Abstract
Background
Treatment of traumatic knee dislocations remains controversial and challenging. Current techniques for PCL reconstruction utilize either a transtibial approach with potential risk of vascular injury from drilling toward the popliteal artery or a tibial inlay technique with prone patient positioning, which is cumbersome and adds operative time. We therefore developed a surgical technique using a supine posteromedial approach for PCL tibial inlay reconstruction for the treatment of Schenck KDIIIM (ACL/PCL/medial collateral ligament) knee dislocations. In patients undergoing this technique, we evaluated patient-reported outcome scores, ROM, stability, and complications.
Description of Technique
Tibial inlay PCL reconstructions were performed through a posteromedial approach with the patient supine, knee flexed, and hip externally rotated, thus avoiding prone patient positioning. The inlay approach uses the interval between the medial head of the gastrocnemius and the pes anserinus (gracilis and semitendinosus), with release of the semimembranosus tendon approximately 1 cm from its insertion on the tibia. Retraction of the medial gastrocnemius and semimembranosus allows access to the posteromedial aspect of the proximal tibia while protecting the neurovascular bundle.
Methods
All 11 patients sustaining a KDIIIM multiligamentous knee injury treated between 2002 and 2011 with a three-ligament reconstruction received this posteromedial approach. Seven patients were available for complete evaluation, and one completed telephone followup only. Mean followup was 6.0 years (range, 2.0–11.2 years). Clinical evaluation included Lysholm and Tegner activity scores and measurements of ROM and knee laxity. We also recorded complications.
Results
Mean Lysholm and Tegner activity scores were 81 and 4.9, respectively, with three patients returning to recreational or competitive sports. Mean knee flexion was 120° (range, 106°–137°); however, two patients had stiffness in flexion, lacking greater than 20° of flexion compared to the contralateral side. Five had less than 3 mm of translation. Three returned to the operating room, two for arthrofibrosis or painful hardware and a third for ACL reinjury requiring revision reconstruction; there were no vascular injuries.
Conclusions
Outcome scores, stability, and complications using this surgical technique were comparable to those found in other studies. The posteromedial approach for tibial inlay avoids prone positioning and the incisions are minimized, allowing safe exposure for combined medial and posterior ligament reconstruction. Further studies are needed to compare this method with others in the treatment of KDIIIM knee dislocations.
Introduction
Knee dislocations are simply defined as ligamentous disruptions with loss of continuity of the tibiofemoral articulation. A combination of tears of the ACL, PCL, medial collateral ligament (MCL), lateral collateral ligament, tendinous structures (patellar tendon, biceps femoris, etc), and other stabilizing structures are typical of knee dislocations. Traumatic knee dislocation is an uncommon but potentially devastating orthopaedic injury. Although exceptions have been reported [3, 20], the hallmark of this injury is rupture of both cruciate ligaments, often associated with a collateral ligament tear [17]. This type of injury pattern is classified as a Schenck KDIII (ACL/PCL/collateral ligament) [17]. In an internal, unpublished review of 97 knee dislocations operatively treated at our institution over an 8-year period, the KDIII injury pattern was most common, accounting for 75% of our knee dislocations.
The PCL has been referred to as the cornerstone of ligamentous stability of the knee [10], and in multiligamentous injuries, it has been our focus. Reconstruction of the PCL is a critical step in surgical treatment of the dislocated knee. Most PCL reconstruction techniques utilize both a tibial and a femoral bone tunnel for graft placement (transtibial technique). Intraoperative imaging of the tibial guide pin is recommended to ensure proper tunnel positioning. The surgeon must exercise great care during drilling of the tibial tunnel to avoid injury to the popliteal artery. The passage of the graft as it exits the posterior tibia and turns superiorly and anteriorly toward its position on the medial femoral condyle has been termed the “killer curve.” Fanelli and Edson [5] have demonstrated that the transtibial single-bundle technique provides long-term functional stability with successful return to preinjury level of activity observed in the majority of patients. Moreover, the durability of the transtibial PCL reconstruction was demonstrated at 3- to 8-year followup using stress radiography [6]. Regardless of the long-term effects of the killer curve, the acute turn from the posterior tibia to the femoral notch can complicate graft passage during PCL reconstruction.
An alternative technique for PCL reconstruction that avoids these limitations is the tibial inlay technique, with placement of the graft’s bone block anatomically on the back of the tibia [1, 11]. The most commonly described inlay technique can be cumbersome to many surgeons as it involves flipping the patient from supine to prone and back again, adding additional time with the entire leg needing to be reprepared and draped each time. Furthermore, any graft adjustments would require repositioning, adding to an already complicated and lengthy procedure. We have developed a novel method for tibial inlay using a modification of Lobenhoffer’s posteromedial approach, which allows the patient to remain in the supine position throughout the procedure [14]. This report describes our approach, the surgical technique, patient-reported outcomes, ROM and stability metrics, and complications in a series of KDIIIM knee dislocations where this technique was utilized.
Surgical Technique
The surgical technique can be viewed in a video on YouTube [16].
Patient Positioning
The patient is positioned supine on a standard operating room table with the foot of the table up. The patient is secured to the table to minimize changes in position. An examination under anesthesia is performed. A lateral leg post and bump under the contralateral hip is recommended to allow for ipsilateral hip and leg external rotation to access the back of the knee. A thigh tourniquet is placed around the operative extremity. The tourniquet is inflated when making the posteromedial approach to the tibia, as this markedly improves visualization and safety in our experience. The affected extremity is draped with adequate exposure to allow placement of necessary incisions.
Graft Choice and Preparation
An appropriate autograft or allograft tendon is selected for reconstruction of the bicruciate ligaments. We prefer to use one of the following allograft options for the PCL inlay: bone-patellar tendon-bone (BTB) allograft, quadriceps tendon-bone allograft, or Achilles tendon allograft.
