are high, particularly for those with mental health problems, navigating the social terrain of the illness experience is critical (Pescosolido, 1991; Pescosolido et al. 1998). Individuals with mental illness are sensitive to the potential social consequences of making excessive requests for support and highly responsive to others' perceptions (Link, Cullen, Struening, Shrout, & Dohrenwend, 1989; Perry, 2012). To manage stigma, interaction strategies such as secrecy, withdrawal, and education are employed (Link, 1987; Link et al. 1989). This may result in selective or preemptive disclosure, perhaps eliciting health discussion with ties perceived to be sympathetic, who have particular attitudes toward mental health issues, or have experience with mental illness (Wahl, 2012).
In sum, the NEM and associated network theory leads us to propose a clear mechanism of tie activation and network influence — health discussion. We conceptualize activation as a multilevel phenomenon, mirroring the nested structure of individuals, ties, and networks as they function in the social world. Moreover, we focus on both the origins and consequences of tie activation, reflecting the dynamic and fluid nature of the illness career as theorized by the NEM. Thus, two research questions form the basis of an empirical analysis: First, how do characteristics of individuals, relationships, and networks shape the activation of ties during the early stages of an acute episode of illness? Second, how do properties of activated networks at the point of initial entry into treatment influence recovery outcomes nearly one year later?
Data and methods
Sample
The Indianapolis Network Mental Health Study (INMHS) employed an egocentric social network design to identify relationships between the early illness career and social network dynamics. The study was conducted at two large public and private hospitals (including an embedded community mental health center). All new clients making their first major contact with the mental health system and with a mental health history of no more than two years were contacted and asked to participate in face-to-face interviews (66.4% consented). Both of these inclusion criteria were assessed using self-report. Participants were administered the Structured Clinical Interview for DSM-III-R (Spitzer, Williams, Gibbon, & First, 1990) and recruited if a major Axis I research diagnosis was identified (schizophrenia, bipolar disorder, or major depression). A comparison sample with less serious mental illness (largely adjustment disorder) was also recruited simultaneously. Recruitment was conducted through emergency rooms and crisis centers. Some respondents were subsequently hospitalized, but the majority was referred for outpatient treatment. None of the respondents were exclusively diagnosed with substance abuse or dependence. Fielded from 1990 to 1997 to recruit a sufficient number of “first timers,” the INMHS remains one of the most detailed longitudinal, network-based studies in the health arena, including both egos and their alters elicited using nearly a dozen network batteries across life domains. Additional information can be obtained at http://www.indiana.edu/∼icmhsr/inmhs.html.
A total of 173 individuals participated in the first round of face-to-face interviews, conducted within three months of treatment initiation. Due to missing data across waves, the effective sample size is 171 at Time 1 and 108 at Time 2 (about 10 months later, on average). Respondents reported information about 2593 network members.
Measures
Name generators
As noted above, the INMHS includes data on respondents' associates across a broad range of domains: household, family, romantic partnerships, work and school ties, friends, acquaintances, people with common problems, and treatment providers. Each domain has a corresponding name generator, with no limitations on the number or types of people respondents could name. This approach provides a near inventory of people who have contact with respondents (“total network”), including ties of great significance (e.g., core supporters) as well as those who may play a more peripheral or unidimensional role (e.g., treatment providers, neighbors, etc.).
Activation for health discussion is measured using data from a name generator that is a targeted variant of the “important matters” General Social Survey question (Marsden, 1987). The “health matters” name generator is located about two-thirds of the way through the interview. It reads: “I'm interested in who, among all of the people in your life, you talk to about health problems when they come up. Who are the people that you discuss your health with or you can really count on when you have physical or emotional problems?” Respondents were notified that they could list people who had already been named previously or could provide new names. During the interview, names of network members were checked against those provided in response to previous name generators. Alters were given unique identification numbers, and this process was verified by respondents. Some overlap between different network domains is observed, as has been documented previously (Perry & Pescosolido, 2010). These network ties are referred to here as “health discussants.”
To capture the complexity of individuals, ties, and networks, variables are measured at two distinct analytic levels and four conceptual levels. Characteristics of ego (i.e. the focal person at the center of the network analysis) and aggregated characteristics of ego's social networks constitute Level 2, consistent with previous research on egocentric networks analyzed using multilevel modeling (de Miguel Luken & Tranmer, 2010; Snijders, Spreen, & Zwaagstra, 1995). Characteristics of alters (i.e. network members named by ego) and ties (i.e. relationships between ego and alter) constitute Level 1. Unless otherwise noted, measures were developed for the Indianapolis Network Mental Health Study by members of the research team.
Level-2 variables: egos and networks
Because socio-demographic characteristics of respondents like gender, race, age, and educational attainment shape the structure and function of personal community networks (Ajrouch, Antonucci, & Janevic, 2001; Marsden, 1987; Peek & O'Neill, 2001), these variables are considered as controls in regression analyses. Gender (1 = female; 0 = male) and race (1 = white, 0 = black) are coded into dummy variables. Mental illness diagnosis is coded into three dichotomous indicators representing depression (unipolar or bipolar), schizophrenia, schizoaffective disorder, or Psychosis NOS, and a group of less severe other disorders comprised largely of respondents with adjustment disorder. Number of psychiatric symptoms was assessed using the diagnostic instrument (i.e. SCID). Respondents were asked about a large number of symptoms across multiple diagnostic categories. Reported symptoms are summed to provide a continuous (as opposed to dichotomous) measure of psychiatric impairment. Other controls were included in initial models (i.e. education and age), but these were removed from final models due to non-significance and having no influence on key social network variables.
Measures of “total network” characteristics, examined at Level 2, are network size (total number of alters listed by ego), percent women, and percent kin (by marriage or blood). Average closeness is the mean of reported closeness (higher = closer) to each alter aggregated across the total network (response categories: “not very close,” “sort of close,” “very close”). Average network trust in physicians is the mean of each alter's reported trust in physicians (higher = more trust) aggregated across the total network (response categories: “not very much,” “most of the time,” “a lot,” “unsure” with the latter coded to missing).
Measures of the size of the health discussion network, mean closeness, and mean trust in physicians are coded identically to those above except that only network ties activated for health discussion are included in calculations. Identical measures are also created for the network of ties not activated for health discussion to compare the effects of activated and inactivated networks on outcomes.
Four Level-2 dependent variables are indicators of overall functioning and wellbeing. A quality of life scale (8 items; higher = more satisfied) is adapted from Bond's Life Satisfaction Checklist, which has shown high internal reliability and convergent validity (Bond et al., 1990). It asks respondents to rate satisfaction with various aspects of their life (financial situation, housing, family and friend relationships, employment situation, recreational activities, general health, and overall life). Responses are “good,” “fair,” and “poor.” The scale score is the mean of all non-missing items (alpha = 0.74). A social satisfaction scale (15 items; higher = more satisfied) measures satisfaction with social relationships, including family, neighbors, coworkers, fellow students, fellow volunteers, other people, friends, and people at church. Responses are measured on a Delightful—Terrible scale ranging from 1 to 5 with a scale score being the mean of all non-missing items (alpha = 0.84). The measure of satisfaction in the social life domain has been used previously in social science research (Michalos, 1985) and has been validated in a number of samples, including people with mental illness (Lehman, 1988).
Perceived success at performing social roles is also a scale (25 items) asking “how good or successful” the respondent is at being (social role), including family roles (e.g. parent, son/daughter, sibling), work and volunteer roles, friend, neighbor, and church member, etc. Responses range from “poor” to “good” (higher = more success) with a scale score being the mean of all non-missing items (alpha = 0.81). Finally, Global Assessment of Functioning (GAF) is included as an indicator of respondents' overall psychological health where interviewers with minimal training subjectively but reliably rate the social, occupational, and psychological functioning of people with mental illness (Startup, Jackson, & Bendix, 2002). It ranges from 0 to 100 (higher = better functioning).
