Abstract
Background:
Cystatin C (Cys C) has been implicated as a prognostic marker in cardiovascular disease. The aim of this study was to evaluate the value of Cys C as a marker of acute kidney injury (AKI) in acute heart failure (AHF), the impact of Cys C and N-terminal probrain natriuretic peptides (NT-proBNP) on in-hospital and 12 months mortality were also investigated.
Materials and Methods:
A total of 162 patients with AHF were enrolled. NT-proBNP, Cys C, serum creatinine (Scr), blood urea nitrogen (BUN) and parameters of echocardiography were measured for analyze. The in-hospital and 12 months mortality was analyzed.
Results:
There was 28 (17%) of all AHF patients with AKI. Compared with no-AKI patients, the levels of Cys C (1.51 ± 0.34 vs. 1.32 ± 0.29, P = 0.003) and NT-proBNP (8163.87 ± 898.06 vs. 5922.45 ± 576.73, P = 0.001) were higher in AKI patients. Higher levels of NT-proBNP (odds ratio (OR) = 1.92, 95% confidence interval (CI): 2.19-10.98, P = 0.018, OR = 4.31, 95% CI: 2.35-9.82, P = 0.002, respectively) and Cys C (OR = 1.48, 95% CI: 1.75-4.16, P = 0.027, OR = 2.72, 95% CI: 1.92-4.28, P = 0.017, respectively) were independent association with the in-hospital and 12 months mortality. Cys C was positively correlated with NT-proBNP (r = 0.87, P < 0.001). Combining tertiles of Cys C and NT-proBNP improved risk stratification further. Compared with patients without AKIcysC, patients with AKIcysC was associated with higher in-hospital (7/28 vs. 10/134, P = 0.002) and 12-month mortality (13/28 vs. 32/134, P = 0.001).
Conclusion:
Cys C was not only a promising risk marker in patients hospitalized for AHF, but also an independent predictor of 12-month mortality. Combining tertiles of Cys C and NT-proBNP could be used to distinguish the mortality risk identification of patients with AHF. AKI was an independent predictor of in-hospital and 12-month mortality.
Keywords: Acute heart failure, acute kidney injury, cardiorenal syndrome, cystatin C, n-terminal probrain natriuretic peptides
INTRODUCTION
Studies have found that impaired renal function was common in heart failure and often associated with poor prognosis.[1,2] The pathophysiological interaction between the heart and the kidney, also termed the cardiorenal syndrome (CRS), has risen into focus due to its detrimental effect on prognosis.[3] The CRS is a clinical manifestation of the bidirectional interaction between the heart and kidneys. Evaluating renal function is an essential part of the assessment of every cardiac patient. The recognition of the importance of CRS has brought about the need for accurate and timely assessment of renal function in patients with cardiovascular disease. It has become clear that serum creatinine (Scr) is not an accurate enough marker of glomerular filtration rate (GFR).[4] Cystatin C (Cys C) is a small 13-kDa protein with properties making it a candidate for a good marker of GFR. It has been studied as a risk marker for prognosis in cardiovascular disease.[5] Acute heart failure (AHF) is a condition with significant morbidity and mortality. Acute kidney injury (AKI) is common and one of the most powerful determinants of outcome after hospitalization for AHF. The relationship of Cys C and N-terminal probrain natriuretic peptides (NT-proBNP) shown in AHF was fewer reported.[6] The purpose of this study was to evaluate the association between Cys C and NT-proBNP, which is used as a marker of cardiac stress in patients with AHF and to assess the value of Cys C as a marker of AKI in a Chinese population of patients with AHF. Further, we evaluated both the frequency of early (within 48 h) AKI in AHF as well as its impact on in-hospital outcomes and mortality during 12-month follow-up.