For the ACL, the previous three allografts may be used or an anterior tibialis or hamstring allograft can be used as soft tissue ACL grafts, as any of these options have adequate length for ACL reconstruction. In the later patients in this series (ie, 2- or 3-year followup), we used an accessory medial approach to create a low femoral tunnel. In the earlier patients (ie, 8- or 10-year followup), the transtibial technique was utilized. With the help of an assistant, the allograft tendons are prepared simultaneously with femoral tunnel preparation. The femoral side of the PCL graft (bone plug or soft tissue) is prepared in the usual fashion. The tibial portion of the PCL allograft is fashioned to create a 25- to 35-mm × 10- to 12-mm × 5-mm-thick rectangular graft.
For the MCL, we utilize the ipsilateral semitendinosus in a modified Bosworth loop reconstruction [2]. In our experience (DCW, RCS), the use of a modified Bosworth, leaving the semitendinosus attached distally, has provided good stability, though we understand current considerations regarding anatomic reconstruction of the posteromedial component of any MCL reconstruction and the impact on improved patient function and valgus instability [12].There are various strategies that can be used to achieve functional MCL stability, including repair or plication of the posterior oblique ligament to the MCL graft. When using the approach described in this series, the semimembranosus must be repaired after being taken down. Incorporating a portion of the posterior capsule in this repair controls the rotatory component of what any MCL reconstruction must control. We attempt to recreate the femoral anatomic site of the MCL, recognizing that a staple or screw can only best estimate that position. On the tibial side, we have kept the semitendinosus attached distally. We recognize that position of the anterior limb of the tibial side of the Bosworth is not perfectly anatomic, but with the loop down from the femur, we are able to place that limb more posteriorly and thus in direct contact with the anatomic site of the superficial MCL. Also, if both sides of the graft are free, healing of the distal limbs can be problematic. The Sharpey’s fiber attachment of the anterior limb does not need to heal and creates what we believe is an advantage to having a free loop graft fixed distally.
Diagnostic and Operative Arthroscopy
The surgical procedure begins with a diagnostic and operative arthroscopy without elevating the tourniquet. Care is taken to thoroughly evaluate the knee for any concomitant injury, specifically involving the posterolateral corner. Any associated injuries such as meniscal tears or adhesions are addressed at this time.
Femoral Tunnel Preparation
Once the diagnostic arthroscopy is complete, the ACL and PCL remnants are arthroscopically débrided and the anatomic origin of the PCL is noted. We mark the center of the PCL footprint of the anterolateral bundle with a sharp curette, typically at the 10:30 position in the left knee with respect to the notch and 6 to 8 mm posterior to the articular surface. A guide wire (Beath pin) for the femoral tunnel reamer is attached to a drill and inserted through an accessory anterolateral portal created just above the lateral meniscus with the knee positioned in 90° of flexion. Under arthroscopic visualization, the tip of the guide wire is positioned in the center of PCL footprint and the guide wire is then drilled through the medial femoral condyle and out through the skin overlying the distal, medial thigh. We utilize a guide-free technique; however, this also can be done with the assistance of a PCL femoral guide. The drill is then removed and an appropriately sized tunnel reamer is placed over the guide wire and drilled across the medial cortex. The skin incision is lengthened to allow interference screw placement. The reamer size is determined by the diameter of the femoral graft, typically 10 or 11 mm. A passing suture is placed through the femoral tunnel with the loop resting on the posteromedial capsule for later retrieval with the inlay. With the knee still in 90° of flexion, the anatomic origin of the ACL on the femur is identified. The ACL femoral tunnel is then drilled and reamed in standard fashion using an accessory medial portal.
Posteromedial Approach, ACL Femoral Graft Fixation, and Tibial Inlay Site Preparation
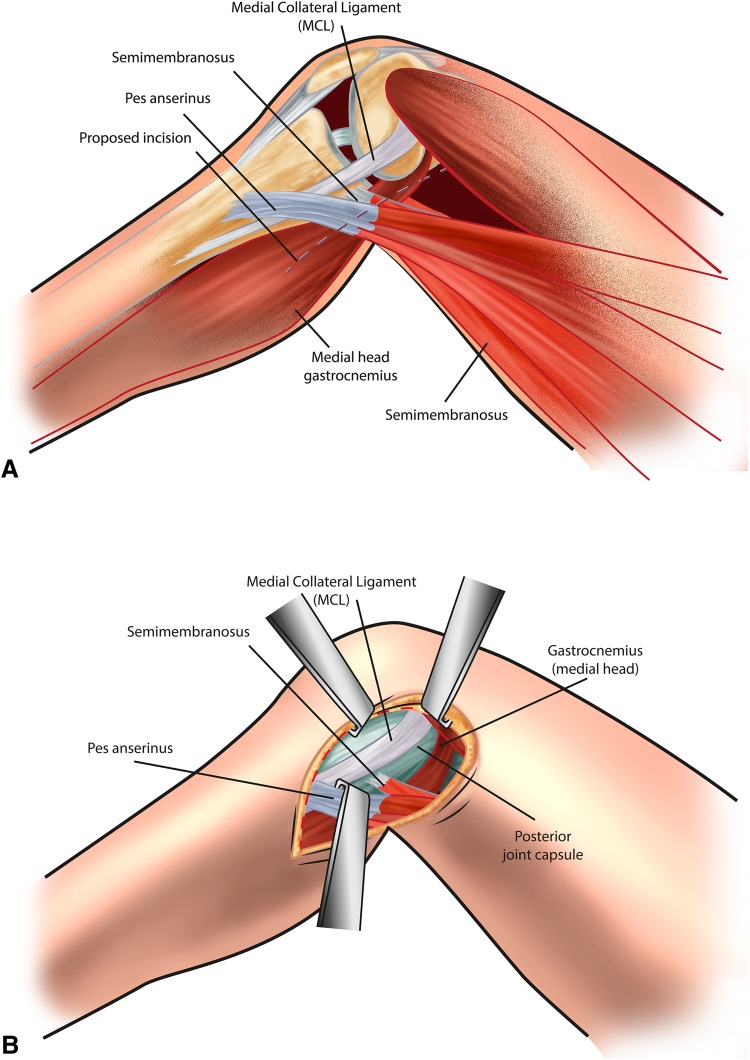
All arthroscopic instruments are removed from the knee. The leg is exsanguinated and the tourniquet inflated. The affected limb is placed in the unilateral frog leg position by flexing the knee to approximately 60° while externally rotating the hip such that the leg sits more with the heel of the patient on the operating table. This allows the surgeon to clearly and safely visualize the back of the tibia while standing on the opposite side of the table (Fig. 1) [22]. Use of a headlamp can be considered, but overhead lights are usually satisfactory. An assistant remains on the ipsilateral side of the table for retraction purposes.