Level-1 variables: alters and ties
Characteristics of alters and ties (Level 1) include gender (1 = female; 0 = male) and age in years. Three variables measure orientation to health/health care. Having a common emotional or mental health problem (i.e., experiential homophily, or the tendency to interact with others who have had similar experiences) is a dummy variable (1 = yes; 0 = no). Trust in physicians is a dichotomous variable (1 = a lot; 0 = most of the time or not very much). The latter two categories are combined because initial analyses indicated no distinct effects on the dependent variable. Finally, respondents were asked to name alters who had suggested they seek mental health treatment (1 = yes; 0 = no).
Tie characteristics include the nature of the relationship between ego and alter measured using a series of dichotomous indicators representing partner/spouse, parent, sibling, child, friend, coworker, neighbor, medical or mental health professional, or another type of relationship. Relationship closeness, as above, is dichotomized (1 = very close; 0 = sort of close or not very close). Frequency of verbal or face-to-face contact is also dichotomized (1 = often; 0 = occasionally or hardly ever). Relationship conflict is measured by asking how often the person hassles the respondent, causes problems, or makes life difficult (1 = a lot; 0 = sometimes or not really). The latter three variables are dichotomized with the lower two categories collapsed for ease of interpretation since initial analyses found no significant difference on the overall findings.
Network activation is the dichotomous Level-1 dependent variable in the multilevel model. As described above, egos named alters they talked to/could depend on regarding health problems. If an alter is listed, they are coded 1, otherwise 0.
Analysis
We proceed in two steps. The first identifies characteristics of egos, alters, ties, and networks that are associated with activation of alters for health discussion. Multilevel regression modeling uses data on respondents (egos) and alters at Time 1 – the point of entry into mental health treatment. Specifically, a random-intercept model is used with Level-1 alters nested in Level-2 egos. These models include a random intercept for each ego and adjust for the lack of independence between observations for nominated alters. Because in egocentric network research we are typically interested in the population of clusters (egos) rather than the population of observations (alters) controlling for clusters, random-intercept models are a better fit than fixed effects models. Also, unlike fixed effects models, random-intercept models permit estimation of ego, alter, tie, and network-level effects.1 The two-level binary logistic regression model predicting probability p of ego j activating a tie with alter i is written as:
In this model, i corresponds to alter (i.e. Level 1) identifier, j to respondent (i.e. Level 2) identifier, ζj to the random intercept, and εij to the Level-1 residual. Together, ζj and εij represent random parts of the model, while the other components are fixed.
This analytic strategy is ideal in cases where the dependent variable is a characteristic of alters or ties since aggregation to the ego level results in a loss of information. Because variables at the levels of ego, alter, and network are correlated, groups of related variables are added in a stepwise fashion to a series of separate regression models. All models control for ego demographics and illness characteristics. Odds ratios and confidence intervals are presented.
The aim of the second analytic component is to determine how characteristics of the activated health discussion network and the inactivated network at Time 1 (point of entry into treatment) are related to a variety of indicators of health, social functioning, and wellbeing at Time 2. These two waves of data are used because we are interested in examining the proximate effects on recovery (i.e. Time 2) of social network processes that occur in response to a health crisis (i.e. Time 1), when support needs are likely to be most pronounced. This analysis uses a subsample of respondents present in two waves of the study and with at least one health discussion partner. Comparisons of cases retained and those dropped due to missing data or no health discussants were conducted to assess potential biases associated with this strategy. These suggest that there are significant differences only with regard to gender (p < .05) and size of the inactivated network (p < .001). The latter is expected since activating at least one network member for health discussion is a criterion for inclusion. With regard to gender, 54% of excluded cases are female compared to 69% of included cases.
Since the aim is to predict the effects of social network characteristics on egos' outcomes, multilevel modeling is not appropriate. Instead, characteristics of alters are aggregated to the network level and analyzed as properties of egos. OLS regression is used to model the effects of three characteristics of the health discussion network and the network not activated for health discussion, plus a set of ego-level control variables (demographics and illness characteristics) on four scales. These network characteristics were chosen from among multiple available measures because they are commonly used in egocentric network research and produce the best model fit. Including other network variables (e.g., homophily, density, gender composition, etc.) does not substantially alter the results or the conclusions drawn from them. For the sake of parsimony, the simplest models are presented. The model predicting outcome y at Time 2 using network properties at Time 1 can be written as follows:
Models controlling for levels of y at Time 1are also performed to provide a conservative test of causal direction. Because this strategy results in autocorrelation and inflated R2 statistics, models without controls for prior values of y are also presented. The model predicting outcome y at Time 2 using network properties at Time 1 and controlling for values of y at Time 1 can be written as:
The dependent variables are relatively normally distributed, making OLS regression an appropriate estimation procedure. Variance inflation factors and Cook–Weisberg tests indicate that levels of multicollinearity and heteroskedasticity are unproblematic, with one exception. The model predicting GAF is heteroskedastic and this is corrected using the robust estimator of variance. Unstandardized coefficients and standard errors are presented. To convey the magnitude of these effects, a selection of significant findings is presented in figures of standardized predicted values in addition to tables and text.
Results
Table 1 indicates that 64% of respondents in the full sample are female; 73% are white and 27% are black. Respondents range in age from 16 to 72 (mean = 30.6 years) with average education at 11.6 years. About 59% of respondents are diagnosed with depression (unipolar or bipolar), 13% with schizophrenia, schizoaffective disorder or similar, and 28% with less severe disorders (largely adjustment disorder). Mean number of psychiatric symptoms is 4.43. Though not shown in Table 1, most lived and worked independently (e.g., 86% lived either alone, with a spouse or partner, or with a roommate; 78% were currently working, full-time students, or keeping house; details on request).
Table 1.
Sample descriptive statisticsa, INMHS.
| n | Prop | Mean | SD | Range | ||
|---|---|---|---|---|---|---|
| Panel A: full sampleb | ||||||
| Egos (n = 171) | ||||||
| Gender (1 = female) | 109 | 0.64 | ||||
| Age (years) | 30.56 | 10.17 | 18.00–72.00 | |||
| Race (1 = white) | 125 | 0.73 | ||||
| Education (years) | 11.59 | 2.00 | 6.00–16.00 | |||
| Diagnosisc | ||||||
| Schizophrenia | 22 | 0.13 | ||||
| Depression | 101 | 0.59 | ||||
| # Of psychiatric symptoms | 4.43 | 2.09 | 0.00–12.00 | |||
| Alters and ties (n = 2593) | ||||||
| Gender (1 = female) | 0.56 | |||||
| Age (ten years) | 34.79 | 16.18 | 1–96 | |||
| Common mental health problem | 0.06 | |||||
| High trust in physicians (a lot) | 0.12 | |||||
| Suggested MH services | 0.05 | |||||
| Relationshipc | ||||||
| Kin | 0.55 | |||||
| Friend | 0.21 | |||||
| Medical/MH prof | 0.10 | |||||
| Very close | 0.43 | |||||
| Frequent contact (often) | 0.50 | |||||
| Hassles or causes problems | 0.11 | |||||
| Alter activated as discussant | 0.20 | |||||
| Whole networks (n = 171) | ||||||
| Network size | 15.50 | 6.20 | 5.00–37.00 | |||
| % Women | 55.15 | 14.30 | 16.67–91.67 | |||
| % Kin | 56.06 | 17.15 | 21.74–100.00 | |||
| Mean closeness | 2.20 | 0.35 | 1.33–3.00 | |||
| Mean trust in physicians | 2.26 | 0.42 | 1.00–3.00 | |||
| Panel B: Subsampleb | ||||||
| Egos (n = 108) | ||||||
| Gender (1 = female) | 75 | 0.69 | ||||
| Race (1 = white) | 81 | 0.75 | ||||
| Diagnosisc | ||||||
| Schizophrenia | 10 | 0.09 | ||||
| Depression | 67 | 0.62 | ||||
| Quality of lifed (scale) | 2.25 | 0.47 | 1.13–3.00 | |||
| Social satisfactiond (scale) | 3.52 | 0.70 | 1.50–5.00 | |||
| Social role performanced (scale) | 3.88 | 0.59 | 2.00–4.93 | |||
| GAFd (scale) | 66.22 | 14.51 | 18.00–98.00 | |||
| Health discussion networks | ||||||
| Network size | 3.59 | 2.16 | 1.00–10.00 | |||
| Mean closeness | 2.64 | 0.44 | 1.00–3.00 | |||
| Mean trust in physicians | 2.38 | 0.51 | 1.00–3.00 | |||
| Inactivated networks | ||||||
| Network size | 12.40 | 5.76 | 2.00–30.00 | |||
| Mean closeness | 2.08 | 0.37 | 1.17–3.00 | |||
| Mean trust in physicians | 2.28 | 0.41 | 1.00–3.00 | |||
Subsample includes those with ≥1 health discussant who are present in two waves. Dropped cases differ significantly only with respect to gender and size of the inactivated network.
