Abstract
Today diabetes mellitus has emerged as a major healthcare problem throughout the world. It has recently broken the age barrier and has been diagnosed in younger people also. Sustained hyperglycemia is associated with many complications including male reproductive dysfunctions and infertility. Numerous medicinal plants have been used for the management of the diabetes mellitus in various traditional system of medicine and in folklore worldwide as they are a rich source of bioactive phytoconstituents, which lower blood glucose level and/or also act as antioxidants resulting in the amelioration of oxidative-stress-induced diabetic complications. The present review describes the ameliorative effects of medicinal plants or their products, especially on male reproductive dysfunctions, in experimental diabetic animal models.
Keywords: Antioxidant, blood glucose, sperm function, testosterone, testis
INTRODUCTION
Diabetes mellitus (DM) is a chronic, complicated metabolic disorder characterized by hyperglycemia, which often results from defects in insulin secretion, insulin action, or both. Moreover, DM is associated with severe disturbances of carbohydrate, fat, and protein metabolism.[1]
Diabetes is rapidly emerging as a major public health challenge and demands special attention towards its management. According to the diabetic atlas of the International Diabetic Federation, 366 million people were affected by diabetes worldwide in 2011, and diabetes prevalence is expected to 522 million by 2030.[2] Furthermore, the increasing prevalence of diabetes mellitus in children and adolescents is also of concern. Poorly managed diabetes can lead to a large number of complications including retinopathy, neuropathy, nephropathy, cardiovascular diseases, and male impotency.[3,4]
A large number of studies, both in diabetic men and animal models indicate that DM causes male infertility based on impotency, retrograde ejaculation, and hypogonadism. DM may affect male reproductive functions at multiple levels including variation in sperm quality, altered spermatogenesis, morphological changes in testes, altered glucose metabolism in Sertoli-blood testes barrier, reduced testosterone, ejaculatory dysfunction, and reduced libido.[5,6,7,8,9,10,11,12,13] Several clinical and animal studies have focused on the molecular mechanism responsible for the alterations induced by DM in male reproductive potential including endocrine disorders, neuropathy, and increased oxidative stress.[12]
DM-induced adverse effects on male reproductive functions might be mediated through hormonal alterations in the hypothalamic-pituitary-gonadal axis or through the direct interactions of insulin with the testes and sperm cells, as both the testes and sperms themselves produce insulin.[11] Insulin expression in the testes also seems to be affected by diabetes.[14] Both diabetic men and knockout mice had notably impaired spermatogenesis, increased germ cell depletion, and Sertoli cell vacuolization, suggesting that insulin may have an important role in spermatogenesis.[6,15] It is still unclear whether the effects of diabetes on male fertility are mediated through testicular insulin insufficiency or through systemic effects of diabetes.[16,17,18]
