Figure 6.
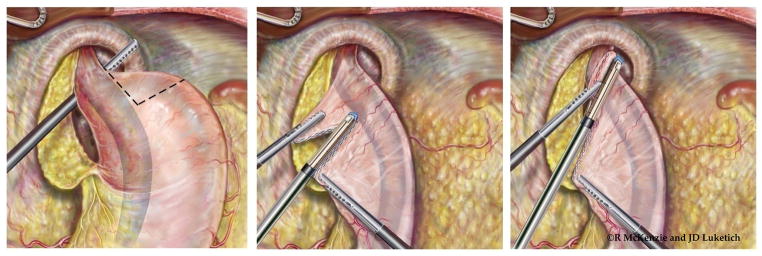
Laparoscopic wedge Collis gastroplasty. If additional esophageal length is needed following extensive esophageal mobilization, the stomach is then grasped at the short gastric vessels and rolled toward the surgeon. The surgeon determines the length of gastroplasty required to create a neoesophagus that will provide at least 2 cm of tension-free intraabdominal esophagus. A 54-french Bougie is placed by the surgeon with direct visualization with the laparoscope to ensure safe passage into the stomach. The surgeon then grasps the stomach just proximal to the planned location of the initial staple line. Depending on the thickness of the stomach, either a 4.8-mm (green load) or 3.5-mm (blue load) cutting endostapler is then applied. Serial fires of the stapler directly perpendicular to the bougie are used to divide the stomach until the staple line reaches the bougie. The surgeon and assistant provide very gentle counter-traction on the proximal and distal aspects of the stomach to draw the lesser curve tight against the bougie. This ensures that the neoesophagus is not patulous. Care must be taken to avoid traction in the cephalad or caudal direction as this can tear the stomach at the crotch of the staple line; this can be difficult to repair and increases the risk of postoperative leak from the Collis gastroplasty. The wedge of stomach is then removed with serial firings of the endostapler parallel to the bougie. (Video 3)