Omitted category is other.
Outcomes measured at T2, all other variables at T1.
Also shown in Table 1, the size of the total network of regular interaction partners is about 15.50, on average. Slightly more than half of egos' total networks are comprised of women and kin. Mean closeness is moderate (2.20 on a 3-point scale), on average, suggesting a tendency to nominate both stronger and weaker ties. Mean trust in physicians is moderately high (2.23 on a 3-point scale), reflecting in part the inclusion of some treatment providers. Ego respondents talk to about three people, on average, about their health problems. This network is comprised of very close ties (mean = 2.64) with moderately high trust in physicians (mean = 2.34).
With respect to alter characteristics, 6% have mental health problems in common with respondents, 12% have high trust in physicians, and 5% suggested treatment as a solution to mental health problems. About half of total networks are comprised of family members, 21% are friends and 10% are medical or mental health professionals. About 43% of ties are very close, on average, and 50% are in frequent contact. Overall, only 20% of the entire set of social network ties is activated specifically for health discussion and advice, suggesting that respondents are selective in whom they to talk to regarding health matters.
Who is activated?
As shown in Model 1 of Table 2, two ego characteristics significantly affect propensity to activate alters for health discussion. Each additional ten years of age is associated with a 15% increase in the odds of activating any given tie for health discussion (p < .05). Higher levels of psychiatric symptoms are also associated with increasing odds of activation of health discussion networks (OR = 1.09, p < .05). Model 2 demonstrates that alter characteristics also influence activation for health discussion. Alter age is positively related to the odds of activation (OR = 1.24, p < .001). Experiential homophily also shapes tie activation. Alters who have had a mental illness are over two and a half times more likely to be sought out for health discussion relative to those without similar experiences (p < .001). Finally, people who initially suggested that ego should seek medical or mental health treatment are over six times as likely as those who did not to be approached for help with health problems following entry into treatment (p < .001).
Table 2.
Random-intercept logistic regression of activation for health discussion on characteristics of egos, alters, and ties (n = 2593).
| 1 | 2 | 3 | 4 | |
|---|---|---|---|---|
|
|
|
|
|
|
| OR (CI) | OR (CI) | OR (CI) | OR (CI) | |
| Egos | ||||
| Gender (1 = female) | 1.05 (0.77–1.42) | 0.92 (0.66–1.28) | 0.89 (0.58–1.38) | 0.96 (0.68–1.35) |
| Age (ten years) | 1.15 (1.01–1.31)* | 1.07 (0.92–1.24) | 1.31 (1.08–1.59)** | 1.14 (0.99–1.31) |
| Race (1 = white) | 0.88 (0.64–1.21) | 0.78 (0.55–1.10) | 1.11 (0.70–1.75) | 1.09 (0.76–1.56) |
| Education (years) | 1.00 (0.93–1.07) | 1.00 (0.93–1.08) | 1.06 (0.96–1.16) | 1.03 (0.95–1.10) |
| Diagnosisa | ||||
| Schizophrenia | 0.95 (0.57–1.58) | 0.89 (0.51–1.54) | 1.31 (0.64–2.67) | 0.93 (0.54–1.60) |
| Depression | 0.87 (0.60–1.24) | 0.85 (0.58–1.26) | 1.02 (0.61–1.70) | 0.89 (0.61–1.30) |
| # Of psychiatric symptoms | 1.09 (1.01–1.17)* | 1.11 (1.02–1.21)* | 1.07 (0.97–1.19) | 1.09 (1.01–1.17)* |
| Alters | ||||
| Gender (1 = female) | 1.23 (0.98–1.53) | 1.27 (1.01–1.59)* | ||
| Age (ten years) | 1.24 (1.15–1.32)*** | |||
| Common MH problem (1 = yes) | 2.52 (1.74–3.67)*** | |||
| Trust in physicians (1 = a lot) | 0.95 (0.68–1.34) | 0.95 (0.67–1.35) | ||
| Suggested MH services (1 = yes) | 6.57 (4.42–9.78)*** | |||
| Ties | ||||
| Relationship (1 = yes)b | ||||
| Partner | 6.58 (3.61–11.98)*** | |||
| Mother | 5.51 (3.27–9.30)*** | |||
| Father | 1.08 (0.53–2.20) | |||
| Sibling | 0.91 (0.59–1.40) | |||
| Child | 0.16 (0.09–0.29)*** | |||
| Co-worker | 0.45 (0.25–0.80)*** | |||
| Neighbor | 0.51 (0.19–1.40) | |||
| Medical or MH prof | 1.86 (1.09–3.20)* | |||
| Other relationship | 0.17 (0.09–0.30)*** | |||
| Kin (1 = yes) | 1.08 (0.86–1.37) | |||
| Closeness (1 = very) | 5.39 (3.88–7.50)*** | 5.17 (4.03–6.63)*** | ||
| Frequency of contact (1 = often) | 2.56 (1.86–3.52)*** | |||
| Hassles/problems (1 = a lot) | 0.38 (0.21–0.68)*** | |||
| Whole networksc | ||||
| Network size | 0.96 (0.94–0.98)*** | |||
| Percent women (tens) | 1.03 (0.92–1.16) | |||
| Percent kin (tens) | 0.94 (0.86–1.03) | |||
| Mean closeness | 0.79 (0.49–1.27) | |||
| Mean trust in physicians | 1.64 (1.03–2.60)* | |||
| Wald Xb | 8.79 | 162.34*** | 287.71*** | 206.39*** |
| ρ | 0.09 | 0.11 | 0.18 | 0.09 |
p < .05;
p < .01;
p < .001.
Omitted category is other diagnosis.
Omitted category is friend.
Model controls for level-1 indicators of alter gender, alter trust in physicians, relationship, and closeness of tie.