MATERIALS AND METHODS
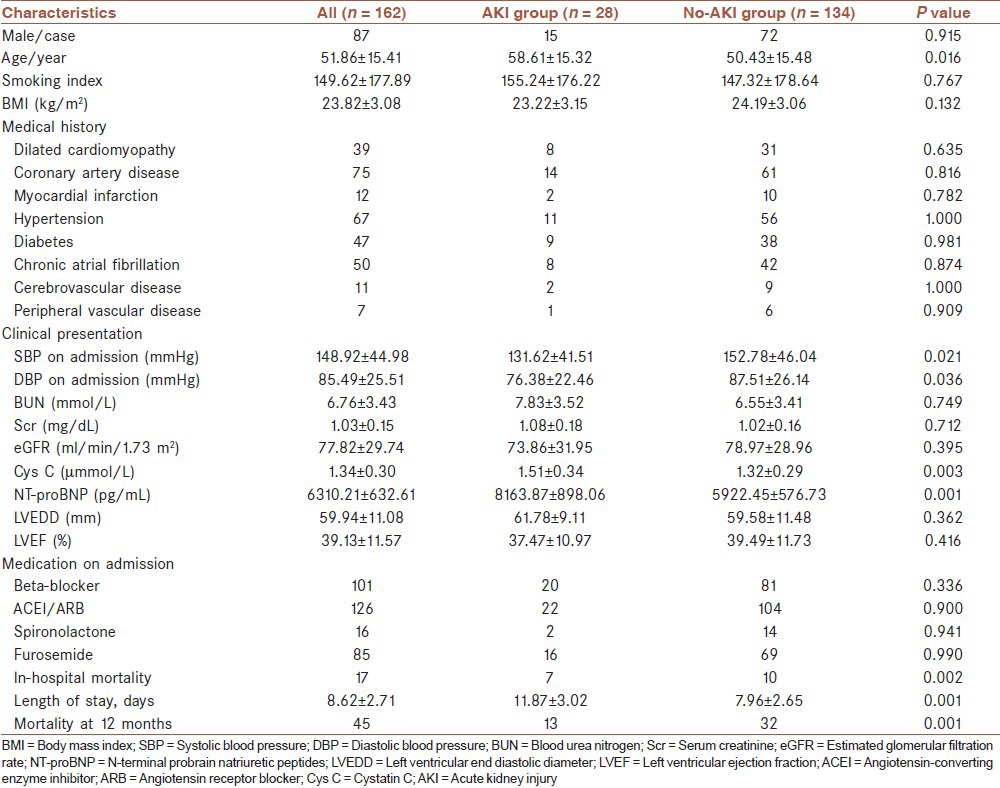
The prospective, observational and single center study was approved by the ethics committee of Taizhou People's Hospital. Written informed consent was obtained from 162 patients with AHF during hospitalization from January 2010 to October 2012. All patients presenting with symptoms, signs, and diagnostic findings of AHF, according to current European Society of Cardiology guidelines,[7] and requiring hospitalization were eligible. The diagnosis of heart failure had to be confirmed during hospital stay. Both patients with new onset (i.e., no previous history) of heart failure and with acute decompensation of CHF were included. Information about baseline characteristics (including age, sex, body mass index and history of smoking index, medical disease, clinical presentation, and medication on admission) was collected from the medical records by a special doctor and shown in [Table 1]. Smoking index was defined as the number of cigarette-years smoked.[8]
Table 1.
Characteristics of the study population
Centralized analyze of NT-proBNP was performed from blood samples obtained on admission. Differences in Cys C and creatinine levels between samples on admission and at 48 h after admission were calculated. Cys C was measured using the DakoCytomation immunoturbidimetric assay. For the definition of normal renal function, the upper limit of the reference interval recommended by the manufacturer (Cys C <1.05 mg/L) was used.[9] Plasma concentration of NT-proBNP was measured by microparticle enzyme immunoassay (NT-proBNP <125 pg/mL in adults ≤75 years of age were considered normal).[10] Scr was analyzed using commercially available kits. The simplified MDRD equation was used to estimate GFR (eGFR) from measured Scr values. eGFR (ml/min/1.73 m2) = 186 × Scr (mg/dl)-1.154 × age-0.203 (if female, ×0.742).
The performance of Cys C as a diagnostic marker of AKI was assessed by receiver operating characteristics analysis. AKI was defined as a rise in Scr by 0.3 mg/dL or more (definition of AKI suggested by the AKI Network).[11] The incidence of an increase in Cys C levels by 0.1, 0.3, and 0.5 mg/L was evaluated, and the effect on outcomes assessed.
