Abstract
Objective
To examine the association between hospital, patient, and local health system characteristics and the likelihood, prevalence, and duration of observation care among fee-for-service Medicare beneficiaries.
Data Sources
The 100 percent Medicare inpatient and outpatient claims and enrollment files for 2009, supplemented with 2007 American Hospital Association Survey and 2009 Area Resource File data.
Study Design
Using a lagged cross-sectional design, we model the likelihood of a hospital providing any observation care using logistic regression and the conditional prevalence and duration of observation care using linear regression, among 3,692 general hospitals in the United States.
Principle Findings
Critical access hospitals (CAHs) have 97 percent lower odds of providing observation care compared to other hospitals, and they conditionally provide three fewer observation stays per 1,000 visits. The provision of observation care is negatively associated with the proportion of racial minority patients, but positively associated with average patient age, proportion of outpatient visits occurring in the emergency room, and diagnostic case mix. Duration is between 1.5 and 2.8 hours shorter at government-owned, for-profit hospitals, and CAHs compared to other nonprofit hospitals.
Conclusions
Variation in observation care depends primarily on hospital characteristics, patient characteristics, and geographic measures. By contrast, local health system characteristics are not a factor.
Keywords: Observation status, observation care, hospitals, Medicare, elderly
In May 2013, the Centers for Medicare and Medicaid Services issued a proposed rule in the Federal Register outlining changes to the Medicare billing policy for observation care (Centers for Medicare and Medicaid Services 2013). The proposed rule would limit the duration of an observation stay by automatically converting any stay in excess of two midnights to an inpatient admission. The proposed rule was issued in response to growing policy concerns over the increasing use and extended duration of observation stays among Medicare beneficiaries, as summarized in a July 2013 report from the Office of Inspector General (2013). These most recent developments are merely the latest in what has been a series of congressional hearings, lawsuits, and advocacy efforts focused on observation care policy (Center for Medicare Advocacy 2011, 2012; Morgan 2011).
When patients present at the emergency department, their symptoms may warrant further close evaluation and monitoring rather than immediate hospitalization or discharge. In such cases, physicians may place the patient under observation care, defined by the Centers for Medicare and Medicaid Services (CMS) as “specific, clinically appropriate services, which include ongoing short-term treatment, assessment, and re-assessment that are furnished while a decision is being made regarding whether patients will require further treatment as hospital inpatients or if they are able to be discharged from the hospital” (Centers for Medicare and Medicaid Services 2011).
From the provider's perspective, observation care often uses fewer resources than inpatient care, can improve diagnostic accuracy, and may reduce patient risks associated with hospitalization (Farkouh et al. 1998; Baugh, Venkatesh, and Bohan 2011). However, observation care can also have unintended consequences for patients. For example, Medicare beneficiaries are responsible for a $147 deductible and 20 percent co-insurance for most outpatient services (up to 100 percent for some hospital charges). By contrast, if patients are admitted to the hospital, they pay a single $1,184 deductible for the first 60 days and are not responsible for any additional charges. Therefore, an observation stay can impose greater financial liability on patients than an inpatient admission (Centers for Medicare and Medicaid Services 2012a). Evidence suggests that the burden is substantial for some patients, leading to growing interest in this issue among policy makers and Medicare advocacy groups (Armstrong 2010; Center for Medicare Advocacy 2010, 2011; Jaffe 2010). Several studies have described the increasing prevalence and duration of observation stays as well as the characteristics of patients and the costs and benefits associated with observation care (Cooke, Higgins, and Kidd 2003; Mace et al. 2003; Schuur, Venkatesh, and Bohan 2010; Venkatesh et al. 2011; Feng, Wright, and Mor 2012).
Significance
While substantial interhospital variation in observation care has been reported, it is unclear how much of this variation is driven by patient characteristics (e.g., diagnosis, age, race, gender) versus hospital characteristics (e.g., ownership, size, location) or local health system characteristics (e.g., competition with other local providers, physician supply) (Feng, Wright, and Mor 2012). Prior studies have either focused solely on the availability of observation units at the hospital level (Wiler, Ross, and Ginde 2011) or have examined both the availability of observation units at the hospital level and predictors of observation use at the patient level (Venkatesh et al. 2011). Both of these studies relied on the National Hospital Ambulatory Medical Care Survey, which consists of a nationally representative sample of hospitals and all-payer patient data. Our study extends this work by using the 100 percent Medicare claims file to get comprehensive data on the 65 and up Medicare population, and incorporating more extensive data on hospital characteristics. The objective of this study was to examine the association between hospital, patient, and local health system characteristics and the likelihood, prevalence, and duration of observation stays among fee-for-service Medicare beneficiaries at the hospital level in 2009.
Methods
Sample and Data
We identified observation stays among fee-for-service Medicare beneficiaries using the 100 percent Medicare outpatient claims file (for institutional providers) for 2009, supplemented with the 100 percent Medicare inpatient claims file to standardize observation stays relative to the sum of inpatient admissions and outpatient visits. We used the Medicare enrollment file to limit our sample to fee-for-service Medicare beneficiaries, age 65 and older. Hospital-level characteristics were drawn from 2007 American Hospital Association Survey data and merged with county-level health system characteristics from the 2009 Area Resource File (ARF), which reports 2007 data. The use of the 2-year lag allows for a delay between hospital administrative composition and culture and its impact on the billing/utilization of observation care, and the ARF data were matched to this time period.