Furthermore, oxidative stress may play a pathogenic role in diabetes-related male reproductive function abnormalities.[12] Studies have shown that men suffering from diabetes have sperms with greater DNA fragmentation and an increase in advanced glycation end products and their receptors (RAGE) leading to deterioration of sperm quality, sperm functions coupled with changes in testicular metabolite levels and spermatogenic gene expression.[19,20,21] Several studies have shown that antioxidant treatment improves glycemic index, reduces diabetic complications, and protects components from oxidative damage.[22,23]
The use of plants in the management of diabetes is well documented, which is primarily due to anti-hyperglycemic and/or oxygen radical scavenging of their various phytoconstituents through various mechanisms.[24,25] Medicinal plants provide better alternatives as they are less toxic, easily available and affordable.[26]
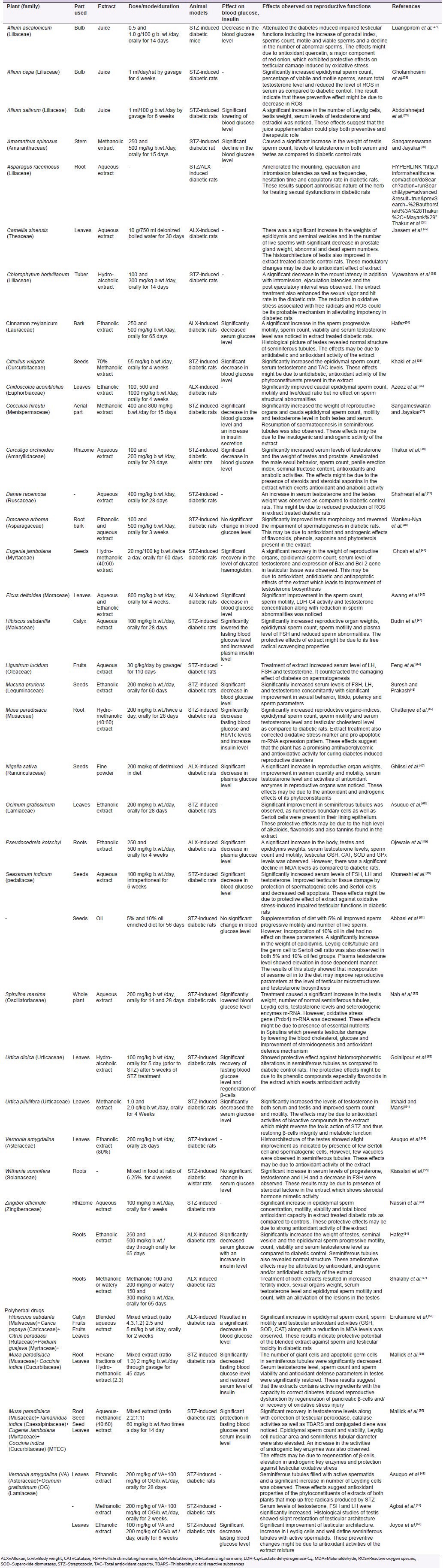
A brief review of the medicinal plants having ameliorative effects on blood sugar levels and/or male reproductive functions in experimental diabetic animals is presented in Table 1.
Table 1.
Review of the literature of various plants/herbs showing modulatory effect on reproductive dysfunctions in male diabetic animals
CONCLUSION
From the results of the above studies, it can be concluded that supplementation of medicinal plant products, extracts, or herbal formulations may be useful in alleviation of DM-induced complications, especially male reproductive dysfunction, by virtue of their antidiabetic, antioxidant, and androgenic activities of various bioactive phytoconstituents.
ACKNOWLEDGMENTS
The authors are thankful to Professor N. P. Singh, Head of the Department and Center for Advanced Studies Phase II, Department of Zoology, University of Rajasthan, Jaipur for providing necessary facilities.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2011;34(Suppl 1):62–9. doi: 10.2337/dc11-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: Global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94:311–21. doi: 10.1016/j.diabres.2011.10.029. [DOI] [PubMed] [Google Scholar]
- 3.Melendez-Ramirez LY, Richards RJ, Cefalu WT. Complications of type 1 diabetes. Endocrinol Metab Clin North Am. 2010;39:625–40. doi: 10.1016/j.ecl.2010.05.009. [DOI] [PubMed] [Google Scholar]
- 4.Atkinson MA, Maclaren NK. The pathogenesis of insulin-dependent diabetes mellitus. N Engl J Med. 1994;331:1428–36. doi: 10.1056/NEJM199411243312107. [DOI] [PubMed] [Google Scholar]
- 5.Sexton WJ, Jarow JP. Effect of diabetes mellitus upon male reproductive function. Urology. 1997;49:508–13. doi: 10.1016/s0090-4295(96)00573-0. [DOI] [PubMed] [Google Scholar]
- 6.Baccetti B, La Marca A, Piomboni P, Capitani S, Bruni E, Petraglia F, et al. Insulin-dependent diabetes in men is associated with hypothalamo-pituitary derangement and with impairment in semen quality. Hum Reprod. 2002;17:2673–7. doi: 10.1093/humrep/17.10.2673. [DOI] [PubMed] [Google Scholar]
- 7.Scarano WR, Messias AG, Oliva SU, Klinefelter GR, Kempinas WG. Sexual behaviour, sperm quantity and quality after short-term streptozotocin-induced hyperglycaemia in rats. Int J Androl. 2006;29:482–8. doi: 10.1111/j.1365-2605.2006.00682.x. [DOI] [PubMed] [Google Scholar]