All patients were checked with ultrasound echocardiography (Philips iE33) by a special doctor, left ventricular end-diastolic internal diameter and left ventricular ejection fraction (LVEF) were recorded.
All patients were followed for 12 months and the data were reassessed by a special doctor. The in-hospital, 3, 6, 9, and 12 months mortality was registered and length of hospital stay was calculated for patients discharged alive. For the endpoint of all-cause mortality or rehospitalized, vital status was ascertained at the end of follow-up.
Statistical analysis
Data were read and reassessed by a special doctor, and expressed as means ± standard deviation of the mean. Unpaired Student's t-test was used to compare continuous variables, and Chi-square test and Fisher's exact test were used to compare categorical variables. Significant difference in variables between groups was determined with the Fisher exact test for categorical variables and the t-test for continuous variables. Line correlation analysis was performed in correlation analysis, stepwise multiple regression and logistic regression model were used in performing multivariate analysis. All statistical tests were two-sided with a 0.05 level of significance. Statistical analyses were performed using SPSS software (version 13.0, SPSS, Inc., Chicago).
RESULTS
Study population
A total of 162 patients with AHF during hospitalization from January 2010 to October 2012 were enrolled, the diagnosis of AHF had to be confirmed during hospital stay. Information of all cases about baseline characteristics was collected from the medical records. On admission, beta-blocker medication was used by 62% of patients and 78% were taking an angiotensin-converting enzyme inhibitor (ACEI) or angiotensin receptor blocker (ARB), and at discharge 81% of the patients was on a beta-blocker and 84% taking an ACEI/ARB. The in-hospital mortality rate was 10.49% and by 12 months 45 patients (27.78%) had died. For the purpose of this study, after initial evaluation of the prevalence, diagnostic performance (sensitivity and specificity for detecting AKI), and effect on outcomes with different cut-offs, AKIcysC was defined as an increase in Cys C levels by >0.3 mg/L[4] between the two measurements for further analyses. Differences in characteristics between patients with and without AKIcysC were then assessed in Table 1.
Measured biomarkers and parameters of echocardiography compared in different acute heart failure group according to New York Heart Association classification
All AHF patients were categorized into one of two groups on the basis of New York Heart Association (NYHA) class according to acute presentation, NYHA class III group (n = 82), NYHA class IV group (n = 80). The levels of Cys C, NT-proBNP, LVEF, blood urea nitrogen (BUN) and Scr were shown in Table 2. Compared with NYHA class III group, there was significantly different of NT-proBNP and Cys C in NYHA class IV group (P < 0.05). However, there was no difference of BUN, Scr, eGFR and LVEF between the two groups.
Table 2.
Laboratory findings and parameters of echocardiography in different NYHA class group

Mortality analysis
17 of 162 (10.49%) AHF patients died during hospitalization. By 12-month follow-up, 45 patients (27.78%) had died. Compared with survivors during hospitalization and after 12-month follow-up, the patients who died were older, the values of NT-proBNP, BUN, Scr and Cys C were higher when admission. Whereas, LVEF and eGFR values were lower [Table 3]. Multivariate logistic regression analysis shows that higher levels of NT-proBNP and Cys C were independent association with higher mortality for AHF patients during hospitalization and 12-month follow-up [Table 4].
Table 3.
Clinical characteristics between death group and survival group
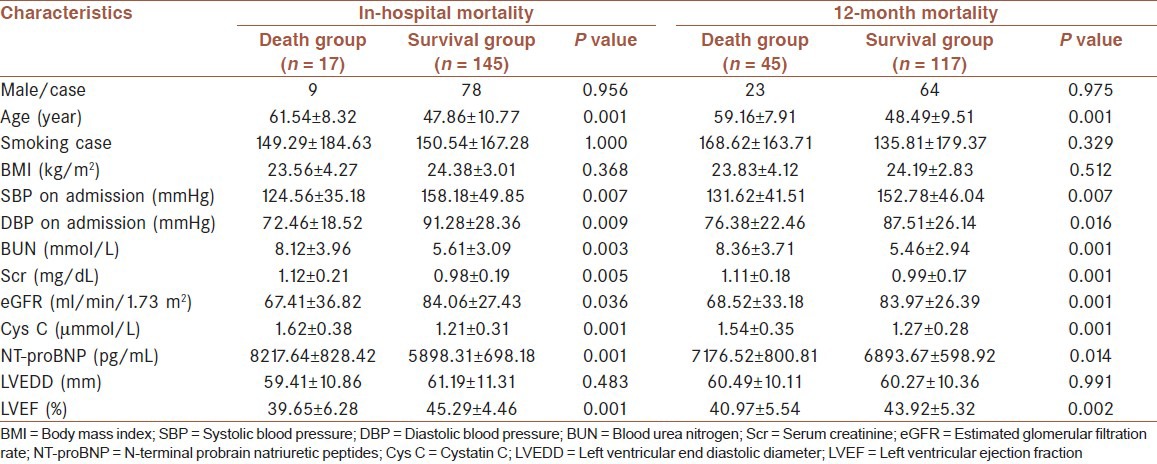
Table 4.