Fig. 1.
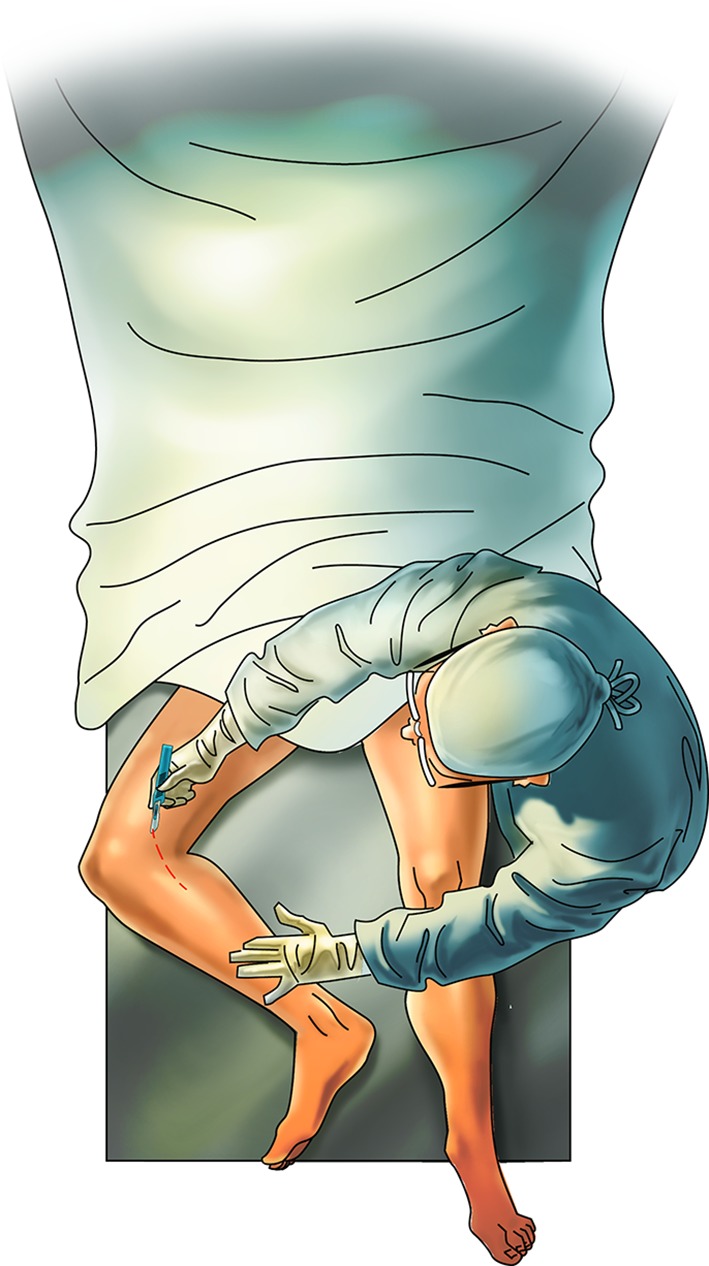
A diagram illustrates the posteromedial approach to the tibial attachment of the PCL. The patient is placed in the supine position with the knee flexed 60° and the leg and hip externally rotated.
