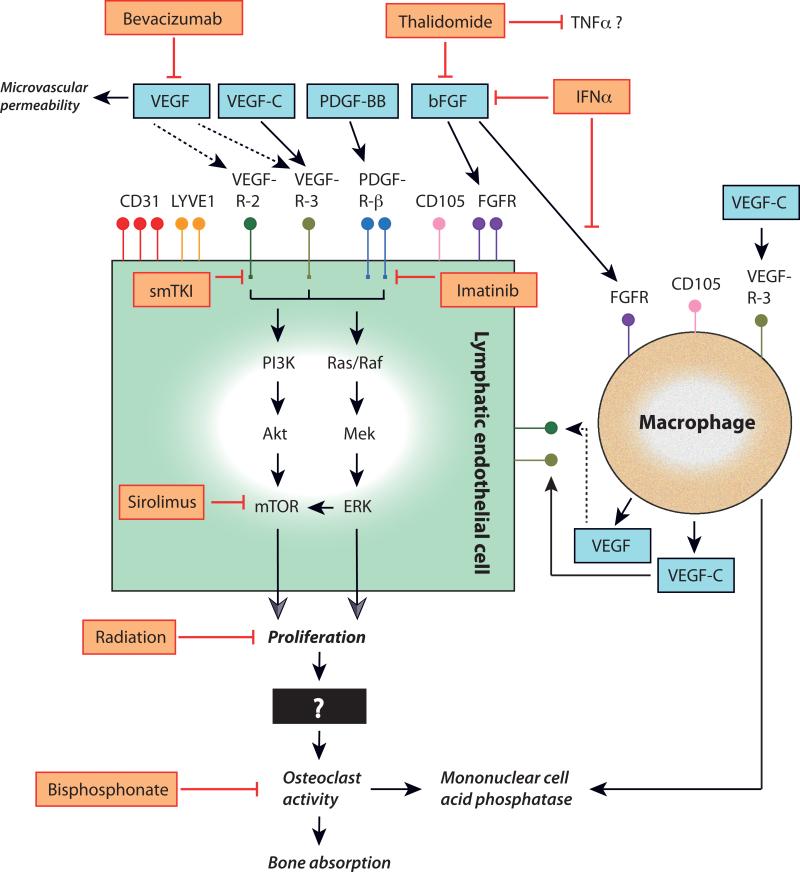
FIGURE 1. Schematic representation of the putative molecular pathways and their clinical inhibitors in Gorham disease.
Lymphatic endothelial cell (LEC) markers shown to be variably expressed in Gorham tissues include cluster of differentiation (CD)-31 protein, lymphatic vessel endothelial hyaluronan receptor (LYVE)-1, and CD105. Growth factors stimulating (black arrows) LEC proliferation and macrophage activation in Gorham disease are shown (blue boxes) and include vascular endothelial growth factor (VEGF; though it may not have a direct effect on LECs in Gorham disease (dashed arrows)), VEGF-C, platelet-derived growth factor (PDGF)-BB, and basic fibroblast growth factor (bFGF). Binding of these ligands to their receptors—VEGF-receptor (R)-2, VEGFR-3, PDGFR-β, and FGFR—will trigger downstream signaling. Clinical inhibitors (orange boxes, red barred lines) of LEC surface receptor proteins and their ligands shown to affect disease progression in Gorham disease include humanized monoclonal antibody bevacizumab, thalidomide and interferon (IFN)-alpha. Imatinib mesylate (imatinib) inhibits signaling through the tyrosine kinase domain of PDGFR-β. Small molecule tyrosine kinase inhibitors (smTKI) that are now in development and in clinical trials may be able to block signaling through the tyrosine kinase domains of activated receptors or their downstream effectors. One promising agent—sirolimus—blocks the mTOR pathway, which is activated through the PI3K/Akt and Ras/Raf signaling pathways. However, there are many other signaling targets that may present potential therapeutic opportunities in Gorham disease. Radiation therapy also halts progression in Gorham disease (in part) by inhibiting LEC proliferation. Bisphosphonates inhibit increased osteoclast activity and the ensuing bone resorption.