Multivariate logistic regression of in-hospital and 12-month mortality
Correlation analysis
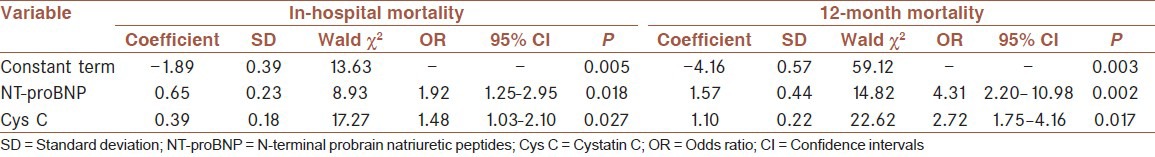
By the linear correlation analysis, Cys C was found to correlate most strongly with NT-proBNP (r = 0.87, P < 0.001). NT-proBNP and Cys C were negatively correlated with LVEF (r = −0.36, P < 0.001, r = −0.39, P < 0.001, respectively). However, there was no are no significant correlation between eGFR and LVEF (r = 0.13, P = 0.128). Categorizing patients in tertiles of Cys C and NT-proBNP yielded three separate risk groups with low, medium, and high 1-year mortality, the interaction between NT-proBNP and CsyC was further tested by examine mortality in groups with higher or lower concentrations of both biomarkers. All-cause mortality at 12 months was ranged from 3.2% in patients in the lowest tertile of both biomarkers to 52.8% in patients in the highest [Figure 1].
Figure 1.
Risk stratification in acute heart failure by combining tertiles of cystatin C and N-terminal probrain natriuretic peptides
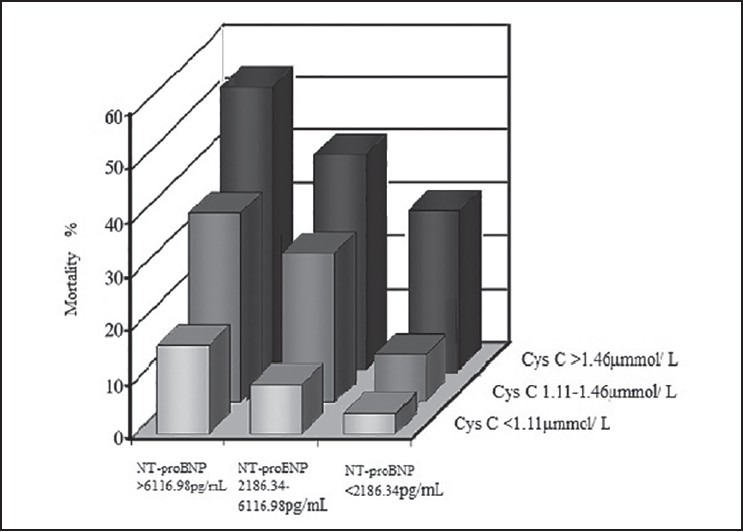
Acute kidney injury and mortality
A rise of Cys C exceeding 0.3 mg/L within 48 h from admission (AKIcysC) was associated with higher in-hospital mortality and longer hospital stay [Table 1]. Crude mortality rates during hospitalization were 25% for patients with AKIcysC and 7.5% in patients with changes in Cys C of 0.3 mg/L or less. During 12 months of follow-up, 46% of patients died in the group with compared to 24% in the group without AKIcysC. [Figure 2] shows cumulative all-cause mortality during follow-up associated with AKIcysC.