- 8.Agbaje IM, Rogers DA, McVicar CM, McClure N, Atkinson AB, Mallidis C, et al. Insulin dependent diabetes mellitus: Mplications for male reproductive function. Hum Reprod. 2007;22:1871–7. doi: 10.1093/humrep/dem077. [DOI] [PubMed] [Google Scholar]
- 9.Ricci G, Catizone A, Esposito R, Pisanti FA, Vietri MT, Galdieri M. Diabetic rat testes: Morphological and functional alterations. Andrologia. 2009;41:361–8. doi: 10.1111/j.1439-0272.2009.00937.x. [DOI] [PubMed] [Google Scholar]
- 10.Mallidis C, Agbaje I, McClure N, Kliesch S. The influence of diabetes mellitus on male reproductive function: A poorly investigated aspect of male infertility. Urologe A. 2011;50:33–7. doi: 10.1007/s00120-010-2440-3. [DOI] [PubMed] [Google Scholar]
- 11.Schoeller EL, Schon S, Moley KH. The effects of type 1 diabetes on the hypothalamic, pituitary and testes axis. Cell Tissue Res. 2012;349:839–47. doi: 10.1007/s00441-012-1387-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.La Vignera S, Condorelli R, Vicari E, D’Agata R, Calogero AE. Diabetes mellitus and sperm parameters. J Androl. 2012;33:145–53. doi: 10.2164/jandrol.111.013193. [DOI] [PubMed] [Google Scholar]
- 13.Alves MG, Martins AD, Cavaco JE, Socorro S, Oliveira PF. Diabetes, insulin-mediated glucose metabolism and Sertoli/blood-testis barrier function. Tissue Barriers. 2013;1:e23992. doi: 10.4161/tisb.23992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gomez O, Ballester B, Romero A, Arnal E, Almansa I, Miranda M, et al. Expression and regulation of insulin and the glucose transporter GLUT8 in the testes of diabetic rats. Horm Metab Res. 2009;41:343–9. doi: 10.1055/s-0028-1128146. [DOI] [PubMed] [Google Scholar]
- 15.Brüning JC, Gautam D, Burks DJ, Gillette J, Schubert M, Orban PC, et al. Role of brain insulin receptor in control of body weight and reproduction. Science. 2000;289:2122–5. doi: 10.1126/science.289.5487.2122. [DOI] [PubMed] [Google Scholar]
- 16.Guneli E, Tugyan K, Ozturk H, Gumustekin M, Cilaker S, Uysal N. Effect of melatonin on testicular damage in streptozotocin-induced diabetes rats. Eur Surg Res. 2008;40:354–60. doi: 10.1159/000118032. [DOI] [PubMed] [Google Scholar]
- 17.Rabbani SI, Devi K, Khanam S. Inhibitory effect of glimepiride on nicotinamide-streptozotocin induced nuclear damages and sperm abnormality in diabetic Wistar rats. Indian J Exp Biol. 2009;47:804–10. [PubMed] [Google Scholar]
- 18.Fernandes GS, Fernandez CD, Campos KE, Damasceno DC, Anselmo-Franci JA, Kempinas WD. Vitamin C partially attenuates male reproductive deficits in hyperglycemic rats. [Last accessed on 2011 Oct 03];Reprod Biol Endocrinol. 2011 9:100. doi: 10.1186/1477-7827-9-100. Available from: http://www.rbej.com/content/9/1/100 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Amaral S, Oliveira PJ, Ramalho-Santos J. Diabetes and impairment of reproductive function: Possible role of mitochondria and reactive oxygen species. Curr Diabetes Rev. 2008;4:46–54. doi: 10.2174/157339908783502398. [DOI] [PubMed] [Google Scholar]
- 20.Mallidis C, Agbaje IM, Rogers DA, Glenn JV, Pringle R, Atkinson AB, et al. Advanced glycation end products accumulate in the reproductive tract of men with diabetes. Int J Androl. 2009;32:295–305. doi: 10.1111/j.1365-2605.2007.00849.x. [DOI] [PubMed] [Google Scholar]
- 21.Karimi J, Goodarzi MT, Tavilani H, Khodadadi I, Amiri I. Relationship between advanced glycation end products and increased lipid peroxidation in semen of diabetic men. Diabetes Res Clin Pract. 2011;91:61–6. doi: 10.1016/j.diabres.2010.09.024. [DOI] [PubMed] [Google Scholar]