Starting with 4,622 hospitals, we limited our sample using a number of criteria as shown in Figure1. First, we excluded all federal hospitals (N = 31) because they do not receive Medicare reimbursement. Next, we excluded all nongeneral hospitals (N = 147) to eliminate specialized hospitals (e.g., psychiatric facilities, long-term hospitals) from our study. Then, we excluded 11 hospitals that were not in operation for the full year during 2007. Then, because observation stays overwhelmingly arise from emergency department visits, and estimates for hospitals with fewer than 25 annual admissions can be unstable, we dropped hospitals without a dedicated emergency department (N = 694) or at least 25 Medicare admissions per year (N = 39). Finally, we dropped hospitals that were missing data about the hospital's operation of a freestanding outpatient clinic (N = 4), freestanding emergency department (N = 3), or outpatient surgery unit (N = 1), leaving 3,692 hospitals for analysis.
Figure 1.
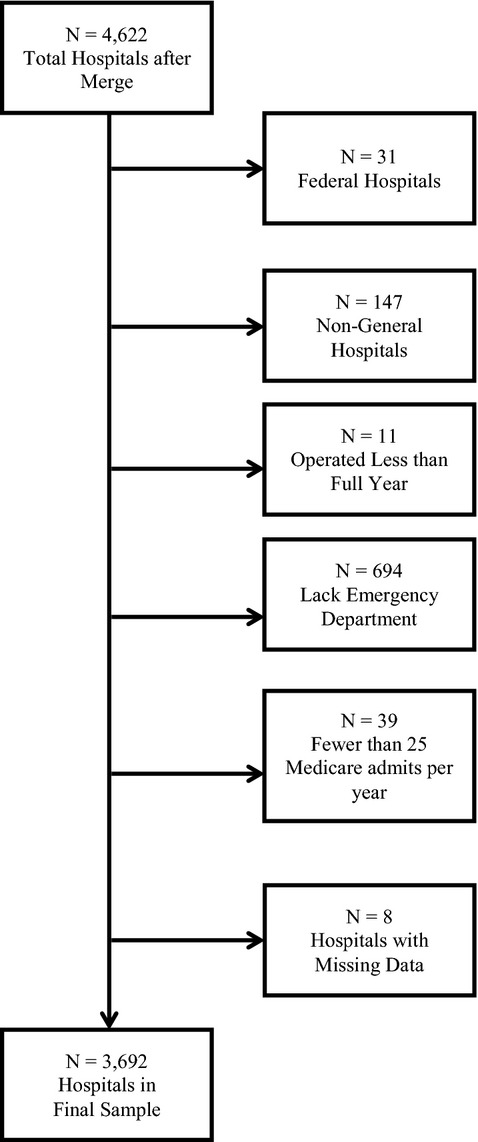
Hospital Sample Selection Criteria
Analysis
Using Medicare claims data, we identified observation stays, inpatient admissions, and outpatient visits at the individual level. Observation stays were flagged by the co-occurrence of specific revenue center codes (0760 or 0762) together with specific Healthcare Common Procedure Coding System classifications (G0378 or G0379). Next, we aggregated these counts to the hospital level and calculated the annual number of observation stays for every 1,000 visits (inpatient admissions + outpatient visits) for each hospital in our sample. Then, we calculated the average duration of each hospital's observation stays. These data and the derivation of our dependent variables have been described previously (citation withheld for review).
Because 18.1 percent of hospitals in our sample provided no observation care, we used logistic regression to model the likelihood of a hospital providing any observation care as a function of hospital characteristics, patient characteristics, local health system characteristics, and state fixed effects. Next, we used two ordinary least squares regression models to estimate the hospital-specific prevalence and average duration of observation care as a function of the same independent variables, conditional on the hospital having at least one observation stay.
Hospital characteristics included bed count, medical school affiliation, critical access hospital status, and ownership type. We selected these variables based on earlier findings that observation units are more prevalent in nonprofit, government, and nonteaching hospitals, and we included a categorical measure of bed count to capture hospital size (Yealy et al. 1989; Venkatesh et al. 2011). We controlled for critical access hospital status because these facilities are subject to unique CMS rules regarding observation stays, which appear to be differentially influencing their use of observation care compared to other hospitals (Hale 2008; Wright et al. 2013). To capture a relative measure of emergency room volume (which produces the majority of observation stays), we included the proportion of outpatient visits that occurred in the emergency room. Because some hospitals may have a large number of outpatient visits in settings that are unlikely to generate an observation stay, we also include four binary controls that indicate whether the hospital operated a freestanding outpatient clinic, freestanding emergency department, urgent care center, and/or outpatient surgery unit. To account for differences in acuity and practice patterns, we also included a variable for Medicare beneficiaries' average length of stay.
Patient characteristics included the proportion of a hospital's outpatient visits by race, gender, and average age. We included these controls because prior analyses have found that female gender and older age are associated with increased prevalence and duration of observation stays, while nonwhite race is associated with decreased prevalence, but increased duration, of observation stays (Feng, Wright, and Mor 2012). Because certain clinical presentations are more likely to result in an observation stay, we adjusted for hospital case mix using a measure that captures the proportion of a hospital's outpatient visits that were for any one of the ten most prevalent observation care diagnoses (Venkatesh et al. 2011). Hospitals that see these diagnoses more often would be expected to have a higher prevalence of observation stays.