An approximately 12-cm skin incision is made over the posteromedial aspect of the knee, overlying the posteromedial border of the tibia and centered about the posterior joint line (Fig. 1). The skin incision is along a line from the posterior edge of the tibia, in line with the medial femoral epicondyle. The sartorius fascia is identified and sharply incised, and the pes tendons are identified and retracted distally. The semitendinosus tendon is identified and released proximally with an open tendon stripper, keeping the tibial insertion intact. The semitendinosus tendon is then packed in the fat to be used later for MCL reconstruction. At this point, the ACL tibial tunnel is drilled. The ACL graft is then passed from the tibia up into the femur and fixed on the femoral side with either interference screw fixation for a BTB graft or an Endobutton® (Smith & Nephew, Inc, Memphis, TN, USA) for an ACL soft tissue graft. The tibial side is left unfixed at this point, which allows for knee manipulation and positioning without placing tension on an ACL graft that is fixed at both ends. This technique of placing the ACL graft and only fixing the femoral side allows for a quicker and more reliable reconstruction, as the posteromedial release can make arthroscopic visualization more difficult
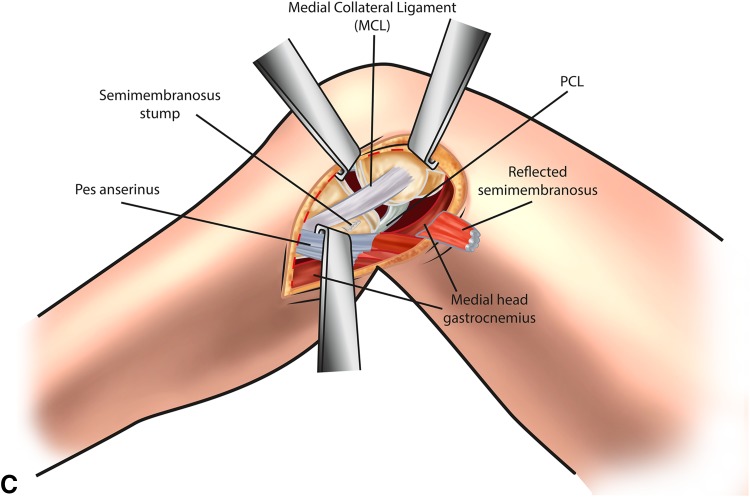
The inlay approach to the PCL origin on the back of the tibia is then completed. The interval between the medial head of the gastrocnemius and the pes anserinus (gracilis and semitendinosus) is developed. The semimembranosus is released by transecting the tendon approximately 1 cm from its insertion on the tibia (Fig. 2). Stay sutures using a Krackow configuration are placed in the proximal end of the semimembranosus tendon and it is then retracted posteriorly. Retraction of the medial gastrocnemius and semimembranosus allows access to the posteromedial aspect of the proximal tibia while protecting the neurovascular bundle. Blunt dissection is carried out medially to elevate the superior fibers of the popliteus muscle and allow exposure to the PCL tibial insertion. External rotation of the tibia facilitates the exposure.
Fig. 2A–C.
(A) A skin incision is placed at the back edge of the medial tibia, coursing proximally to the posterior edge of the medial epicondyle. Superficial dissection is made through the sartorius fascia along the line of the skin incision. (B) Deep dissection is made between the posterior knee joint capsule and the gastrocnemius. Partial detachment of the semimembranosus is required to access this interval. (C) Exposure of the proximal tibia and capsulotomy allows identification of the PCL.
Once adequate visualization is achieved, a midline trough is created using a burr starting just below the joint capsule and extending distally. If exposure is limited, the trough is angled such that proximally the PCL origin is reproduced, but distally the trough is closer to the skin incision medially on the posterior aspect of the tibia (Fig. 3). The trough dimensions are roughly 10 mm wide × 20 to 30 mm long × 5 mm deep to match the bone plug. Care is taken not to excessively deepen the trough, which can create a killer curve at the tendon-bone junction. With the operative extremity still in the unilateral frog position, a curved Kelly clamp is placed through the anteromedial portal and passed medial to the ACL; the tip allows identification for a posterior midline capsulotomy. Once the capsulotomy is made, it is distended with a Kelly clamp to accommodate the diameter of the PCL soft tissue graft.
Fig. 3.
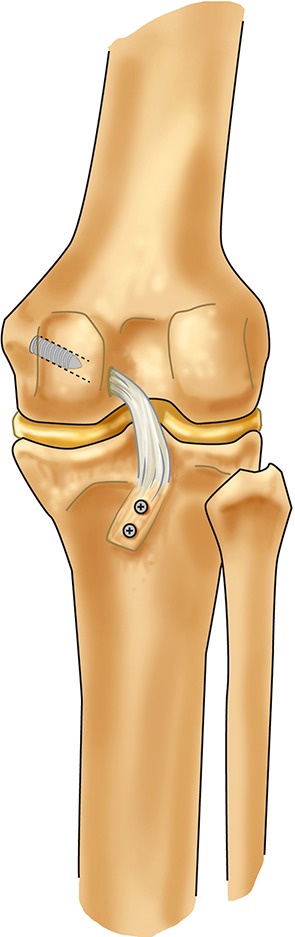
A drawing illustrates PCL reconstruction utilizing a tibial inlay technique.
PCL Tibial Graft Fixation
The tibial inlay graft is then positioned in the posterior tibial trough with the tendon-bone junction at the posterior joint line. Two 4.0-mm-diameter cannulated screw guide pins are used to secure the inlay graft in the trough. The trajectory for the guide pins should be directed slightly laterally to avoid penetrating the ACL tibial tunnel. The first guide pin is then overdrilled, and a 4.0-mm-diameter cannulated screw is placed. Finally, the other guide pin is drilled and the second screw placed to obtain secure tibial fixation. We typically use 46-mm-length, 4.0-mm-diameter fully threaded cannulated screws.
Once the inlay is fixed, a right angle clamp is used to retrieve the loop of suture placed through the femoral tunnel. It is grasped and pulled through the back of the knee. The traction sutures on the soft tissue portion of the inlay are placed in the loop. Traction is placed on the passing suture and the proximal end of the graft is pulled into the intercondylar notch, out the femoral tunnel, and through the skin over the medial distal thigh (Fig. 4).
Fig. 4.

An intraoperative photograph demonstrates the posteromedial approach to the PCL.
PCL Femoral Graft Fixation
With the tibial side of the allograft secured, the knee is brought out of the figure-of-four position and flexed over the side of the operating table. The arthroscope is placed back into the knee and the proximal end of the graft pulled into the femoral tunnel. Because a capsulotomy has been made, it is usually performed dry to visualize graft passage. The PCL graft is then tensioned and fixed at 70° of flexion.
ACL Tibial Graft Fixation
Once the PCL is fixed, the ACL graft is then ranged to minimize graft laxity. The graft is tensioned and the tibial side is secured with the knee in slight flexion.
MCL Graft Fixation
The medial femoral epicondyle is then exposed through the medial incision. Using a modified Bosworth loop reconstruction technique, the semitendinosus graft is passed proximally to this point and fixed with a staple or spiked soft tissue washer. It is then brought back down to the insertion of the superficial MCL under the pes anserine and fixed distally on the tibial side using a second staple with the knee in 30° of flexion.