- 22.Rahimi R, Nikfar S, Larijani B, Abdollahi M. A review on the role of antioxidants in the management of diabetes and its complications. Biomed Pharmacother. 2005;59:365–73. doi: 10.1016/j.biopha.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 23.Mohasseb M, Ebied S, Yehia MA, Hussein N. Testicular oxidative damage and role of combined antioxidant supplementation in experimental diabetic rats. J Physiol Biochem. 2011;67:185–94. doi: 10.1007/s13105-010-0062-2. [DOI] [PubMed] [Google Scholar]
- 24.Grover JK, Yadav S, Vats V. Medicinal plants of India with anti-diabetic potential. J Ethnopharmacol. 2002;81:81–100. doi: 10.1016/s0378-8741(02)00059-4. [DOI] [PubMed] [Google Scholar]
- 25.Chan CH, Ngoh GC, Yusoff R. A brief review on anti diabetic plants: Global distribution, active ingredients, extraction techniques and acting mechanisms. Pharmacogn Rev. 2012;6:22–8. doi: 10.4103/0973-7847.95854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Khan V, Najmi AK, Akhtar M, Aqil M, Mujeeb M, Pillai KK. A pharmacological appraisal of medicinal plants with antidiabetic potential. J Pharm Bioallied Sci. 2012;4:27–42. doi: 10.4103/0975-7406.92727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Luangpirom A, Kourchampa W, Junaimuang T, Somsapt P, Sritragool O. Effect of shallot (Allium ascalonicum L.) bulb juice on hypoglycemia and sperm quality in streptozotocin induced diabetic mice. ABAH Bioflux. 2013;5:49–54. [Google Scholar]
- 28.Gholamhosini B, Khaki A, Ahmadi-Ashtiani HR, Rezazadeh S, Rastegar H, Fathiazad F, et al. Treatment effects of onion on spermatogenesis in streptozotocin-induced diabetic rat. J Med Plants. 2009;8:153–61. [Google Scholar]
- 29.Abdolahnejad A, Gol A, Dabiri S. Garlic effects on reproductive complications of diabetes mellitus in male rats. Physiol Pharmacol. 2009;13:297–307. [Google Scholar]
- 30.Sangameswaran B, Jayakar B. Anti-diabetic, anti-hyperlipidemic and spermatogenic effects of Amaranthus spinosus Linn. on streptozotocin-induced diabetic rats. J Nat Med. 2008;62:79–82. doi: 10.1007/s11418-007-0189-9. [DOI] [PubMed] [Google Scholar]
- 31.Thakur M, Bhargava S, Dixit VK. Effect of Asparagus racemosus on sexual dysfunction in hyperglycemic male rats. Pharmaceut Biol. 2009;47:390–5. [Google Scholar]
- 32.Jassem HM, Ismaiel HK, Jasem AY. Effect of aqueous extract of green tea on sexual efficiency in adult male rats treated with alloxan. Iraq J Vet Sci. 2008;22:75–82. [Google Scholar]
- 33.Vyawahare NS, Kagathara VG, Kshirsagar AD, Rajendran R, Patil MN, Jagtap AA, et al. Effect of hydroalcoholic extract of Chlorophytum borivilianum tubers in alleviating the diabetic impotency in streptozotocin induced male diabetic rats. Phcog Res. 2009;1:314–9. [Google Scholar]
- 34.Hafez DA. Effect of extracts of ginger roots and Cinnamon bark on fertility of male diabetic rats. J Am Sc. 2010;6:940–7. [Google Scholar]
- 35.Khaki A, Ouladsahebmadarek E, Zahedi A, Ahmadnezhad B. Effect of water melon seeds extracts (citrullus vulgaris) on sperms in diabetic rat. Indones J Pharm. 2013;24:122–6. [Google Scholar]
- 36.Azeez OI, Oyagbemi AA, Oyeyemi MO, Odetola AA. Ameliorative effects of Cnidoscolus aconitifolius on alloxan toxicity in Wistar rats. Afr Health Sci. 2010;10:283–91. [PMC free article] [PubMed] [Google Scholar]