Local health system characteristics included county-level measures of physicians per 1,000 population, total population, proportion of Medicare beneficiaries in managed care, and the number of short-term general hospitals per 10,000 population. We included per capita physician supply to determine if the adequacy of the health care workforce plays a role in reducing the need and/or use of observation care. We controlled for local Medicare managed care penetration rates because they directly affect our numerator and denominator (since claims data are not available for these beneficiaries) and in areas with higher rates of Medicare managed care, we expect the remaining fee-for-service population to be less healthy, on average, as managed care plans have historically attracted healthier subpopulations within Medicare. We also controlled for local market competition by including the number of other short-term general hospitals in the area, and adjusting for market size using both total population and indicators of metropolitan and micropolitan areas (relative to rural areas). Finally, we included a dummy variable for each state to account for time-invariant unobserved state effects, and we adjusted for within-state correlation of the hospital-specific error terms using state-clustered standard errors. For ease of presentation, the coefficients on these state variables are not reported in the results. However, they are available upon request. This study was exempted from human subjects review by the Institutional Review Board.
Results
Sample Characteristics
Descriptive statistics for this sample are shown in Table 1 and are broken out into two groups reflecting hospitals that did and did not provide any observation care in 2009. A series of t-tests indicate significant differences in means between the two groups. Among hospitals providing any observation care, the mean number of observation stays per 1,000 visits (inpatient + outpatient) was 14.2, though it ranged from a low of 0.01 to a high of 119.5. Similarly, among this conditional sample, the mean duration of observation stays was 25.9 hours, ranging from a low of 0 (kept less than 1 hour) to a high of 95 hours, or nearly 4 days.
Table 1.
Sample Descriptive Statistics by Provision of Observation Care, 2009
| No Observation Care | Any Observation Care | |
|---|---|---|
| Hospital characteristics (n) | ||
| % by bed count | ||
| 6–24 (260) | 15.9 | 5.1* |
| 25–49 (791) | 43.9 | 16.5* |
| 50–99 (655) | 17.8 | 17.7 |
| 100–199 (814) | 9.3 | 24.9* |
| 200–299 (486) | 4.8 | 15.0* |
| 300–399 (287) | 3.4 | 8.7* |
| 400–499 (162) | 1.5 | 5.0* |
| 500+ (237) | 3.4 | 7.1* |
| % with medical school affiliation (898) | 12.9 | 26.9* |
| % critical access hospitals (1,005) | 73.7 | 17.0* |
| % with freestanding emergency dept. (158) | 1.9 | 4.8* |
| % with freestanding outpatient clinic (1,109) | 17.4 | 32.8* |
| % with outpatient surgery unit (3,510) | 88.6 | 96.5* |
| % with urgent care clinic (867) | 14.2 | 25.5* |
| Ownership type | ||
| % Government, nonfederal (920) | 40.9 | 21.4* |
| % For-profit (487) | 5.8 | 14.8* |
| % Nonprofit (2,285) | 53.3 | 63.8* |
| ED visits as % of outpatient visits | 24.0 (19.8) | 29.3* (19.0) |
| Medicare length of stay | 4.9 (1.1) | 5.5* (0.9) |
| Patient characteristics | ||
| Average age | 77.6 (1.6) | 76.9* (1.4) |
| % Male | 38.8 (4.1) | 38.4* (4.0) |
| % Black | 6.2 (13.7) | 7.5* (12.3) |
| % Asian | 1.0 (5.4) | 1.2 (3.8) |
| % Hispanic | 1.5 (4.8) | 1.7 (4.7) |
| % Other race | 2.2 (8.0) | 1.5* (3.0) |
| % Top 10 observation diagnoses | 14.3 (5.2) | 12.9* (4.6) |
| Local health system characteristics | ||
| Physicians per 1,000 population | 1.1 (1.1) | 1.6* (1.0) |
| Population (10,000) | 35.1 (110.0) | 60.2* (145.2) |
| % of Beneficiaries in Medicare HMO | 14.1 (12.2) | 18.4* (12.9) |
| No. of short-term general hospitals per 100,000 population | 9.6 (11.8) | 3.8* (6.1) |
| % Metropolitan area | 34.1 | 60.6* |
| % Micropolitan area | 13.5 | 20.1* |
| Sample size (N) | 668 | 3,024 |
Note. Standard deviation shown in parentheses. To calculate the proportion of hospitals with specific characteristics that do or do not provide any observation care, simply multiple the percentage in a selected row and column by the overall denominator (N) for that column, and divide this figure by the hospital-specific denominator (n) in the corresponding row. For example, the proportion of all for-profit hospitals that do not provide any observation care is found by (6.0 × 668)/487 = 8.2%.
p <.05.
Hospital Provision of Any Observation Care
Results from the logistic regression model of a hospital's likelihood of providing any observation care are shown in Table 2. All hospitals in Delaware and Rhode Island had observation stays; thus, 14 hospitals (5 in DE, 9 in RI) were dropped from the logistic regression model but included in the subsequent OLS models. Hospital size and critical access hospital status are the only hospital characteristics significantly associated with the likelihood of providing any observation care. Specifically, the odds of having any observation stays are 97 percent lower at critical access hospitals compared to other short-term general hospitals. In our sample, there were 1,005 critical access hospitals, 492 of which did not provide any observation care, compared to 2,687 prospective payment system hospitals, of which only 176 did not provide any observation care.
Table 2.