Postoperative Rehabilitation Protocol
In general, we keep our patients with KDIIIM reconstruction nonweightbearing for a total of 6 weeks to allow all soft tissues to heal after a major orthopaedic operation. They are initially protected in a postoperative brace locked in extension for the first 2 weeks. We then allow ROM from full extension up to 70° of flexion from Weeks 2 through 6. After Week 6, full active and passive ROM is allowed. We typically do not allow jogging for a minimum of 3 months postoperatively. Although some patients may be able to return to heavy labor or sports at 6 months from surgery, these complex reconstructions more often take 9 to 12 months of recovery.
Patients and Methods
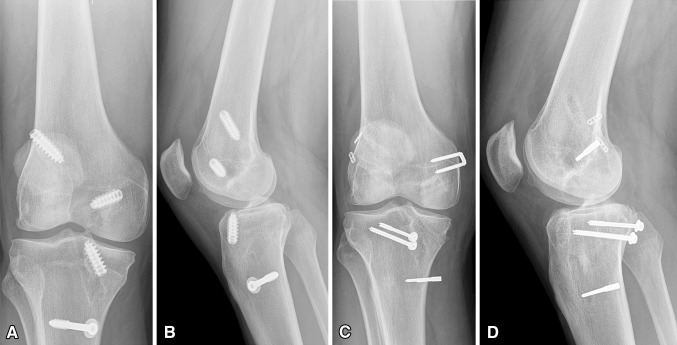
The modified inlay approach detailed above was first devised for PCL-only reconstructions to avoid potential problems with graft passage (ie, killer curve) and difficulty with patient positioning (ie, prone). Since then, the indications have broadened to include patients sustaining a KDIIIM multiligamentous knee injury. For this case series, eligible patients included those who had a PCL inlay as part of treatment for KDIIIM injuries, with a minimum 2-year followup at the senior author’s current site of practice. All 11 patients who sustained a KDIIIM multiligamentous knee injury and were treated by the senior author (RCS) between 2002 and 2011 underwent an inlay reconstruction through this posteromedial approach and were thus eligible for evaluation here. Seven patients were available for complete evaluation, and one additional patient completed a telephone survey (Table 1). Three of 11 patients were lost to followup despite vigorous efforts to make contact. The mean followup was 6.0 years (range, 2.0–11.2 years). The mean age at the time of injury was 28 years (range, 16–39 years). Six were males and two females. None of the patients had a neurovascular injury at the time of injury. The timing of reconstruction was greater than 6 weeks in six patients, once swelling had subsided and they had regained ROM. One patient was treated in the acute period (3 weeks) by another surgeon with standard ACL and PCL reconstruction utilizing a transtibial approach. This patient developed graft laxity requiring revision ACL reconstruction, revision PCL reconstruction utilizing a tibial inlay graft, and MCL reconstruction approximately 18 months from his index procedure (Fig. 5). The study was approved by the Human Research Review Committee for the University of New Mexico Health Sciences Center.
Table 1.
Patient characteristics
| Patient | Age at time of injury (years) | Sex | Followup (years) | Mechanism | Timing of reconstruction |
|---|---|---|---|---|---|
| 1 | 29 | Male | 4.1 | Skiing | Acute |
| 2 | 29 | Male | 3.0 | Hit by bulldozer | Late |
| 3 | 33 | Male | 2.0 | Cattle injury | Late |
| 4 | 23 | Male | 4.3 | Basketball | Late |
| 5 | 39 | Female | 9.5 | Pedestrian vs motor vehicle collision | Late |
| 6 | 16 | Female | 11.2 | Motor vehicle collision | Late |
| 7 | 19 | Male | 9.3 | Football | Acute |
| 8 | 39 | Male | 4.2 | Mixed martial arts | Late |
Fig. 5A–D.
(A) AP and (B) lateral radiographs show a KDIIIM injury initially treated with transtibial PCL reconstruction. (C) AP and (D) lateral radiographs show the knee after conversion to inlay PCL reconstruction with double-bundle ACL reconstruction after failure of both primary ACL and PCL grafts.
The patients underwent a comprehensive clinical evaluation involving both subjective and objective measures. Subjective measures included self-administration of the Lysholm scale and Tegner activity score.
Objective measures included a comprehensive knee examination (utilizing the 2000 IKDC Knee Form) performed by a sports medicine fellow (TTN) who was not involved in any of the surgeries. KT1000™ arthrometer (MEDmetric Corp, San Diego, CA, USA) measurements were performed by an experienced examiner (JD) who also was not involved in the surgical management. As past studies have found it difficult to accurately reproduce a neutral tibiofemoral step-off during arthrometer testing, we instead measured the total AP displacement (89 N and 133 N) at 20° and 70° of knee flexion [24]. Physical therapy functional testing included the single-legged hop test for distance, a timed single-hop test, and a triple-hop test for distance.
Radiographic followup was utilized in all patients to evaluate primarily for the development and progression of arthritis in the injured knee. The Kellgren-Lawrence grading scale was used to grade the osteoarthritis. Furthermore, stress radiography was performed utilizing the technique described by Schulz et al. [18] for grading and classification of PCL lesions. With the knee in 90° of flexion, a posteriorly directed force of 150 N was applied at the level of the tibial tubercle with use of the Telos® stress radiographic device (Telos, Marburg, Germany). Then, a lateral radiograph was taken from medial to lateral. The stress radiograph was performed on both the surgical and nonsurgical knees for a total of two lateral radiographs. The difference in posterior tibial displacement between the knees was then measured and compared.
Results
The mean Lysholm score was 81 (range, 58–100) and the mean Tegner activity score was 4.9 (range, 2–7), with three of the eight patients returning to recreational or competitive sports (Table 2).