- 37.Sangameswaran B, Jayakar B. Anti-diabetic and spermatogenic activity of Cocculus hirsutus (L) Diels. Afr J Biotechnol. 2007;6:1212–6. [Google Scholar]
- 38.Thakur M, Chauhan NS, Sharma V, Dixit VK, Bhargava S. Effect of Curculigo orchiodes on hyperglycemia-induced oligospermia and sexul dysfunction in male rats. Int J Impot Res. 2012;24:31–7. doi: 10.1038/ijir.2011.43. [DOI] [PubMed] [Google Scholar]
- 39.Shahreari S, Khaki A, Ahmadi-Ashtiani HR, Rezazadeh S, Hajiaghaei R. Effects of Danae racemosa on testosterone hormone in experimental diabetic rats. J Med Plants. 2010;9:114–9. [Google Scholar]
- 40.Wankeu-Nya M, Florea A, Bâlici S, Watcho P, Matei H, Kamanyi A. Dracaena arborea alleviates ultra-structural spermatogenic alterations in streptozotocin-induced diabetic rats. [Last accessed on 2013 Apr 16];BMC Complement Altern Med. 2013 l13:71. doi: 10.1186/1472-6882-13-71. Available from: http://www.biomedcentral.com/1472-6882/13/71 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ghosh A, Jana K, Ali KM, De D, Chatterjee K, Ghosh D. Corrective role of Eugenia jambolana on testicular impairment in streptozotocin-induced diabetic male albino rat: An approach through genomic and proteomic study. Andrologia. 2013. [Last accessed on 2013 May 09]. Available from: http://onlinelibrary.wiley.com/doi/10.1111/and 12081/pdf . [DOI] [PubMed]
- 42.Awang Z, Najib ML, Idzham M, Zarin A. Penang, Malaysia: Proceeding of the 2011 IEEE Colloquium on Humanities, Science and Engineering; 2011 Dec 5-6; 2011. Effect of Ficus deltoidea leaves extracts on sperm quality, LDH-C4 activity and testosterone level in alloxan-induced male diabetic rats. CHUSER 2011; pp. 888–91. [Google Scholar]
- 43.Budin SB, Idris MH, Mohamed J, Osman M. Protective role of Hibiscus sabdariffa calyx extract against streptozotocin induced sperm damage in diabetic rats. Excli J. 2012;11:659–69. [PMC free article] [PubMed] [Google Scholar]
- 44.Feng SL, Li SH, Wang Y, Chen CC, Gao B. Effect of ligustrum fruit extract on reproduction in experimental diabetic rats. Asian J Androl. 2001;3:71–3. [PubMed] [Google Scholar]
- 45.Suresh S, Prakash S. Effect of Mucuna pruriens (Linn.) on sexual behavior and sperm parameters in streptozotocin-induced diabetic male rat. J Sex Med. 2012;9:3066–78. doi: 10.1111/j.1743-6109.2010.01831.x. [DOI] [PubMed] [Google Scholar]
- 46.Chatterjee K, Ali KM, De D, Bera TK, Jana K, Maiti S. Diabetes induced testicular dysfunction amelioration by ethyl acetate fraction of hydromethanolic extract of root of Musa paradisiaca L. in streptozotocin-induced diabetic rat. Asian Pac J Trop Dis. 2012;(Suppl 1):233–41. [Google Scholar]
- 47.Ghlissi Z, Hamden K, Saoudi M, Sahnoun Z, Mounir Zeghal K, El Fki A, et al. Effects of Nagella sativa seeds on reproductive system of male diabetic rats. Afr J Pharm Pharacol. 2012;6:1444–50. [Google Scholar]
- 48.Asuquo O, Edet A, Mesembe O, Atanghwo J. Ethanolic extracts of Vernonia amygdalina and Ocimum gratissimum enhance testicular improvement in diabetic Wistar rats. [Last accessed on 2011 Mar 11];Internet J Alternative Med. 2010 8:2. Available from: http://archive.ispub.com/journal/ the-internet- journal-of-alternative-medicine/volume-8-number-2/ethanolic- extracts-of-vernonia-amygdalina-and-ocimum-gratissimum- enhance-testicular-improvement-in-diabetic-wistar-rats.html . [Google Scholar]