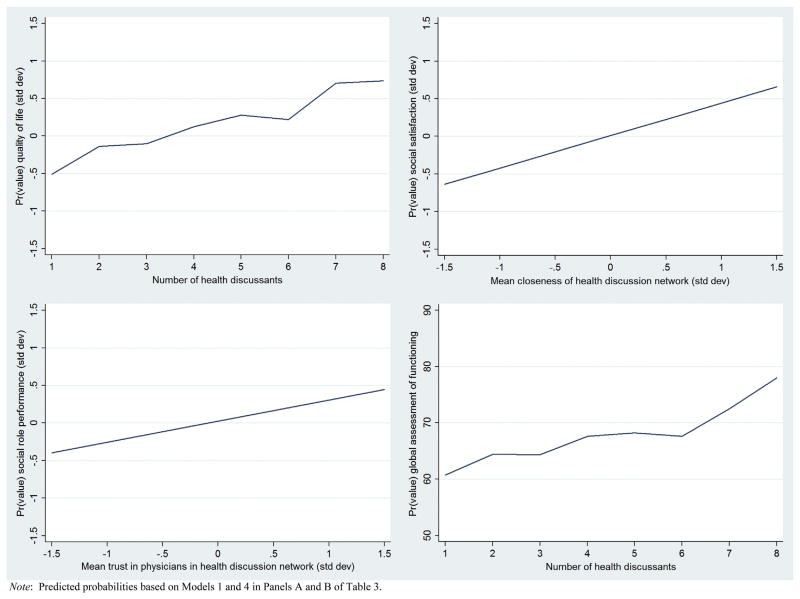
Findings in Model 3 highlight the importance of relationship characteristics. Those in relationships characterized by closeness (OR = 5.39; p < .001) or frequent contact (OR = 2.56; p < .001) are more likely to be activated to discuss health problems relative to others. Relationships with high levels of conflict, hassles, and problems are significantly less likely to be activated for discussion of health problems (OR = 0.38, p < .001). Also, compared to being a friend, being a partner or spouse (OR = 6.58, p < .001), mother (5.51, p < .001), or medical or mental health professional (OR = 1.86, p < .05) is associated with increased odds of being activated for health discussion. In contrast, being a child (OR = 0.16, p < .001), a coworker (OR = 0.45, p < .001), or having some other kind of relationship (OR = 0.17, p < .001) are associated with lower odds of being approached compared to being a friend.2 Graphed as predicted probabilities of tie activation (Fig. 1), the probability that a partner or spouse and mother will be sought out is nearly 0.50 – significantly larger than for any other type of relationship. Particularly striking is the finding that the predicted probability of discussing health with a medical or mental health professional is not significantly different from the probability of talking to a father, sibling, friend, or neighbor.
Fig. 1.
Predicted probabilities of tie activation for health discussion by relationship type.
Model 4 shows significant effects of total network properties over and above the influence of ego or alter characteristics. Any particular alter in a larger network is less likely to be activated for health discussion, on average (OR = 0.96, p < .001). In addition, alters embedded in networks with higher mean trust in physicians have significantly larger odds of being sought out for health discussions, controlling for each alter's own trust in physicians (OR = 1.64, p < .05). Importantly, this suggests that the overall network culture regarding health care systems and providers may have independent effects on the likelihood of talking about health problems.
Does the activation profile matter for recovery?
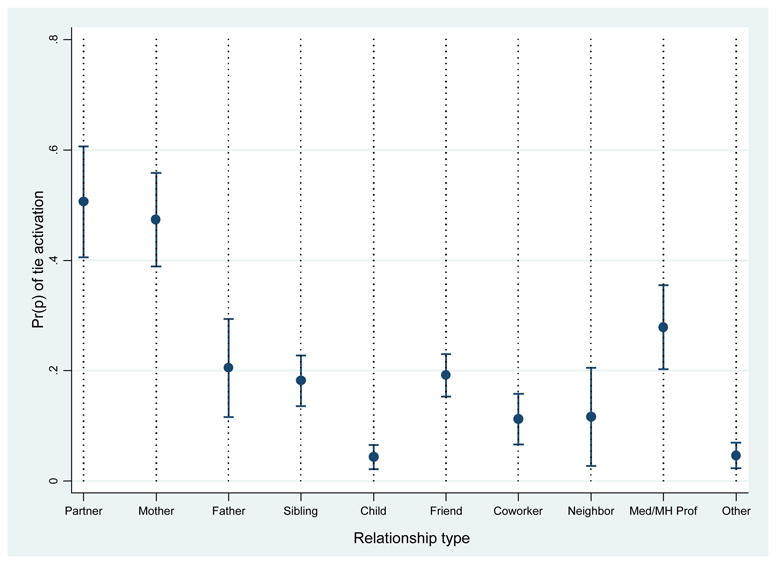
OLS regressions of four different health indicators on characteristics of the activated health discussion network and the inactivated network control for demographic and health characteristics of egos (Table 3). As shown in Models 1–3 of Panel A, characteristics of health discussion networks at the point of entry into mental health treatment are significantly associated with wellbeing about 10 months later. Specifically, higher quality of life is associated with activating a larger number of people for health discussion (b = 0.06, p < .001), feeling closer to health discussants (b = 0.21, p < .05), and perceiving more trust in physicians among health discussants (b = 0.26, p < .001). As shown in Fig. 2, the predicted value of quality life for someone with one health discussant is 0.50 standard deviations below the mean. In contrast, someone with four discussants reports average quality of life, while someone who talks about health with eight people has a predicted quality of life score that is 0.75 standard deviations above the mean. Together, the three characteristics of health discussion networks explain 22% of the variation in quality of life. In contrast, adding identical measures of the inactivated network (i.e. those with whom health is not discussed) results in poorer model fit and no additional explained variance, and none of these measures are statistically significant. When quality of life at Time 1 is added to the model (see Model 3, Panel A), the effects of network size remain significant, providing a conservative test of causality and an estimate of change in quality of life due to the extent of network activation for discussion during a health crisis.
Table 3.
OLS regression of wellbeing outcomes on characteristics of inactivated and health discussion networks (n = 108).
| Panel A | b (SE) | b (SE) | b (SE) | b (SE) | b (SE) | b (SE) |
|---|---|---|---|---|---|---|
|
|
|
|
|
|
|
|
| Quality of life | Social satisfaction | |||||
|
|
|
|||||
| 1 | 2 | 3 | 4 | 5 | 6 | |
| Gender (1 = female) | −0.08 (0.09) | −0.08 (0.09) | −0.08 (0.07) | −0.27 (0.14)* | −0.25 (0.14) | −0.19 (0.12) |
| Race (1 = white) | 0.23 (0.09)** | 0.24 (0.09)** | 0.15 (0.08) | −0.22 (0.14) | −0.17 (0.14) | −0.15 (0.13) |
| Diagnosisa | ||||||
| Schizophrenia | 0.32 (0.15)* | 0.27 (0.16) | 0.16 (0.13) | 0.54 (0.23)* | 0.48 (0.25) | 0.36 (0.23) |
| Depression | 0.11 (0.09) | 0.08 (0.09) | 0.03 (0.08) | 0.17 (0.14) | 0.15 (0.15) | 0.09 (0.13) |
| Health discussion networks | ||||||
| Network size | 0.06 (0.02)*** | 0.06 (0.02)*** | 0.03 (0.02)* | 0.02 (0.03) | 0.02 (0.03) | 0.01 (0.03) |
| Mean closeness | 0.21 (0.09)* | 0.16 (0.09) | 0.08 (0.08) | 0.69 (0.14)*** | 0.62 (0.15)*** | 0.36 (0.14)* |
| Mean trust in physicians | 0.26 (0.08)*** | 0.22 (0.10)* | 0.12 (0.08) | 0.34 (0.12)*** | 0.30 (0.14)* | 0.24 (0.13) |
| Inactivated networks | ||||||
| Network size | 0.01 (0.01) | 0.002 (0.002) | −0.004 (0.01) | 0.001 (0.01) | ||
| Mean closeness | 0.14 (0.11) | 0.02 (0.09) | 0.28 (0.16) | −0.05 (0.16) | ||
| Mean trust in physicians | 0.08 (0.13) | 0.06 (0.11) | 0.04 (0.19) | −0.14 (0.18) | ||
| Dependent variable at T1 | 0.54 (0.08)*** | 0.49 (0.11)*** | ||||
| F | 7.02*** | 5.23*** | 11.19*** | 6.67*** | 5.04*** | 7.65*** |
| Adjusted R2 | 0.28 | 0.28 | 0.51 | 0.28 | 0.29 | 0.42 |
|
| ||||||
| Panel B | Role Performance | Functioning | ||||
|
|
|
|||||
| 1 | 2 | 3 | 4 | 5 | 6 | |
|
| ||||||
| Gender (1 = female) | −0.07 (0.13) | −0.07 (0.13) | −0.15 (0.11) | −3.12 (2.81) | −3.07 (2.94) | −5.21 (3.17) |
| Race (1 = white) | −0.23 (0.12) | −0.21 (0.13) | −0.11 (0.12) | 5.07 (3.63) | 5.30 (4.07) | 4.76 (3.81) |
| Diagnosisa | ||||||
| Schizophrenia | 0.29 (0.21) | 0.37 (0.23) | 0.34 (0.20) | −2.41 (4.79) | −3.54 (5.59) | 8.46 (6.40) |
| Depression | 0.17 (0.13) | 0.20 (0.14) | 0.20 (0.12) | −2.82 (3.20) | −3.86 (3.93) | 0.24 (3.56) |
| Health discussion networks | ||||||
| Network size | 0.05 (0.03) | 0.05 (0.03) | 0.06 (0.02)* | 1.66 (0.70)* | 1.65 (0.70)* | 1.68 (0.63)** |
| Mean closeness | 0.33 (0.13)** | 0.33 (0.13)* | 0.23 (0.12) | 7.12 (3.72) | 4.57 (3.82) | 4.86 (3.10) |
| Mean trust in physicians | 0.32 (0.11)** | 0.40 (0.13)** | 0.38 (0.12)** | 7.66 (3.09)* | 4.27 (3.23) | 4.49 (3.09) |
| Inactivated networks | ||||||
| Network size | 0.001 (0.01) | 0.01 (0.01) | 0.09 (0.20) | 0.24 (0.23) | ||
| Mean closeness | 0.001 (0.15) | −0.12 (0.14) | 8.53 (4.72) | 6.64 (4.32) | ||
| Mean trust in physicians | −0.17 (0.18) | −0.24 (0.16) | 5.27 (4.58) | 1.89 (4.18) | ||
| Dependent variable at T1 | 0.45 (0.09)*** | 0.43 (0.14)** | ||||
| F | 4.19*** | 2.96** | 5.80*** | 2.68** | 2.65** | 2.87** |
| Adjusted R2 | 0.18 | 0.16 | 0.35 | 0.15 | 0.19 | 0.28 |
p < .05;
p < .01;
p < .001.