Table 2.
Subjective and objective assessment results and complications
| Patient | Complications | Subjective assessment scores | Objective assessment scores | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lysholm score (points) | Tegner activity level (0–10) | IKDC objective score | ROM (°) | KT1000™ difference* (mm) | Single-hop distance (%)* | 6-m timed hop (%)* | Triple-hop distance (%)* | Crossover hop distance (%)* | Global PT average (%)* | ||||||
| Involved | Uninvolved | 20° | 70° | ||||||||||||
| Extension | Flexion | Extension | Flexion | ||||||||||||
| 1 | None; revision case: failed initial reconstruction done elsewhere | 100 | 5 (heavy labor) | C | 0 | 137 | 5 | 138 | 0 | 1.8 | 95 | 100 | 91 | 99 | 96 |
| 2 | Arthrofibrosis requiring MUA | 72 | 4 (moderate labor) | D | 0 | 110 | 0 | 138 | 4.5 | 5.2 | 57 | 65 | 60 | 83 | 66 |
| 3 | None | 93 | 5 (heavy labor) | B | 2 | 122 | 0 | 135 | 5.7 | 3.3 | 101 | 86 | 73 | 84 | 86 |
| 4 | Reinjury with revision ACL reconstruction | 80 | 4 (moderate labor) | B | 0 | 136 | 0 | 140 | 2.5 | 2.3 | 102 | 79 | 100 | 106 | 97 |
| 5 | Hardware removal, lateral release | 58 | 2 (light labor) | C | 4 | 117 | 0 | 138 | 0.3 | 0.3 | 87 | 67 | 84 | 79 | |
| 6 | None | 85 | 6 (recreational sports) | B | 11 | 114 | 10 | 123 | 2.8 | 3.5 | 41 | 36 | 78 | 82 | 59 |
| 7 | None | 94 | 6 (recreational sports) | B | 0 | 106 | −1 | 116 | 0.8 | 2.3 | 98 | 100 | 93 | 105 | 99 |
| 8 | None | 63 | 7 (jumping sports) | ||||||||||||
| Patient | Imaging | |||
|---|---|---|---|---|
| Kellgren-Lawrence grade | Difference in PCL laxity on lateral stress radiographs (mm)* | |||
| Involved | Uninvolved | |||
| 1 | II | 0 | 1 | |
| 2 | 0 | 0 | ||
| 3 | 0 | 0 | 9 | |
| 4 | III | 0 | 6 | |
| 5 | III | 0 | 3 | |
| 6 | III | 0 | 2 | |
| 7 | I | 0 | 8 | |
| 8 | ||||
* Compared to uninvolved side; global PT average = average of scores from combined physical therapy tests; MUA = manipulation under anesthesia.
Mean knee ROM was from 2° of extension (range, 0°–11°) to 120° of flexion (range, 106°–137°). Two patients had stiffness in flexion, lacking greater than 20° of flexion compared to the contralateral side (Table 2). No knees were rated as normal according to the IKDC objective score, primarily due to increased AP laxity of 3 to 5 mm or the presence of crepitus. One knee was rated as severely abnormal, as it lacked greater than 25° of flexion compared to the contralateral side. Five patients had less than 3 mm of translation on the KT1000™ when compared to the contralateral side. On hop testing, two patients had significant limitations.
Of the six patients undergoing stress radiographs, three had less than 3 mm of posterior translation. Three patients had at least moderate arthritis present on radiographs. These patients were also noted to have three of the four longest followups in the group (4.3–11.2 years). One patient with 9.3-year followup demonstrated minimal arthritis compared to the contralateral knee. The two patients with the shortest followup (2.0–3.0 years) did not have any discernible osteoarthritic changes on imaging when compared to the contralateral side.
Three patients underwent additional procedures (Table 2): one patient required revision ACL reconstruction at 3 years after a new injury sustained while jumping off a truck, one patient developed arthrofibrosis requiring manipulation under anesthesia, and one patient required removal of painful hardware greater than 1 year out from surgery. There were no neurovascular injuries or infections.
Discussion
Knee dislocations are uncommon and difficult injuries to treat. The potentially devastating consequences and seriousness of these injuries have been well documented [7, 9]. The goal of creating a stable and functional knee can be challenging, with reconstruction of the PCL being a critical step in the surgical treatment of the dislocated knee. Current techniques for PCL reconstruction utilize either a transtibial approach with potentially complicated graft passage around the killer curve in addition to risk of vascular injury with drilling toward the popliteal fossa or a tibial inlay technique with prone patient positioning, which may be cumbersome to many surgeons and adds operative time. Given these perceived limitations, the senior author developed a surgical technique using a supine posteromedial approach for PCL tibial inlay reconstruction for the treatment of KDIIIM multiligamentous knee injuries. In this surgical technique paper, we present our initial results using this technique, with specific attention focused on patient-reported outcomes, ROM and stability metrics, and complications in a small series of patients.
Our study is subject to a few important limitations. First, we have only a small number of patients, which limits the generalizations that can be made to a larger patient population. Three of 11 patients were lost to followup despite vigorous efforts to make contact. One of the study patients was available for telephone followup only, as he lives out of state. As the loss to followup rate increases, the impact of the nonresponder bias is more pronounced, thus impacting the validity of the inferences drawn from the study. Also, we do not have subjective assessments for preoperative comparison, which introduces a recall bias in the patient’s ability to appropriately remember the function and limitations of their knee before injury and surgical intervention.