Logistic Model Predicting Likelihood of Providing Any Observation Care
| Odds Ratio | |
|---|---|
| Hospital characteristics | |
| Bed count | |
| 6–24 | 0.459* (0.164) |
| 25–49 | 0.421** (0.102) |
| 50–99 | 0.471** (0.122) |
| 200–299 | 1.313 (0.221) |
| 300–399 | 1.423 (0.425) |
| 400–499 | 1.610 (0.487) |
| 500+ | 1.536 (0.462) |
| Medical school affiliation | 0.968 (0.177) |
| Critical access hospital | 0.034** (0.010) |
| Freestanding emergency dept. | 0.867 (0.434) |
| Freestanding outpatient clinic | 1.139 (0.154) |
| Outpatient surgery unit | 1.514 (0.347) |
| Urgent care clinic | 1.088 (0.198) |
| Ownership type | |
| Government, non-federal | 0.751* (0.109) |
| For-profit | 0.794 (0.282) |
| ED visits as% of outpatient visits | 1.006* (0.003) |
| Medicare length of stay | 1.125 (0.180) |
| Patient characteristics | |
| Average age | 1.188* (0.085) |
| % Male | 1.018 (0.022) |
| % Black | 0.985** (0.004) |
| % Asian | 0.962** (0.004) |
| % Hispanic | 0.964 (0.023) |
| % Other race | 0.946** (0.014) |
| % Top 10 observation diagnoses | 1.012 (0.020) |
| Local health system characteristics | |
| Physicians per 1,000 population | 0.885 (0.088) |
| Population (10,000) | 0.999 (0.001) |
| % of Beneficiaries in Medicare HMO | 0.985 (0.010) |
| No. of short-term general hospitals per 100,000 population | 0.988 (0.008) |
| Metropolitan area | 0.946 (0.197) |
| Micropolitan area | 1.381* (0.214) |
| Sample size (N) | 3,678 |
Note. Coefficients for state dummy variables are not shown here but are available by request. Robust standard errors in parentheses.
Significant at 5%;
1%.
A Wald test of the construct of hospital bed size confirms that this is also a significant determinant of the likelihood of providing any observation care (χ2 (7) = 24.1, p =.0011). In particular, smaller hospitals with fewer than 100 beds are less likely to provide any observation care. Compared to hospitals with between 100 and 199 beds, hospitals with 50–99 beds have 53 percent lower odds, hospitals with 25–49 beds have 58 percent lower odds, and hospitals with 6–24 beds have 54 percent lower odds of providing any observation care. While larger hospitals appear to have greater odds of providing any observation care, these results are not statistically significant. Likewise, both government and for-profit hospitals appear less likely than nonprofit hospitals to provide any observation care. However, while the coefficient on nonfederal public hospitals is statistically significant, a Wald test of the construct of hospital ownership was not significant (χ2 (2) = 4.07, p =.1305).
Several patient characteristics are also significant predictors of hospitals providing any observation care. A Wald test confirms that the construct of patient race is significant (χ2 (4) = 117.3, p <.0001). In particular, the proportion of minority patients is negatively associated with the likelihood of providing any observation care. Each 1 percentage point increase in the proportion of a hospital's patients who are black decreases the odds of providing any observation care by nearly 2 percent relative to whites. For Asians, the odds are reduced by 4 percent, and for other race, which includes Native Americans, multiracial individuals, and unidentified races, the odds are reduced by 5 percent. However, the proportion of a hospital's patients who are Hispanic is not significantly associated with the hospital's likelihood of providing any observation care. By contrast, each 1 year increase in the average age of a hospital's Medicare outpatient population is associated with a 19 percent increase in the odds of the hospital providing any observation care. Neither gender nor patient mix by observation-related diagnosis was significant.
Of the local health system characteristics, only the state dummies (not shown) and micropolitan location were significant predictors of a hospital's likelihood of providing any observation care. In particular, compared to hospitals in rural areas, hospitals in micropolitan areas have 38 percent higher odds of providing any observation care.
Conditional Prevalence of Observation Stays
The results of the linear regression model predicting observation stay prevalence among the conditional sample of hospitals providing any observation care are shown in Table 3. While some of the same factors (e.g., critical access hospital status, hospital's patient-mix by race) are significant predictors of both a hospital's likelihood of providing any observation care and the prevalence of observation care provided conditional on providing any, other factors are unique predictors of each outcome. Most notably, critical access hospital status is associated with both a lower likelihood of providing any observation care and a lower conditional prevalence of observation stays. Specifically, critical access hospitals have, on average, three fewer observation stays per 1,000 visits per year. As in the logistic model, hospital ownership is not a significant factor in observation stay prevalence.
Table 3.
Model Predicting Conditional Hospital-Level Prevalence of Observation Stays
| Coefficient | |
|---|---|
| Hospital characteristics | |
| Bed count | |
| 6–24 | −1.582 (1.365) |
| 25–49 | −1.609* (0.737) |
| 50–99 | −0.247 (0.794) |
| 200–299 | 1.435 (0.861) |
| 300–399 | 2.346** (0.853) |
| 400–499 | 1.353 (0.964) |
| 500+ | 0.665 (1.224) |
| Medical school affiliation | −0.641 (0.970) |
| Critical access hospital | −3.022** (1.106) |
| Freestanding emergency dept. | −1.238 (0.791) |
| Freestanding outpatient clinic | −1.589** (0.398) |
| Outpatient surgery unit | 1.866 (2.059) |
| Urgent care clinic | −0.682 (0.431) |
| Ownership type | |
| Government, non-federal | −1.447 (0.766) |
| For-profit | 0.899 (0.852) |
| ED visits as% of outpatient visits | 0.138** (0.018) |
| Medicare length of stay | 0.795 (0.494) |
| Patient characteristics | |
| Average age | −0.190 (0.103) |
| % Male | 0.153* (0.076) |
| % Black | −0.051* (0.020) |
| % Asian | 0.118 (0.061) |
| % Hispanic | −0.087 (0.065) |
| % Other race | 0.148 (0.146) |
| % Top 10 observation diagnoses | 0.263** (0.079) |
| Local health system characteristics | |
| Physicians per 1,000 population | 0.051 (0.242) |
| Population (10,000) | 0.005 (0.007) |
| % of Beneficiaries in Medicare HMO | 0.060 (0.042) |
| No. of short-term general hospitals per 100,000 population | 0.076 (0.048) |
| Metropolitan area | 1.121 (0.675) |
| Micropolitan area | −0.031 (0.818) |
| R2 | 0.65 |
| Sample size (N) | 3,024 |
Note. Coefficients for state dummy variables are not shown here but are available by request. Robust standard errors in parentheses.