Omitted category is other diagnosis.
Fig. 2.
Predicted values for each of four wellbeing outcomes as a function of characteristics of health discussion networks (n = 108).
According to results in Model 4 (Panel A, Table 3), higher mean closeness to health discussants (b = 0.69, p < .001) and more trust in physicians in the health network (b = 0.34, p < .001) are significantly related to satisfaction with relationships and social life ten months after entry into mental health treatment. Fig. 2 demonstrates that each one-standard deviation increase in mean closeness to the health network is associated with a 0.50-standard deviation increase in the predicted value of social satisfaction. In all, health network variables explain 21% of the variance in social satisfaction, while the addition of characteristics of the inactivated network add only 1% variance explained and worsen model fit (see Model 5, Panel A). After including baseline measures of social satisfaction, average health network closeness remains significant, suggesting that strength of relationships with health discussants is predictive of improvements in social satisfaction.
Characteristics of discussion networks activated during a health crisis are also associated with perceived social role performance (see Models 1–3, Panel B, Table 3). Better role performance is associated with activating a larger number of people for health discussion (b = 0.05, p = .06 in Model 1, p < .05 in Model 3), feeling closer to health discussants (b = 0.33, p < .01), and perceiving more trust in physicians among health discussants (b = 0.32, p < .01). As shown in Fig. 2, a one-standard deviation increase in mean trust in physicians among health discussants is associated with an increase in the predicted value of social satisfaction that is about one-third of a standard deviation. Together, the health network variables explain 16% of variation in social role performance, while characteristics of the inactivated network explain zero variance and worsen model fit. When social role performance at Time 1 is added (see Model 3, Panel B), size and physician trust in the health discussion network remain significant, suggesting that this network contributes in important ways to improvements in social role performance during recovery from mental illness.
Finally, we find that health network size (b = 1.66, p < .05) and mean trust in physicians in the health network (b = 7.66, p < .05) are significant indicators of social, cognitive, and emotional functioning (as measured by the GAF) ten months following entry into treatment (see Model 4, Panel B, Table 3). For example, a person with one health discussant at baseline is predicted to have a GAF score of 61 at Time 2 (see Fig. 2). However, the predicted GAF scores for someone with four and eight health discussants are 68 and 79, respectively. These variables explain 14% of the variance in GAF at Time 2. Adding measures of the inactivated network increases variance explained by only 4%, in contrast, and none of these variables is statistically significant. After adding the GAF score at baseline to this model, size of the health network remains a significant predictor of improvement in functioning during recovery from mental illness.
Discussion
Social relationships matter for health outcomes. Here, we aim to more fully understand the causes and consequences of turning to social networks during an acute episode of mental illness. While the process of activating ties for health discussion has potential to bring valuable resources for managing distress and illness fallout, it is also risky. Determining whether individuals benefit from connecting to different kinds of health discussion partners among a larger set of latent ties lies at the heart of our concern. Surprisingly little is known about the process of social network activation for health problems, and looking to the advantages or disadvantages, if any, of engaging in targeted discussions has rarely been examined empirically (Perry & Pescosolido, 2010; Shafer, 2013).
Here we longitudinally examine multilevel factors – characteristics of individual egos, alters, relationships, and social networks – that influence the likelihood of tie activation as a strategy for coping with health problems. As such, this study addresses several limitations of existing research on social networks and health. First, clear mechanisms of network influence are rarely measured or appropriately operationalized in empirical research (Pescosolido & Levy, 2002). Most studies focus on general perceptions of support, or rely on less specific forms of discussion (i.e. the “important matters” network from the General Social Survey), that tap into social integration more broadly (Perry & Pescosolido, 2010). Second, most research is narrowly focused on only one level of analysis (typically features of relationships or dyads; Wellman, 1999). However, in practice, social relationship processes cannot be fully understood when relationships are divorced from characteristics of individuals and those in their networks, on one hand, or from the network context in which interaction and resource exchange occur, on the other (Haines, Beggs, & Hurlbert, 2002; Hurlbert et al., 2000; Wellman & Gulia, 1999). Third, relatively few studies employ longitudinal research, providing little basis for causal inference and limiting our ability to distinguish social selection from social causation mechanisms (Smith & Christakis, 2008).
To identify predictors of tie activation, we examine individuals during the period of heightened crisis and uncertainty immediately following first entry into mental health treatment using the Indianapolis Network Mental Health Study, a unique longitudinal dataset of individuals early in the illness career. Our results show that older individuals and those experiencing worse health problems are more likely to reach out to others for health-related discussion, perhaps reflecting the importance of elevated needs in driving topic-focused discussion. We also find that people are especially inclined to rely on partners and mothers (but not fathers) to discuss health relative to other types of ties. The role of gender ideology and the culture of motherhood in maintaining a safety net for adult children with health problems has been observed in previous research (Cook, 1988), as has the importance of the institution of marriage in structuring support obligations of spouses (Idler, Boulifard, & Contrada, 2012; Schafer, 2013; Umberson, 1992). Perhaps more unexpectedly, however, individuals experiencing a mental illness are no more likely to talk about their health problems to medical or mental health professionals than to siblings, friends, fathers, and neighbors, illustrating the critical role of the lay support system in managing mental illness (Swindle, Heller, & Pescosolido, 2000).
Likewise, when faced with a range of potential providers of information, advice, and instrumental and emotional aid, we find that people turn to their core networks (Wellman, 2000). They tend to discuss their health within the context of strong relationships characterized by frequent verbal or face-to-face contact and relatively low levels of conflict or hassles. However, whether or not they are core supporters, individuals are much more likely to discuss their health with those who've had similar mental illness experiences and those who suggested earlier in the illness career that they seek medical or mental health treatment for their problems. Experiential homophily appears to be a strong factor in tie activation for specific problems (Suitor, Pillemer, & Keeton, 1995). Moreover, consistent with previous research on the network context of support (Wellman, 1999; Wellman & Gulia, 1999), individuals with larger personal networks are less likely than those with smaller ones to activate any given tie for health discussion. A small core network of health discussants may be more specialized, cohesive, or cooperative. Also, individuals embedded in networks perceived to be more trusting of medical professionals have a higher likelihood of discussing health, controlling for each network member's own level of trust.