The findings in this small patient series are generally in agreement with those of other studies. Fanelli and Edson [5] reviewed a series of 35 patients treated with bicruciate reconstruction utilizing a transtibial PCL and variable collateral ligament reconstruction or bracing. In their series, the mean Lysholm score was 91. In a review of 13 knee dislocations treated by the senior author with the transtibial PCL technique at a previous institution, the mean Lysholm score was 82 [23]. Wascher et al. [24] reviewed the results in 13 patients who underwent simultaneous allograft reconstruction of both the ACL and PCL with a transtibial technique after a knee dislocation (nine acute and four chronic injuries). Seven patients sustained related MCL injuries and six patients had posterolateral corner injuries. At followup evaluation (mean 38 months), only one patient described the reconstructed knee as normal and the mean Lysholm score was 88. Six patients had returned to unrestricted sports activities and four had returned to modified sports. Spiridonov et al. [21] evaluated a cohort of 31 patients who underwent double-bundle PCL reconstruction with endoscopic placement of femoral tunnels, finding an increase in the IKDC subjective score from a mean of 39 preoperatively to 74 postoperatively at a mean followup of 2.5 years. MacGillivray et al. [15] compared tibial inlay versus transtibial techniques for isolated PCL reconstruction in a series of 20 patients. At followup evaluation (mean 68 months), 90% of patients were satisfied with their surgery. The mean postoperative Tegner score was 6.0 for each PCL reconstruction technique and the mean Lysholm scores were 76 (inlay) and 82 (endoscopic).
Several of the above studies and others have also evaluated patient ROM and stability metrics. Spiridonov et al. [21] noted the mean posterior tibial translation on posterior stress radiographs of the knees was 15 mm preoperatively and improved to 0.9 mm postoperatively [21]. In the review of Wascher et al. [24], of the 13 patients who underwent simultaneous allograft reconstruction of both the ACL and PCL with a transtibial technique, IKDC ratings were six nearly normal, five abnormal, and one severely abnormal. The mean ROM was 130° with a mean loss of flexion of 4.7° and the mean AP excursion on KT1000™ arthrometer measurements was 4.6 mm at 20° of flexion. MacGillivray et al. [15] noted a mean KT1000™ measurement of 5.5 mm (inlay) and 5.9 mm (endoscopic). Cooper and Stewart [4] have demonstrated good results with the inlay technique. In a review of 41 patients with isolated or combined (multiligament) PCL reconstruction using the tibial inlay technique, the posterior drawer was graded as 0 or 1+ in 34 of the patients with a mean improvement of at least two grades of translation compared to preoperative evaluation. Posterior stress radiographs demonstrated a mean side-to-side difference of 4.11 mm. The final IKDC ratings were 10% normal, 59% nearly normal, 27% abnormal, and 4% severely abnormal. In three studies in which patients were evaluated using the IKDC score, none of the knees were rated as normal at the time of study evaluation [8, 13, 25]. Overall, 39% were nearly normal, 40% were abnormal, and 21% were severely abnormal.
It is important to note that, although many patients achieved good stability in this small case series, these are still not “normal” knees, as either laxity or stiffness may have persisted, three of the patients underwent repeat surgery, and arthritis was common in these patients, particularly in those patients further out from surgery. It is unknown whether this is due to the injury itself, the surgical procedure, or both. The most common complications reported elsewhere are joint stiffness and failure of some component of the reconstruction leading to persistent laxity. In the review of Wascher et al. [24] of the 13 patients, two underwent manipulation for arthrofibrosis. Shapiro and Freedman [19] reported on a series of seven patients treated with allograft ACL and transtibial PCL reconstruction. Four patients underwent arthroscopic lysis of adhesions and six patients developed heterotopic bone around the knee, a complication that was not seen in our series. Furthermore, in one long-term outcome study, dislocation was associated with a risk of posttraumatic osteoarthritis in half of the study subjects [26].
Current surgical techniques used to reconstruct the PCL can be either cumbersome and add operative time or risk difficulty with graft passage around the killer curve in the transtibial technique. Additionally, the transtibial technique risks potential vascular injury with drilling toward the popliteal artery. We found this modification of the posteromedial approach, which avoids prone positioning, to be useful for KDIIIM injuries. The approach to the PCL tibial attachment also allows adequate exposure to perform an MCL reconstruction. Although no intraoperative neurovascular injuries were encountered in this small patient case series, larger comparative studies are needed to review the safety of this approach compared with standard inlay and transtibial approaches.
Acknowledgments
We thank the University of New Mexico Knee Dislocation research team including Kim Fields, research coordinator, Burke Gurney PT, PhD, James Dexter PT, MA, Toribio (Toby) T. Natividad MD, Benjamin Olson MD, Ron Andrews PT, PhD, and Sandra Schreyer. Drs. Schenck and Wascher would like to give a special thanks to our coauthor and outstanding clinician/resident researcher partner, Dustin Richter MD.
Footnotes
Each author certifies that he, or a member of his immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Berg EE. Posterior cruciate ligament tibial inlay reconstruction. Arthroscopy. 1995;11:69–76. doi: 10.1016/0749-8063(95)90091-8. [DOI] [PubMed] [Google Scholar]
- 2.Bosworth DM. Transplantation of the semitendinosus for repair of laceration of medial collateral ligament of the knee. J Bone Joint Surg Am. 1952;34:196–202. [PubMed] [Google Scholar]
- 3.Cooper DE, Speer KP, Wickiewicz TL, Warren RF. Complete knee dislocation without posterior cruciate ligament disruption: a report of four cases and review of the literature. Clin Orthop Relat Res. 1992;284:228–233. [PubMed] [Google Scholar]
- 4.Cooper DE, Stewart D. Posterior cruciate ligament reconstruction using single-bundle patella tendon graft with tibial inlay fixation: 2- to 10-year follow-up. Am J Sports Med. 2004;32:346–360. doi: 10.1177/0363546503261511. [DOI] [PubMed] [Google Scholar]
- 5.Fanelli GC, Edson CJ. Arthroscopically combined anterior and posterior cruciate ligament reconstruction in the multiple ligament injured knee: 2- to 10-year follow-up. Arthroscopy. 2002;18:703–714. doi: 10.1053/jars.2002.35142. [DOI] [PubMed] [Google Scholar]
- 6.Fanelli GC, Orcutt DR, Harris JD, Zijerdi DA. Posterior cruciate ligament reconstruction. Orthopaedic Knowledge Online Journal. 2007;5.