Significant at 5%;
1%.
A joint F-test finds that the construct of bed size is statistically significant, F(7, 50) = 2.26, p =.044. On average, compared to hospitals with between 100 and 199 beds, smaller hospitals (25–49 beds) have 1.6 fewer observation stays per 1,000 visits, and larger hospitals (300–399 beds) have 2.3 more observation stays per 1,000 visits. Additionally, the greater the proportion of a hospital's outpatient visits that occur in the emergency department, the higher the hospital's observation stay prevalence. A 10 percentage point increase in the emergency department proportion of outpatient visits is associated with an increase of 1.4 observation stays per 1,000 visits—a 10 percent increase relative to the mean.
Among the patient characteristics, primary diagnosis has the strongest association with the prevalence of observation stays. Recalling that the measure we use captures the proportion of a hospital's outpatient visits with a primary diagnosis that is one of the ten most common diagnoses among patients held for observation, we find that a 10 percentage point increase in this figure is associated with an increase of 2.63 observation stays per 1,000 visits. The magnitude of this effect is nontrivial, as it represents nearly a 20 percent increase relative to the conditional mean prevalence of observation stays. Other patient characteristics are less instructive. Neither age nor gender is a significant predictor of observation stay prevalence. While a joint F-test of the construct of race was statistically significant, F(4, 50) = 4.31, p =.0045, patient mix by race is significant for blacks, but not other races. Specifically, each 10 percentage point increase in the proportion of a hospital's patients who are black is associated with a decrease of 0.51 observation stays per 1,000 visits. None of the local health system characteristics are significant predictors of the prevalence of observation stays.
Conditional Duration of Observation Stays
The results of the linear regression model predicting the average duration of observation stays among hospitals providing any observation care are shown in Table 4. Despite clinical guidelines suggesting that most observation stays can be resolved within 24 hours (Baugh, Venkatesh, and Bohan 2011), our data indicate that among the 3,024 hospitals providing any observation care, the mean duration of observation stays is 25.9 hours and 63.1 percent of these hospitals have average observation stays longer than 24 hours.
Table 4.
OLS Model Predicting Hospital-Level Average Duration of Observation Stays
| Coefficient | |
|---|---|
| Hospital characteristics | |
| Bed count | |
| 6–24 | −0.479 (0.749) |
| 25–49 | −0.952* (0.458) |
| 50–99 | −0.341 (0.459) |
| 200–299 | 0.410 (0.429) |
| 300–399 | 0.582 (0.709) |
| 400–499 | −0.280 (0.542) |
| 500+ | −1.237 (0.991) |
| Medical school affiliation | −0.478 (0.423) |
| Critical access hospital | −2.813** (0.574) |
| Freestanding emergency dept. | 0.230 (0.833) |
| Freestanding outpatient clinic | 0.174 (0.248) |
| Outpatient surgery unit | 1.611 (0.817) |
| Urgent care clinic | −0.203 (0.348) |
| Ownership type | |
| Government, non-federal | −1.542** (0.281) |
| For-profit | −2.046** (0.495) |
| ED visits as% of outpatient visits | 0.007 (0.007) |
| Medicare length of stay | 1.781** (0.195) |
| Patient characteristics | |
| Average age | 0.262** (0.030) |
| % Male | −0.061 (0.032) |
| % Black | −0.010 (0.016) |
| % Asian | 0.045* (0.020) |
| % Hispanic | −0.009 (0.042) |
| % Other race | −0.101* (0.044) |
| % Top 10 observation diagnoses | 0.018 (0.034) |
| Local health system characteristics | |
| Physicians per 1,000 population | −0.369 (0.197) |
| Population (10,000) | −0.004 (0.002) |
| % of Beneficiaries in Medicare HMO | 0.016 (0.018) |
| No. of short-term general hospitals per 100,000 population | −0.008 (0.031) |
| Metropolitan area | 1.646** (0.484) |
| Micropolitan area | 0.862 (0.434) |
| R2 | 0.94 |
| Sample size (N) | 3,024 |
Note. Coefficients for state dummy variables are not shown here but are available by request. Robust standard errors in parentheses.
Significant at 5%;
1%.
Several hospital characteristics are significant predictors of the amount of time Medicare beneficiaries are held for observation care. The largest effects were observed for ownership type and critical access hospital status. In particular, government-owned hospitals have average stays 1.5 hours shorter, and for-profit hospitals have average stays 2 hours shorter, than nonprofit hospitals. Compared to other general hospitals, critical access hospitals have average stays that are 2.8 hours shorter. According to the results of a joint F-test, the construct of bed size is a significant factor, F(7, 50) = 2.62, p =.0219, although the only individual measure that was significant was for hospitals with 25–49 beds, which have stays that are approximately 1 hour shorter than those in hospitals with between 100 and 199 beds. Hospitals with a longer inpatient length of stay for Medicare beneficiaries also have longer observation stays on average. A 1 day increase in Medicare length of stay is associated with a 1.8 hour increase in the average duration of observation stays.