Finally, because discussing health problems with others may have nontrivial social costs, exploring the consequences of network activation for recovery outcomes is an aim of this analysis. Individuals with larger health discussion networks characterized by close ties and a culture of support for medical care at the point of entry into treatment enjoy better outcomes ten months later. Having a strong social safety net that includes engagement in health discussions with particular kinds of people translates into improved quality of life, social satisfaction, ability to perform social roles, and mental health functioning.
Due to efforts by the consumer movement, conceptualizations of recovery from mental illness have broadened considerably, shifting away from an exclusive focus on freedom from symptoms (Cook & Wright, 1995). Rather, contemporary views of recovery emphasize symptom management, development of a positive self-concept, return to former social roles and identities, and attainment of quality of life and sense of purpose (Markowitz, 2001). Consequently, our results on the consequences of tie activation during a mental health crisis underscore the critical role of social networks in the recovery process.
Social networks have the potential to serve as conduits of general emotional support and information. However, according to our findings, it is not these general support processes that drive recovery outcomes. Rather, the key factor appears to be activation of particular kinds of people for health discussion. This indicates that achieving a state of recovery may be facilitated by cultivating a social safety net that can provide targeted, health-related advice, affirmation, and instrumental aid that buoys the treatment process and permits gains in self-sufficiency and productivity. Our research indicates that obtaining this kind of problem-focused support likely requires health discussion. Moreover, consistent with newer definitions, an important component of recovery is embracing mental illness and related experiences as a nontrivial aspect of one's sense of self, and this likely occurs through sharing aspects of the illness experience with others.
Limitations
The INMHS has little information about personal social networks prior to the onset of mental illness or contact with the mental health treatment system. The NEM was developed to understand and examine how social networks shape pathways to care. Thus, INMHS respondents, recruited through the mental health treatment system, may have social networks that differ in unknown ways from those who did not receive specialty care. In addition, contact with the formal treatment system itself could influence the structure and composition of health discussion networks, creating bonds to health professionals and other consumers (Segal & Holschuh, 1991).
In addition, despite using longitudinal data and employing strategies to minimize endogeneity, it is possible that reverse causation or unobserved confounding factors contribute to findings on social network activation and recovery. For example, it is likely that improvements in mental health lead to greater sociability and closer relationships, particularly for individuals with affective disorders. Likewise, recovery outcomes in the INMHS sample are probably driven in large part by unmeasured treatment decisions, medication compliance, and health behaviors that are correlated with characteristics of health discussion networks. In other words, it is probably not health discussion per se that influences outcomes, but rather the behavioral, attitudinal, and emotional products of social regulation through health discussion (e.g. York Cornwell & Waite, 2012). However, we are not able to examine these more nuanced pathways.
Finally, the sample of egos is relatively small, particularly for the longitudinal analysis, and is not representative of all people with mental illness. A restricted subsample of respondents who named at least one health discussant and were present in two waves of data is used in the second component of the analysis. Because the subsample differs significantly from the full sample with respect to gender, the findings on recovery outcomes may not be generalizable to men or to individuals who, for whatever reason, did not talk to others about their health.
Theoretical implications
Broadly, this research continues to build a strong body of research about the socially embedded nature of the response to illness. It provides support for the NEM, offering insight into the dynamic and synergistic relationship between social networks and the illness career, including the functional specificity hypothesis (Perry & Pescosolido, 2010). Yet, much remains to be done and we identify three important theoretical implications.
First, our findings indicate that tie activation during a mental health crisis may be characterized by elements of rationality, often underestimated in studies of people with mental illness. While the NEM was developed to move away from dominant models where service use was generally seen as “help-seeking,” this theory never denied the role of agency, even as it reintroduced the role of coercion and habitus as forces in the lives of people with serious mental illness (Perry, 2012). Our findings suggest a systematic process, whether a conscious or subconscious strategy. Individuals facing a stigmatized illness turn to the two groups most apt to provide emotional and instrumental support and least likely to respond with a desire for social distance – namely the closest members of their core network and those who have previously faced similar problems. Network culture probably plays a significant role in creating a social context that facilitates tie activation. At the same time, people make decisions about who to talk to from among all possible discussants in the network, and our research indicates that this process is in part systematic, reflecting elements of bounded rationality (Pescosolido, 1992).
Second, these selective activation processes have implications for recovery. Individuals who make injudicious decisions, or have only injudicious options (i.e., weaker ties, unsupportive ties), regarding health discussants do not adapt as well later in the illness career relative to those who secure adequate network resources. Our results demonstrate that verbal exchange of health-related attitudes, information, and resources with effectual discussion partners constitutes a strong mechanism linking social networks and health.
Finally, this research underscores that social network structure and culture matter above and beyond the influence of any particular individual or relationship. One of our most striking findings is that people are more likely to discuss health in the context of networks that have a trusting orientation toward physicians, even after alters' own attitudes are held constant. In turn, having health discussion networks characterized by high confidence in physicians is associated with better outcomes later in the illness career. These findings suggest that health discussion networks are conduits of cultural capital that can be accessed during a health crisis. Being embedded in a pro-medical network culture likely facilitates early and consistent use of health services, and may also validate help-seeking decisions. Networks that possess these types of health capital are particularly likely to be activated for medical advice and health discussion, revealing the role of network culture in both the genesis and the consequences of tie activation. During the period of uncertainty surrounding the initial decision to enter formal mental health services, Kadushin's (1966) classic finding on “the friends and supporters of psychotherapy” is echoed. Social influence is “exerted not by single persons but by social circles (786).”
Footnotes
Because fixed effects models have the advantage of controlling for all unobserved heterogeneity, we did run identical models using fixed effects. The results from random-intercept and fixed effects models are very similar, with identical patterns of significance. This reduces concerns about potentially confounding unobserved variables.
It is possible that the effects of relationship type on activation for health discussion are related to each alter's embeddedness in the network. For example, people who fear stigmatization may be more likely to speak about their illness to alters who are isolated from others in the network. In contrast, spouses, mothers, and other highly embedded ties may be perceived as better able to coordinate informal support (Kalmijn, 2003). Though measures of density were not collected for the entire network, we did compute a proxy measure of density equal to the proportion of network members to whom each alter is connected indirectly through kinship with ego. This proxy measure was not statistically significant and did not reduce the significance of the coefficients for relationship type. However, including this measure did reduce the size of the effect of being a mother by 9%, and the effect of being a partner by 7%, indicating that a small proportion of the effect of relationship type on activation for health discussion may be explained by alter embeddedness.