- 7.Green NE, Allen BL. Vascular injuries associated with dislocation of the knee. J Bone Joint Surg Am. 1977;59:236–239. [PubMed] [Google Scholar]
- 8.Harner CD, Waltrip RL, Bennett CH, Francis KA, Cole B, Irrgang JJ. Surgical management of knee dislocations. J Bone Joint Surg Am. 2004;86:262–273. doi: 10.2106/00004623-200402000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Hoover NW. Injuries of the popliteal artery associated with fractures and dislocations. Surg Clin North Am. 1961;41:1099–1112. doi: 10.1016/s0039-6109(16)36451-9. [DOI] [PubMed] [Google Scholar]
- 10.Hughston JC, Degenhardt TC. Reconstruction of the posterior cruciate ligament. Clin Orthop Relat Res. 1982;164:59–77. [PubMed] [Google Scholar]
- 11.Jakob RP, Ruegsegger M. Therapy of posterior and posterolateral knee instability [in German] Orthopade. 1993;22:405–413. [PubMed] [Google Scholar]
- 12.LaPrade RF, Wijdicks CA. Surgical technique: development of an anatomic medial knee reconstruction. Clin Orthop Relat Res. 2012;470:806–814. doi: 10.1007/s11999-011-2061-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liow RY, McNicholas MJ, Keating JF, Nutton RW. Ligament repair and reconstruction in traumatic dislocation of the knee. J Bone Joint Surg Br. 2003;85:845–851. [PubMed] [Google Scholar]
- 14.Lobenhoffer P, Gerich T, Bertram T, Lattermann C, Pohlemann T, Tscheme H. Particular posteromedial and posterolateral approaches for the treatment of tibial head fractures. Unfallchirurg. 1997;100:957–967. doi: 10.1007/s001130050218. [DOI] [PubMed] [Google Scholar]
- 15.MacGillivray JD, Stein BE, Park M, Allen AA, Wickiewicz TL, Warren RF. Comparison of tibial inlay versus transtibial techniques for isolated posterior cruciate ligament reconstruction: minimum 2-year followup. Arthroscopy. 2006;22:320–328. doi: 10.1016/j.arthro.2005.08.057. [DOI] [PubMed] [Google Scholar]
- 16.Schenck RC. [UNM Orthopaedics]. PCL inlay reconstruction, posteromedial approach with supine positioning. [Video file]. Published on October 2, 2013. Available at: http://youtu.be/_VVo2-lDmLI. Accessed December 13, 2013.
- 17.Schenck RC., Jr The dislocated knee. Instr Course Lect. 1994;43:127–136. [PubMed] [Google Scholar]
- 18.Schulz MS, Steenlage ES, Russe K, Strobel MJ. Distribution of posterior tibial displacement in knees with posterior cruciate ligament tears. J Bone Joint Surg Am. 2007;89:332–338. doi: 10.2106/JBJS.C.00834. [DOI] [PubMed] [Google Scholar]
- 19.Shapiro MS, Freedman EL. Allograft reconstruction of the anterior and posterior cruciate ligaments after traumatic knee dislocation. Am J Sports Med. 1995;23:580–587. doi: 10.1177/036354659502300511. [DOI] [PubMed] [Google Scholar]
- 20.Shelbourne KD, Pritchard J, Rettig AC, McCarroll JR, Vanmeter CD. Knee dislocations with intact PCL. Orthop Rev. 1992;21:607–611. [PubMed] [Google Scholar]
- 21.Spiridonov SI, Slinkard NJ, LaPrade RF. Isolated and combined grade-III posterior cruciate ligament tears treated with double-bundle reconstruction with use of endoscopically placed femoral tunnels and grafts: operative technique and clinical outcomes. J Bone Joint Surg Am. 2011;93:1773–1780. doi: 10.2106/JBJS.J.01638. [DOI] [PubMed] [Google Scholar]
- 22.Stannard JP, Schenck RC, Fanelli GC. Knee dislocations and fracture-dislocations. In: Bucholz RW, Court-Brown CM, Heckman JD, Tornetta P, editors. Rockwood and Green’s Fractures in Adults. 7. Philadelphia, PA: Lippincott Williams & Wilkins; 2010. pp. 1840–1847. [Google Scholar]
- 23.Walker DN, Hardison RR, Schenck RC., Jr A baker’s dozen of knee dislocations. Am J Knee Surg. 1994;7:117–124. [Google Scholar]
- 24.Wascher DC, Becker JR, Dexter JG, Blevins FT. Reconstruction of the anterior and posterior cruciate ligaments after knee dislocation: results using fresh-frozen nonirradiated allografts. Am J Sports Med. 1999;27:189–196. doi: 10.1177/03635465990270021301. [DOI] [PubMed] [Google Scholar]
- 25.Wascher DC, Dvirnak PC, DeCoster TA. Knee dislocation: initial assessment and implications for treatment. J Orthop Trauma. 1997;11:525–559. doi: 10.1097/00005131-199710000-00011. [DOI] [PubMed] [Google Scholar]
- 26.Werier J, Keating JF, Meek RN. Complete dislocation of the knee: the long-term results of ligamentous reconstruction. Knee. 1998;5:255–260. doi: 10.1016/S0968-0160(98)00015-5. [DOI] [Google Scholar]