The only patient characteristic significantly associated with the average duration of observation stays is age. Specifically, the older a hospital's Medicare outpatient population is, the longer their observation stays last. A 1 year increase in average age is associated with an 0.26 hour (∼16 minute) increase in the duration of observation stays. While this is a statistically significant finding, the practical significance of the result is less certain, given that there is not tremendous variation in average age across hospitals in the sample. While the individual coefficients on the proportion of a hospital's outpatients who are black and the proportion who are Asian are individually significant, the results of a joint F-test indicate that the construct of patient-mix by race is not significant, F(4, 50) = 1.95, p =.1165. Likewise, patient gender is not a significant predictor of the duration of observation stays at the hospital level. Finally, local health system characteristics are not significant predictors of observation stay duration, although hospitals in metropolitan areas have average stays that are 1.6 hours longer than hospitals in rural areas.
Discussion
The high degree of interhospital variation observed in the use of observation care is consistent with the small-area variation routinely observed in analyses of Medicare cost and utilization data (Fisher et al. 2003a,b). Our results indicate that different factors are involved in whether a hospital provides observation care, how much observation care a hospital provides once it offers that service, and how long, on average, a hospital tends to hold patients for observation.
The likelihood of a hospital having any observation stays depends mostly on the hospital's critical access status and bed size, while ownership type, case mix by diagnosis, and local health system characteristics are not important factors. This suggests that certain hospital factors may play a dominant role in the hospital administration's decision to begin billing for observation care. Although the optimal amount of observation care is unknown, our results suggest that Medicare beneficiaries living in areas served by small and/or critical access hospitals have less access to this type of care, which may mean that they are more likely to be admitted unnecessarily or discharged home prematurely. It is difficult to know with certainty why these hospitals would opt not to provide any observation care, but differences in Medicare payment policy between critical access hospitals (CAHs) and prospective payment system (PPS) hospitals may play an important role (Hale 2008; Wright et al. 2013).
Once a hospital opts to provide observation care, the amount of observation care that hospital provides seems to depend heavily—although not entirely—on clinical factors. Hospitals with the highest prevalence of observation stays per 1,000 visits are those who see a large share of their outpatients in the emergency department and have a large share of those outpatients present at the emergency department with one of ten primary diagnoses most frequently seen among patients held for observation. However, even after controlling for case mix, we find that CAHs have a lower prevalence of observation stays.
In a prior descriptive study, CAHs providing any observation care were shown to have a higher ratio of observation stays to inpatient admissions compared to PPS hospitals. However, the results of this study, which models the prevalence of observation stays among all inpatient and outpatient visits, indicate that CAHs providing any observation care actually provide three fewer observation stays per 1,000 visits compared to PPS hospitals. While these findings initially appear to be contradictory, the reality is that, compared to PPS hospitals, CAHs provide a much higher volume of outpatient care relative to inpatient care. Considered jointly, this suggests that, compared to PPS hospitals, a smaller fraction of outpatient visits at CAHs result in an observation stay. One reason for this may be the tendency for higher acuity patients to bypass their local CAH (Liu, Bellamy, and McCormick 2007).
While both the Medicare Recovery Audit Contract (RAC) and Hospital Readmissions Reduction Programs were not fully implemented until after our study period, both of these programs are likely to drive hospitals to further increase their use of observation care. Unnecessary short-stay hospitalizations have been a key target for the Medicare Recovery Audit Contractor Program, suggesting that previously observed increases in the prevalence of observation stays and accompanying decreases in inpatient admissions may be hospitals' response to being penalized for unnecessary hospitalizations (Robin and Gershwin 2010; Centers for Medicare and Medicaid Services 2012b; Feng, Wright, and Mor 2012). To the extent that longer observation stays are substitutes for short-stay inpatient admissions, our results suggest that substitution of observation care for inpatient admissions is more likely to occur in nonprofit hospitals than in either government-owned or for-profit hospitals. It is not surprising that for-profit hospitals have a shorter duration of observation stays. Keeping every patient under observation for just the minimum 8 hours required for facility reimbursement is maximally profitable, as hospitals are not reimbursed separately for stays less than 8 hours and do not receive an additional payment for stays in excess of 8 hours (Baugh, Venkatesh, and Bohan 2011). The shorter duration of observation stays seen in government-owned hospitals may have resulted from a similar push for efficiency given limited budgets and capacity constraints. The substitution of observation care for inpatient admissions is likely to increase further in coming years, as financial penalties for excessive hospital readmission rates have been implemented since October 2012 under the Affordable Care Act, potentially incentivizing hospitals to use observation stays rather than readmit patients (Medicare Payment Advisory Commission 2012).
In all three models, the state effects (data not shown) were jointly significant, indicating that significant variation in the likelihood, prevalence, and duration of observation care remains between states even after controlling for hospital characteristics, patient characteristics, and local health system characteristics. This suggests that unobserved state-specific characteristics, such as different practice patterns and organizational culture, are important determinants of whether a hospital provides any observation care, how much observation care they provide, and how long they tend to keep patients. This may also relate to the proportion of hospitals in each state that are critical access hospitals, as our results indicate that these facilities are much less likely to provide observation care, have a lower prevalence of observation stays, and have a shorter average duration of observation stays. Thus, prior findings of significant interstate variation in observation care are not entirely or even primarily driven by interhospital variation (Feng, Wright, and Mor 2012).