- 49.Ojewale AO, Olaniyan OT, Faduyile FA, Odukanmi OA, Oguntola JA, Dare BJ. Testiculo protective effects of ethanolic roots extract of Pseudocedrela kotschyi on alloxan induced testicular damage in diabetic rats. Br J Med Med Res. 2014;4:548–63. [Google Scholar]
- 50.Khaneshi F, Nasrolahi O, Azizi S, Nejati V. Sesame effects on testicular damage in streptozotocin-induced diabetes rats. Avicenna J Phytomed. 2013;3:347–55. [PMC free article] [PubMed] [Google Scholar]
- 51.Abbasi Z, Tabatabaei SR, Mazaheri Y, Barati F, Morovvati H. Effects of sesame oil on the reproductive parameters of diabetes mellitus-induced male rats. World J Mens Health. 2013;31:141–9. doi: 10.5534/wjmh.2013.31.2.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nah WH, Koh IK, Ahn HS, Kim MJ, Kang HG, Jun JH, et al. Effect of Spirulina maxima on spermatogenesis and steroidogenesis in streptozotocin-induced type I diabetic male rats. Food Chem. 2012;134:173–9. [Google Scholar]
- 53.Ghafari S, Balajadeh BK, Golalipour MJ. Effect of Urtica dioica L. on testicular tissue in STZ-induced diabetic rats. Pak J Biol Sci. 2011;14:798–804. doi: 10.3923/pjbs.2011.798.804. [DOI] [PubMed] [Google Scholar]
- 54.Irshaid F, Mansi K. Effects of leaf extract of Urtica pilulifera L. on male reproductive system of streptozotocin-diabetic rats. Am J Pharmacol Toxicol. 2009;4:22–8. [Google Scholar]
- 55.Kiasalari Z, Khalili M, Aghaei M. Effect of Withania somnifera on levels of sex hormones in the diabetic male rats. Iran J Reprod Med. 2009;7:163–8. [Google Scholar]
- 56.Nassiri M, Khaki A, Ahmadi-Ashtiani HR, Rezazadeh S, Rastgar H, Gharachurlu S. Effects of ginger on spermatogenesis in streptozotocin-induced diabetic rat. J Med Plants. 2009;8:118–24. [Google Scholar]
- 57.Shalaby MA, Hamowieh AR. Safety and efficacy of Zingiber officinale roots on fertility of male diabetic rats. Food Chem Toxicol. 2010;48:2920–4. doi: 10.1016/j.fct.2010.07.028. [DOI] [PubMed] [Google Scholar]
- 58.Erukainure OL, Okafor OY, Obode OC, Ajayi A, Oluwole OB, Oke OV, et al. Blend of roselle calyx and selected fruit modulates testicular redox status and sperm quality of diabetic rats. J Diabetes Metab. 2012;3:1–5. [Google Scholar]
- 59.Mallick C, Bera TK, Ali KM, Chatterjee K, Ghosh D. Diabetes-induced testicular disorders Vis-à-vis Germ cell apoptosis in albino rat: Ramedial effect of haxane fraction of root of Musa paradisiaca and leaf of Coccinia indica. J Health Sci. 2010;56:641–54. [Google Scholar]
- 60.Mallick C, Mandal S, Barik B, Bhattacharya A, Ghosh D. Protection of testicular dysfunctions by MTEC, a formulated herbal drug, in streptozotocin induced diabetic rat. Biol Pharm Bull. 2007;30:84–90. doi: 10.1248/bpb.30.84. [DOI] [PubMed] [Google Scholar]
- 61.Agbai E, Durudola SD, Igbinosun, Mounmbegna PP. Synergistic effect of methanolic extract of Vernonia amygdalina and Ocimum gratissimum on male reproductive hormones in streptozotocin-induced diabetic wistar rats. Int J Biol Sci. 2011;3:105–15. [Google Scholar]
- 62.Joyce OO, Chinwe ND, Nnabufe EJ, Tabot PD, Kwaku JP. Comparative anti-diabetic effects of Ocimium gratissimum, Vernonia amygdalina and insulin on testicular architecture in STZ-induced diabetic rats. Am J Pharm Tech Res. 2012;2:279–87. [Google Scholar]