Figure 2.

Cumulative all-cause mortality associated with AKIcysC (red line indicates patients with and blue line patients without AKIcysC) AKI = Acute kidney injury, Cys C = Cystatin C
DISCUSSION
More and more studies have reported that impaired renal function is common in heart failure and associated with unfavorable outcomes. Conversely, kidney disease is independently associated with increased cardiovascular morbidity and mortality. The clinical manifestation of the bidirectional interaction between the heart and kidneys is called CRS.[12] In the CRS, heart failure leads to kidney dysfunction and/or vice versa through numerous pathways of interaction between the heart and kidney. The CRS has received much interest in recent years, which is particularly important in the diagnosis, treatment, and prognosis in patients with heart failure.[13]
Acute heart failure is characterized by diminished left ventricular systolic function and poor cardiac output triggering compensatory mechanisms such as the renin-angiotensin-aldosterone system, the sympathetic system, and other local mediators, which interact to maintain the fluid volume.
The imbalance between these compensatory mechanisms, unable to maintain adequate cardiac output results in volume overload. Furthermore, decreased renal perfusion and in addition to nephrotoxic agents and over-diuresis, eventually leads to AKI in such patients. Evaluating renal function is an essential part of the assessment of every cardiac patient. It has become clear that Scr is not an accurate enough marker of GFR and should not be used to evaluate kidney dysfunction.[14,15] Cys C has been regarded a promising novel marker of renal function for long, but only recently has the data from different clinical populations and settings been accumulating.[5,16,17,18]
In this study, it was found that there was 17% of all AHF patients with AKI, which was consistent with the report of Lassus et al.[4] Compared with no-AKI patients, the levels of Cys C and NT-proBNP were significantly higher in the AKI patients, but there was no significant difference of Bun and Scr between the two groups. Respectively, in this study, compared with NYHA class III group, there was no significant difference in the levels of BUN and Scr in NYHA class IV group, but there was significant difference in Cys C between the two group. It was showed that Cys C reflected actual GFR better than BUN or Scr, Cys C is a diagnostic index in the early kidney damage and can estimate cardiac function damage early.
N-terminal probrain natriuretic peptides is sensitive to reflect the impaired heart function and recommended as diagnostic indicators of heart failure.[19,20] This study shows that the level of NT-proBNP in NYHA class III group is significantly higher than that of NYHA class IV group, which illustrates that NT-proBNP is a strong indicator that reflects the state of cardiac function. By the linear correlation analysis, Cys C was found to correlate most strongly with NT-proBNP, NT-proBNP and Cys C were negatively correlated with LVEF, Cys C increases with severity of heart failure as measured by NYHA functional class.[21] Our results also show that there are no significant correlation between eGFR and LVEF, which is consistent with the results of the CHARM study.[22]
In this study, compared with the patients who survived during admission and follow-up, there were significantly higher levels of NT-proBNP and Cys C in patients who died, multivariate logistic regression analysis showed that the higher levels of NT-proBNP and Cys C were not only stronger impacts on short-term mortality, but also independently associated with mortality beyond 12 months, which suggested that Cys C and NT-proBNP have been independent predictors of mortality in patients with AHF even after adjustment for baseline creatinine/eGFR or after stratification by eGFR.[23] In this study, we found that, by combining tertiles of Cys C and NT-proBNP, two prognostic biomarkers in AHF, we were able to distinguish the identification of patients with very low mortality risk or high mortality risk. Worst prognosis, with a more than 10-fold increase in mortality risk, was observed in patients belonging to the highest dual biomarker tertile than that in patients with the lowest dual biomarker tertile.
There was a complex interrelation between heart and kidney in AHF patients. More and more clinical studies show that the mortality of heart failure patients with renal insufficiency is 1.81-3.04 times than that in heart failure patients without significant renal dysfunction. Consequently, the predictable intensity of renal injury on patients with heart failure is even more accurate than that of LVEF and NYHA class.[21] In our study, AKIcysC was not only associated with higher in-hospital mortality and longer hospital stay, but also associated with a higher 12-month mortality, which indicated that AKI was an independent predictor of in-hospital and 12-month mortality.