Limitations
This study has some limitations. The cross-sectional nature of our study precludes us from making causal inferences. While additional years of claims data are available, hospital characteristics are relatively stable over brief periods, limiting our ability to employ a model with hospital fixed effects. Our analysis does not allow us to assess whether the observed patterns of observation care are clinically appropriate. While observation stays of extended duration are likely cause for concern, we do not have the data to conclude that they were unnecessary. In all cases, observation stays in excess of 24 hours are unlikely to be cost-effective (Zun 1990). However, our analysis does not account for length of stay in the emergency department, and to the extent that different hospitals have different tolerances for prolonged stays in the emergency department, this could affect the duration of observation stays we observe in these data.
It is also important to note that RAC audits and the Hospital Readmission Reduction Program were not fully implemented nationwide until 2010 and 2012, respectively. It is anticipated that both of these programs will lead to an increase in the use of observation care beyond already observed trends, and because our analyses used 2009 data, our estimates of observation care may be conservative compared to current levels. Future studies extending our work using a pre–post design around these important nationwide policy changes would be particularly valuable.
Finally, although our study is able to partially explain the interhospital variation in observation care, we are unable to ascertain the effect that these differences have on individual Medicare beneficiaries. While beneficiaries at hospitals with a higher prevalence and duration of observation stays are unquestionably subject to a higher out-of-pocket cost burden, for example, we do not calculate these costs here.
Conclusion
The variation between hospitals in the likelihood, prevalence, and duration of observation stays depends on a variety of hospital and patient characteristics, as well as unobserved state-level characteristics. Our findings suggest that critical access hospitals and hospitals with fewer than 100 beds in micropolitan areas are the least likely to provide observation care. We also find that, among hospitals that provide observation care, the prevalence of observation stays is lower at critical access hospitals but does depend heavily on a hospital's case mix. Finally, we found that critical access, government-owned, and for-profit hospitals have shorter average observation stays. While our study is able to explain a significant amount of the interhospital variation in observation care, more work is needed to fully understand the clinical and financial implications this variation has for both beneficiaries and hospitals.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This work was funded by the Retirement Research Foundation (grant no. 2011-066), the National Institute on Aging (grant no. P01AG027296), and the Agency for Healthcare Research and Quality (grant no. 5T32H000011-27). The Medicare enrollment and claims data used in this analysis were made available through a data use agreement (DUA 21845) authorized by the Centers for Medicare and Medicaid Services.
Disclosures: None.
Disclaimers: None.
Supporting Information
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
References
- Armstrong D. “Medicare Fraud Effort Gives Elderly Surprise Hospital Bills”. Bloomberg. 2010 [accessed on July 5, 2012]. Available at http://www.bloomberg.com/news/2010-07-12/hospital-fraud-audits-spur-unintended-cash-penalty-to-elderly-on-medicare.html. [Google Scholar]
- Baugh CW, Venkatesh AK. Bohan JS. “Emergency Department Observation Units: A Clinical and Financial Benefit for Hospitals”. Health Care Management Review. 2011;36(1):28–37. doi: 10.1097/HMR.0b013e3181f3c035. [DOI] [PubMed] [Google Scholar]
- Center for Medicare Advocacy. 2010. “Extended Observation Stays in Acute Care Hospitals: Criticism, Legislation, and Discussion” [accessed on July 5, 2012]. Available at http://www.medicareadvocacy.org/2010/08/extended-observation-stays-in-acute-care-hospitals-criticism-legislation-and-discussion/
- Center for Medicare Advocacy. 2011. “Press Release, Congressman Joe Courtney and Center for Medicare Advocacy Hold Congressional Briefing on Observation Status” [accessed on July 5, 2012]. Available at http://www.medicareadvocacy.org/2011/10/24/congressman-joe-courtney-and-center-for-medicare-advocacy-hold-congressional-briefing-on-observation-status/
- Center for Medicare Advocacy. 2012. “Déjà Vu All Over Again: CMS Decides (Again) Not to Decide about Observation Status” [accessed on September 10, 2013]. Available at http://www.medicareadvocacy.org/deja-vu-all-over-again-cms-decides-again-not-to-decide-about-observation-status/
- Centers for Medicare and Medicaid Services. 2011. “Part B Hospital (Including Inpatient Hospital Part B and OPPS).” Chap. 4 in: Medicare Claims Processing Manual Baltimore, MD CMS (Pub No. 100-04) [accessed on July 5, 2012]. Available at https://www.cms.gov/Regulations-andGuidance/Guidance/Manuals/downloads//clm104c04.pdf.
- Centers for Medicare and Medicaid Services. 2012a. “Medicare General Information, Eligibility, and Entitlement. Chapter 3—Deductibles, Coinsurance Amounts, and Payment Limitations” [accessed on December 11, 2012]. Available at http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/ge101c03.pdf.
- Centers for Medicare and Medicaid Services. 2012b. “Recovery Audit Program” [accessed on July 6, 2012]. Available at http://www.cms.hhs.gov/RAC/
- Centers for Medicare and Medicaid Services. 2013. Federal Register, Vol. 78, No. 91; Proposed Rules [Pages 27644-27650] [FR Doc No: 2013-10234]. [accessed September 10, 2013]. Available at http://www.gpo.gov/fdsys/pkg/FR-2013-05-10/html/201310234.htm.