References
- Abbott KM, Bettger JP, Hanlon A, Hirschman KB. Factors associated with health discussion network size and composition among elderly recipients of long-term services and supports. Health Communication. 2012;27:784–793. doi: 10.1080/10410236.2011.640975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ajrouch KJ, Antonucci TC, Janevic MR. Social networks among blacks and whites: the interaction between race and age. Journal of Gerontology: Social Sciences. 2001;56:112–118. doi: 10.1093/geronb/56.2.s112. [DOI] [PubMed] [Google Scholar]
- Barbee A, Derlega V, Sherburne S, Grimshaw A. Helpful and unhelpful forms of social support for HIV-positive individuals. HIV and Social Interaction. 1998:83–105. [Google Scholar]
- Bolger N, Zuckerman A, Kessler RC. Invisible support and adjustment to stress. Journal of Personality and Social Psychology. 2000;79(6):953–961. doi: 10.1037//0022-3514.79.6.953. [DOI] [PubMed] [Google Scholar]
- Bond GR, Witheridge TF, Dincin J, Wasmer D, Webb J, De Graaf-Kaser R. Assertive community treatment for frequent users of psychiatric hospitals in a large city: a controlled study. American Journal of Community Psychology. 1990;18:865–891. doi: 10.1007/BF00938068. [DOI] [PubMed] [Google Scholar]
- Bourdieu P. In: Distinction: A social critique of the judgement of taste. Richard Nice., translator. Cambridge, MA: Harvard University Press; 1984. [Google Scholar]
- Bury M. Chronic illness as biographical disruption. Sociology of Health & Illness. 1982;4(2):167–182. doi: 10.1111/1467-9566.ep11339939. [DOI] [PubMed] [Google Scholar]
- Carpentier N, Ducharme F. Care-giver network transformations: the need for an integrated perspective. Ageing and Society. 2003;23(04):507–525. [Google Scholar]
- Carpentier N, Ducharme F. Support network transformations in the first stages of the caregiver's career. Qualitative Health Research. 2005;15:289–311. doi: 10.1177/1049732304270813. [DOI] [PubMed] [Google Scholar]
- Carpentier N, Lesage A, White D. Family influence on the first stages of the trajectory of patients diagnosed with severe psychiatric disorders. Family Relations. 1999;48(4):397–403. [Google Scholar]
- Cook JA. Who “Mothers” the chronically mentally ill? Family Relations. 1988;37:42–49. [Google Scholar]
- Cook JA, Wright ER. Medical sociology and the study of severe mental illness: reflections on past accomplishments and directions for future research. Journal of Health and Social Behavior. 1995;35:95–114. [PubMed] [Google Scholar]
- Cutrona CE, Russell D. Type of social support and specific stress: toward a theory of optimal matching. In: Sarason I, Sarason B, Pierce G, editors. Social support: An interactional view. New York: Wiley and Sons; 1990. [Google Scholar]
- Emirbayer M, Goodwin J. Network analysis, culture, and the problem of agency. American Journal of Sociology. 1994;99:1411–1454. [Google Scholar]
- Fehr E, Fischbacher U, Gächter S. Strong reciprocity, human cooperation, and the enforcement of social norms. Human Nature. 2002;13(1):1–25. doi: 10.1007/s12110-002-1012-7. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Nadler A, Whitcher-Alagna S. Recipient reactions to aid. Psychological Bulletin. 1982;91:27–54. [Google Scholar]
- Friedson E. Professional dominance: The social structure of medical care. New York, NY, Atherton: 1970. [Google Scholar]
- Gallant MP. The influence of social support on chronic illness self-management: a review and directions for research. Health Education & Behavior. 2003;30(2):170–195. doi: 10.1177/1090198102251030. [DOI] [PubMed] [Google Scholar]
- Haines VA, Beggs JJ, Hurlbert JS. Exploring the structural contexts of the support process: social networks, social statuses, social support, and psychological distress. Advances in Medical Sociology. 2002;8:269–292. [Google Scholar]
- Horowitz LM, Krasnoperova EN, Tatar DG, Hansen MB, Person EA, Galvin KL, et al. The way to console may depend on the goal: experimental studies of social support. Journal of Experimental Social Psychology. 2001;37(1):49–61. [Google Scholar]
- House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241(4865):540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- Hurlbert JS, Haines VA, Beggs JJ. Core networks and tie activation: what kinds of routine networks allocate resources in nonroutine situations? American Sociological Review. 2000;65(4):598–618. [Google Scholar]
- Idler EL, Boulifard DA, Contrada RJ. Mending broken hearts: marriage and survival following cardiac surgery. Journal of Health and Social Behavior. 2012;53:33–49. doi: 10.1177/0022146511432342. [DOI] [PubMed] [Google Scholar]
- Kadushin C. The friends and supporters of psychotherapy: on social circles in urban life. American Sociological Review. 1966:786–802. [PubMed] [Google Scholar]
- Kalmijn M. Shared friendship networks and the life course: an analysis of survey data on married and cohabiting couples. Social Networks. 2003;25(3):231–249. [Google Scholar]
- Karp DA. The burden of sympathy: How families cope with mental illness. New York: Oxford University Press; 2001. [Google Scholar]
- Kleinman A. Culture and depression. New England Journal of Medicine. 2004;351:951–952. doi: 10.1056/NEJMp048078. [DOI] [PubMed] [Google Scholar]
- Krause N. Received support, anticipated support, social class, and mortality. Research on Aging. 1997;19(4):387–422. [Google Scholar]
- Lehman AF. A quality of life interview for the chronically mentally ill. Evaluation of Program Planning. 1988;11:51–62. [Google Scholar]
- Lehman DR, Ellard JH, Wortman CB. Social support for the bereaved: recipients' and providers' perspectives on what is helpful. Journal of Consulting and Clinical Psychology. 1986;54(4):438. [Google Scholar]
- Lin N. Building a network theory of social capital. Connections. 1999;22(1):28–51. [Google Scholar]
- Link BG. Understanding labeling effects in the area of mental disorders: an assessment of the effects of expectations of rejection. American Sociological Review. 1987:96–112. [Google Scholar]
- Link BG, Cullen FT, Struening E, Shrout PE, Dohrenwend BP. A modified labeling theory approach in the area of mental disorders: an empirical assessment. American Sociological Review. 1989;54(3):100–123. [Google Scholar]
- Link BG, Mirotznik J, Cullen FT. The effectiveness of stigma coping orientations: can negative consequences of mental illness labeling be avoided? Journal of Health and Social Behavior. 1991;32(3):302–320. [PubMed] [Google Scholar]
- Lipton FR, Cohen CI, Fischer E, Katz SE. Schizophrenia: a network crisis. Schizophrenia Bulletin. 1981;7:144–151. doi: 10.1093/schbul/7.1.144. [DOI] [PubMed] [Google Scholar]
- Lively KJ, Smith CL. Handbook of the sociology of health, illness, and healing. New York: Springer; 2011. Identity and illness; pp. 505–525. [Google Scholar]
- Lizardo O. How cultural tastes shape personal networks. American Sociological Review. 2006;71:778–807. [Google Scholar]
- Lo MCM, Stacey CL. Beyond cultural competency: bourdieu, patients and clinical encounters. Sociology of Health & Illness. 2008;30:741–755. doi: 10.1111/j.1467-9566.2008.01091.x. [DOI] [PubMed] [Google Scholar]
- Markowitz FE. Modeling processes in recovery from mental illness: relationships between symptoms, life satisfaction, and self-concept. Journal of Health and Social Behavior. 2001;42:64–79. [PubMed] [Google Scholar]
- Marsden P. Core discussion networks of Americans. American Sociological Review. 1987;52:122–131. [Google Scholar]
- Michalos AC. Multiple discrepancies theory (MDT) Social Indicators Research. 1985;16(4):347–413. [Google Scholar]
- de Miguel Luken V, Tranmer M. Personal support networks of immigrants to Spain: a multilevel analysis. Social Networks. 2010;32(4):253–262. [Google Scholar]
- Muhlbauer SA. Navigating the storm of mental illness: phases in the family's journey. Qualitative Health Research. 2002;12(8):1076–1092. doi: 10.1177/104973202129120458. [DOI] [PubMed] [Google Scholar]
- Nichter M. Global health: Why cultural perceptions, social representations, and biopolitics matter. University of Arizona Press; 2008. [Google Scholar]