Study limitations
Like in most studies on changes in renal function, no direct measurements of GFR were available. Urine output was not recorded in this study, as measurement of urine output usually requires a urinary catheter and is difficult to perform in populations outside the intensive or coronary care units.
CONCLUSIONS
Cystatin C was a useful marker of early AKI in patients with AHF. It was not only a promising risk marker in patients hospitalized for AHF, but also an independent predictor of 12-month mortality. By combining tertiles of Cys C and NT-proBNP, we could distinguish the mortality risk identification of patients with AHF. AKI was an independent predictor of in-hospital and 12-month mortality in patients hospitalized for AHF.
AUTHORS’ CONTRIBUTION
Authors contribution (based on ICJME 2013): Zhongbao Ruan carried out the design and coordinated the study, participated all the experiments, prepared the manuscript and revised it. Li Zhu provided assistance in the design of the study, coordinated and carried out most of the experiments and participated in manuscript preparation. Yi-gang Yin and Ge-cai Chen provided assistance for all experiments and revised manuscript critically for important intellectual content. All authors have approved the version of the manuscript and the agreement to be accountable for all aspects of the study in ensuring that questions related to the accuracy or integrity of any part of the study are appropriately investigated and resolved.
ACKNOWLEDGMENT
We are thankful to Jun Ye and Wei-xiang Guo for technical assistance and Wen-qi Li for the assistance of statistical analysis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Ben-Shoshan J, Entin-Meer M, Guzner-Gur H, Keren G. The cardiorenal syndrome: A mutual approach to concomitant cardiac and renal failure. Isr Med Assoc J. 2012;14:570–6. [PubMed] [Google Scholar]
- 2.Eren Z, Ozveren O, Buvukoner E, Kaspar E, Degertekin M, Kantarci G. A Single-Centre Study of Acute Cardiorenal Syndrome: Incidence, Risk Factors and Consequences. Cardiorenal Med. 2012;2:168–76. doi: 10.1159/000337714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ronco C, Haapio M, House AA, Anavekar N, Bellomo R. Cardiorenal syndrome. J Am Coll Cardiol. 2008;52:1527–39. doi: 10.1016/j.jacc.2008.07.051. [DOI] [PubMed] [Google Scholar]
- 4.Lassus JP, Nieminen MS, Peuhkurinen K, Pulkki K, Siirilä-Waris K, Sund R, et al. Markers of renal function and acute kidney injury in acute heart failure: Definitions and impact on outcomes of the cardiorenal syndrome. Eur Heart J. 2010;31:2791–8. doi: 10.1093/eurheartj/ehq293. [DOI] [PubMed] [Google Scholar]
- 5.Lassus J, Harjola VP. Cystatin C: A step forward in assessing kidney function and cardiovascular risk. Heart Fail Rev. 2012;17:251–61. doi: 10.1007/s10741-011-9242-6. [DOI] [PubMed] [Google Scholar]
- 6.Lassus J, Harjola VP, Sund R, Siirilä-Waris K, Melin J, Peuhkurinen K, et al. Prognostic value of cystatin C in acute heart failure in relation to other markers of renal function and NT-proBNP. Eur Heart J. 2007;28:1841–7. doi: 10.1093/eurheartj/ehl507. [DOI] [PubMed] [Google Scholar]
- 7.McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2012;33:1787–847. doi: 10.1093/eurheartj/ehs104. [DOI] [PubMed] [Google Scholar]
- 8.Aslam M, Asif M, Altaf S. Estimation of smoking index for male smokers in Multan City. Pak J Nutr. 2011;10:80–5. [Google Scholar]
- 9.Yang Lin, Mei Chen, Chun-fang Wu, Piao Huang. Cystatin C and alpha-L-fucosidase in diabetic nephropathy. Lab Med Clin. 2013;10:575–6. [Google Scholar]
- 10.Bai L, Chen ZN, Liao SW, Liang Q. Application of NT-proBNP levels in the diagnosis of emergency breathing difficulties. China Mod Doct. 2012;50:24–6. [Google Scholar]