- Cooke M, Higgins J. Kidd P. “Use of Emergency Observation and Assessment Wards: A Systematic Literature Review”. Emergency Medicine Journal. 2003;20(2):138–42. doi: 10.1136/emj.20.2.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farkouh ME, Smars PA, Reeder GS, Zinsmeister AR, Evans RW, Meloy TD, Kopecky SL, Allen M, Allison TG, Gibbons RJ. Gabriel SE. “A Clinical Trial of a Chest-Pain Observation Unit for Patients with Unstable Angina”. New England Journal of Medicine. 1998;339(26):1882–8. doi: 10.1056/NEJM199812243392603. [DOI] [PubMed] [Google Scholar]
- Feng Z, Wright B. Mor V. “Sharp Rise in Medicare Enrollees Being Held in Hospitals for Observation Raises Concerns about Causes and Consequences”. Health Affairs (Millwood) 2012;31(6):1251–9. doi: 10.1377/hlthaff.2012.0129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL. Pinder EL. “The Implications of Regional Variations in Medicare Spending. Part 1: The Content, Quality, and Accessibility of Care”. Annals of Internal Medicine. 2003a;138(4):273–87. doi: 10.7326/0003-4819-138-4-200302180-00006. [DOI] [PubMed] [Google Scholar]
- Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL. Pinder EL. “The Implications of Regional Variations in Medicare Spending. Part 2: Health Outcomes and Satisfaction with Care”. Annals of Internal Medicine. 2003b;138(4):288–98. doi: 10.7326/0003-4819-138-4-200302180-00007. [DOI] [PubMed] [Google Scholar]
- Hale DK. 2008. “Observation Status: A Guide to Compliant Level of Care Determinations. Second Edition.” HCPro, Inc. [accessed on July 6, 2012]. Available at http://www.hcmarketplace.com/supplemental/6325_browse.pdf.
- Jaffe S. 2010. “Growing Number of Patients Find a Hospital Stay Does Not Mean They're Admitted.” Kaiser Health News [accessed on July 5, 2012]. Available at http://www.kaiserhealthnews.org/Stories/2010/September/07/hospital-observation-care.aspx.
- Liu J, Bellamy GR. McCormick M. “Patient Bypass Behavior and Critical Access Hospitals: Implications for Patient Retention”. Journal of Rural Health. 2007;23(1):17–24. doi: 10.1111/j.1748-0361.2006.00063.x. [DOI] [PubMed] [Google Scholar]
- Mace SE, Graff L, Mikhail M. Ross M. “A National Survey of Observation Units in the United States”. American Journal of Emergency Medicine. 2003;21(7):529–33. doi: 10.1016/j.ajem.2003.08.012. [DOI] [PubMed] [Google Scholar]
- Medicare Payment Advisory Commission. Report to the Congress: Medicare Payment Policy. Washington, DC: MedPAC; 2012. “.” [accessed on July 6, 2012]. Available at http://medpac.gov/documents/Mar12_EntireReport.pdf. [Google Scholar]
- Morgan D. 2011. “Medicare Beneficiaries Sue U.S. over Hospital Stays.” Reuters. [accessed on September 10, 2013]. Available at http://www.reuters.com/article/2011/11/03/usa-medicare-lawsuit-idUSN1E7A21ST20111103.
- Office of Inspector General. 2013. “Memorandum Report: Hospitals' Use of Observation Stays and Short Inpatient Stays for Medicare Beneficiaries, OEI-02-12-00040.” Washington, DC [accessed on September 10, 2013]. Available at http://oig.hhs.gov/oei/reports/oei-02-12-00040.asp.
- Robin DW. Gershwin RJ. “RAC Attack—Medicare Recovery Audit Contractors: What Geriatricians Need to Know”. Journal of the American Geriatrics Society. 2010;58(8):1576–8. doi: 10.1111/j.1532-5415.2010.02974.x. [DOI] [PubMed] [Google Scholar]
- Schuur JD, Venkatesh AK. Bohan JS. “Variation in the Use of Observation Status Evaluation in Massachusetts Acute Care Hospitals, 2003–2006”. International Journal of Emergency Medicine. 2010;3(4):367–72. doi: 10.1007/s12245-010-0188-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venkatesh AK, Geisler BP, Chambers JJG, Baugh CW, Bohan JS. Schuur JD. “Use of Observation Care in US Emergency Departments, 2001 to 2008”. PLoS ONE. 2011;6(9):e24326. doi: 10.1371/journal.pone.0024326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiler JL, Ross MA. Ginde AA. “National Study of Emergency Department Observation Services”. Academic Emergency Medicine. 2011;18(9):959–65. doi: 10.1111/j.1553-2712.2011.01151.x. [DOI] [PubMed] [Google Scholar]
- Wright B, Jung H-Y, Feng Z. Mor V. “Trends in Observation Care among Medicare Fee-for-Service Beneficiaries at Critical Access Hospitals, 2007-2009”. Journal of Rural Health. 2013 doi: 10.1111/jrh.12007. doi: 10.1111/jrh.12007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yealy DM, De Hart DA, Ellis G. Wolfson AB. “A Survey of Observation Units in the United States”. The American Journal of Emergency Medicine. 1989;7(6):576–80. doi: 10.1016/0735-6757(89)90277-5. [DOI] [PubMed] [Google Scholar]
- Zun L. “Observation Units: Boom or Bust for Emergency Medicine”. Journal of Emergency Medicine. 1990;8(4):485–90. doi: 10.1016/0736-4679(90)90180-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.