- Pachucki MA, Breiger RL. Cultural holes: beyond relationality in social networks and culture. Annual Review of Sociology. 2010;36:205–224. [Google Scholar]
- Parsons T. The social system. New York: The Free Press; 1951. [Google Scholar]
- Peek MK, O'Neill GS. Networks in later life: an examination of race differences in social support networks. International Journal of Aging and Human Development. 2001;52:197–219. doi: 10.2190/F1Q1-JV7D-VN77-L6WX. [DOI] [PubMed] [Google Scholar]
- Penning MJ. Receipt of assistance by elderly people: hierarchical selection and task specificity. The Gerontologist. 1990;30(2):220–227. doi: 10.1093/geront/30.2.220. [DOI] [PubMed] [Google Scholar]
- Perry BL. The labeling paradox stigma, the sick role, and social networks in mental illness. Journal of Health and Social Behavior. 2011;52:460–477. doi: 10.1177/0022146511408913. [DOI] [PubMed] [Google Scholar]
- Perry BL. Coming untied? Narrative accounts of social network dynamics from first-time mental health clients. Sociology of Health & Illness. 2012;34(8):1125–1139. doi: 10.1111/j.1467-9566.2012.01459.x. [DOI] [PubMed] [Google Scholar]
- Perry BL, Pescosolido BA. Functional specificity in discussion networks: the influence of general and problem-specific networks on health outcomes. Social Networks. 2010;32(4):345–357. [Google Scholar]
- Perry BL, Pescosolido BA. Social network dynamics and biographical disruption: the case of “first-timers” with mental illness. American Journal of Sociology. 2012;118(1):134–175. [Google Scholar]
- Pescosolido BA. Illness careers and network ties: a conceptual model of utilization and compliance. Advances in Medical Sociology. 1991;2:161–184. [Google Scholar]
- Pescosolido BA. Beyond rational choice: the social dynamics of how people seek help. American Journal of Sociology. 1992;97(4):1096–1138. [Google Scholar]
- Pescosolido BA. Of pride and prejudice: the role of sociology and social networks in integrating the health sciences. Journal of Health and Social Behavior. 2006 Sep;47:189–208. doi: 10.1177/002214650604700301. [DOI] [PubMed] [Google Scholar]
- Pescosolido BA, Brooks-Gardner C, Lubell KM. Choice, coercion, and muddling through: accounts of help-seeking from ‘First-Timers’. Social Science & Medicine. 1998;46(2):275–286. doi: 10.1016/s0277-9536(97)00160-3. [DOI] [PubMed] [Google Scholar]
- Pescosolido BA, Levy JA. The role of social networks in health, illness, disease, and healing: the accepting present, the forgotten past, and the dangerous potential for a complacent future. Social Networks and Health. 2002;8:3–25. [Google Scholar]
- Pescosolido BA, Martin JK, Long JS, Medina TR, Phelan JC, Link BG. A disease like any other'? A decade of change in public reactions to schizophrenia, depression, and alcohol dependence. American Journal of Psychiatry. 2010;167(11):1321–1330. doi: 10.1176/appi.ajp.2010.09121743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rafaeli E, Gleason MEJ. Skilled support within intimate relationships. Journal of Family Theory & Review. 2009;1(1):20–37. [Google Scholar]
- Salokangas RK. Living situation, social network and outcome in schizophrenia: a five-year prospective follow-up study. Acta Psychiatrica Scandinavica. 1997;96:459–468. doi: 10.1111/j.1600-0447.1997.tb09948.x. [DOI] [PubMed] [Google Scholar]
- Sandefur RL, Laumann EO. A paradigm for social capital. Rationality and Society. 1998;10(4):481–501. [Google Scholar]
- Schafer MH. Discussion networks, physician visits, and non-conventional medicine: probing the relational correlates of health care utilization. Social Science & Medicine. 2013;87:176–184. doi: 10.1016/j.socscimed.2013.03.031. [DOI] [PubMed] [Google Scholar]
- Segal SP, Holschuh J. Effects of sheltered care environments and resident characteristics on the development of social networks. Hospital and Community Psychiatry. 1991;42(11):1125. doi: 10.1176/ps.42.11.1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharfstein SS. Goals of inpatient treatment for psychiatric disorders. Annual Review of Medicine. 2009;60:393–403. doi: 10.1146/annurev.med.60.042607.080257. [DOI] [PubMed] [Google Scholar]
- Simons RL. Specificity and substitution in the social networks of the elderly. International Journal of Aging and Human Development. 1983-1984;18(2):121–139. doi: 10.2190/auy4-cmpk-jfcb-e04v. [DOI] [PubMed] [Google Scholar]
- Singh-Manoux A, Marmot M. Role of socialization in explaining social inequalities in health. Social Science & Medicine. 2005;60:2129–2133. doi: 10.1016/j.socscimed.2004.08.070. [DOI] [PubMed] [Google Scholar]
- Smith KP, Christakis NA. Social networks and health. Annual Review of Sociology. 2008;34(1):405–429. [Google Scholar]
- Snijders TA, Spreen M, Zwaagstra R. The use of multilevel modeling for analysing personal networks: networks of cocaine users in an urban area. Journal of Quantitative Anthropology. 1995;5(4):85–105. [Google Scholar]
- Spitzer RL, Williams J, Gibbon M, First MB. Structured clinical interview for DSM-III-R, patient edition. Washington, D.C.: American Psychiatric Press; 1990. [Google Scholar]
- Startup M, Jackson MC, Bendix S. The concurrent validity of the global assessment of functioning. British Journal of Clinical Psychology. 2002;41(4):417–422. doi: 10.1348/014466502760387533. [DOI] [PubMed] [Google Scholar]
- Suitor JJ, Pillemer K, Keeton S. When experience counts: the effects of experiential and structural similarity on patterns of support and interpersonal stress. Social Forces. 1995;73(4):1573–1588. [Google Scholar]
- Swindle R, Heller K, Pescosolido B. Responses to nervous breakdowns in America over a 40-year period. American Psychologist. 2000;55(7):740–749. doi: 10.1037//0003-066x.55.7.740. [DOI] [PubMed] [Google Scholar]
- Thoits PA. Mechanisms linking social ties and support to physical and mental health. Journal of Health and Social Behavior. 2011;52(2):145–161. doi: 10.1177/0022146510395592. [DOI] [PubMed] [Google Scholar]
- Umberson D. Gender, marital status and the social control of health behavior. Social Science & Medicine. 1992;34(8):907–917. doi: 10.1016/0277-9536(92)90259-s. [DOI] [PubMed] [Google Scholar]
- Wahl O. Telling is risky business. New Brunswick, NJ: Rutgers University Press; 2000. [Google Scholar]
- Wahl O. Stigma as a barrier to recovery from mental illness. Trends in Cognitive Sciences. 2012;16(1):9–10. doi: 10.1016/j.tics.2011.11.002. [DOI] [PubMed] [Google Scholar]
- Ware NC, Idoko J, Kaaya S, Biraro IA, Wyatt MA, Agbaji O, et al. Explaining adherence success in sub-Saharan Africa: an ethnographic study. PLoS Medicine. 2009;6:e1000011. doi: 10.1371/journal.pmed.1000011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wellman B. Network capital in a multi-level world: getting support from personal communities. In: Lin N, Cook K, Bury R, editors. Social capital: Theory and research. Chicago: Aldine de Gruter; 1999. pp. 233–273. [Google Scholar]
- Wellman B. Partners in illness: who helps when you are sick? In: Kelnar M, Wellman B, Pescosolido BA, Saks M, editors. Complementary and alternative medicine: Challenge and change. Amsterdam, Netherlands: Harwood Academic Publishers; 2000. pp. 143–162. [Google Scholar]
- Wellman B, Gulia M. The network basis of social support: a network is more than the sum of its ties. In: Wellman B, editor. Networks in the global village: Life in contemporary communities. Boulder, CO: Westview; 1999. pp. 83–118. [Google Scholar]
- Wellman B, Wortley S. Brothers' keepers: Situating kinship relations in broader networks of social support. Sociological perspectives. 1989:273–306. [Google Scholar]
- Wellman B, Wortley S. Different strokes from different folks: community ties and social support. American Journal of Sociology. 1990;96(3):558–588. [Google Scholar]
- York Cornwell E, Waite LJ. Social network resources and management of hypertension. Journal of Health and Social Behavior. 2012;53:215–231. doi: 10.1177/0022146512446832. [DOI] [PMC free article] [PubMed] [Google Scholar]