- 11.Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, et al. Acute Kidney Injury Network: Report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11:R31. doi: 10.1186/cc5713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ronco C, McCullough P, Anker SD, Anand I, Aspromonte N, Bagshaw SM, et al. Cardio-renal syndromes: Report from the consensus conference of the acute dialysis quality initiative. Eur Heart J. 2010;31:703–11. doi: 10.1093/eurheartj/ehp507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Coats CJ, Parisi V, Ramos M, Janagarajan K, O’Mahony C, Dawnay A, et al. Role of serum N-terminal pro-brain natriuretic peptide measurement in diagnosis of cardiac involvement in patients with anderson-fabry disease. Am J Cardiol. 2013;111:111–7. doi: 10.1016/j.amjcard.2012.08.055. [DOI] [PubMed] [Google Scholar]
- 14.Kshatriya S, Kozman H, Siddiqui D, Bhatta L, Liu K, Salah A, et al. The cardiorenal syndrome in heart failure: An evolving paradigm. Am J Med Sci. 2010;340:33–7. doi: 10.1097/MAJ.0b013e3181e59108. [DOI] [PubMed] [Google Scholar]
- 15.Ahmed MS, Wong CF, Pai P. Cardiorenal syndrome — a new classification and current evidence on its management. Clin Nephrol. 2010;74:245–57. doi: 10.5414/cnp74245. [DOI] [PubMed] [Google Scholar]
- 16.Jensen J, Ma LP, Bjurman C, Hammarsten O, Fu ML. Prognostic values of NTpro BNP/BNP ratio in comparison with NTpro BNP or BNP alone in elderly patients with chronic heart failure in a 2-year follow up. Int J Cardiol. 2012;155:1–5. doi: 10.1016/j.ijcard.2011.01.083. [DOI] [PubMed] [Google Scholar]
- 17.Nosaka K, Nakamura K, Kusano K, Toh N, Tada T, Miyoshi T, et al. Serum cystatin C as a biomarker of cardiac diastolic dysfunction in patients with cardiac disease and preserved ejection fraction. Congest Heart Fail. 2013;19:E35–9. doi: 10.1111/chf.12039. [DOI] [PubMed] [Google Scholar]
- 18.Premaratne E, MacIsaac RJ, Finch S, Panagiotopoulos S, Ekinci E, Jerums G. Serial measurements of cystatin C are more accurate than creatinine-based methods in detecting declining renal function in type 1 diabetes. Diabetes Care. 2008;31:971–3. doi: 10.2337/dc07-1588. [DOI] [PubMed] [Google Scholar]
- 19.Mahadevan G, Dwivedi G, Williams L, Steeds RP, Frenneaux M. Epidemiology and diagnosis of heart failure with preserved left ventricular ejection fraction: Rationale and design of the study. Eur J Heart Fail. 2012;14:106–12. doi: 10.1093/eurjhf/hfr153. [DOI] [PubMed] [Google Scholar]
- 20.Tang WH, Van Lente F, Shrestha K, Troughton RW, Francis GS, Tong W, et al. Impact of myocardial function on cystatin C measurements in chronic systolic heart failure. J Card Fail. 2008;14:394–9. doi: 10.1016/j.cardfail.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 21.Alehagen U, Dahlström U, Lindahl TL. Cystatin C and NT-proBNP, a powerful combination of biomarkers for predicting cardiovascular mortality in elderly patients with heart failure: Results from a 10-year study in primary care. Eur J Heart Fail. 2009;11:354–60. doi: 10.1093/eurjhf/hfp024. [DOI] [PubMed] [Google Scholar]
- 22.Hillege HL, Nitsch D, Pfeffer MA, Swedberg K, McMurray JJ, Yusuf S, et al. Renal function as a predictor of outcome in a broad spectrum of patients with heart failure. Circulation. 2006;113:671–8. doi: 10.1161/CIRCULATIONAHA.105.580506. [DOI] [PubMed] [Google Scholar]
- 23.Smilde TD, Hillege HL, Navis G, Boomsma F, de Zeeuw D, van Veldhuisen DJ. Impaired renal function in patients with ischemic and nonischemic chronic heart failure: Association with neurohormonal activation and survival. Am Heart J. 2004;148:165–72. doi: 10.1016/j.ahj.2004.02.007. [DOI] [PubMed] [Google Scholar]


