Figure 1.
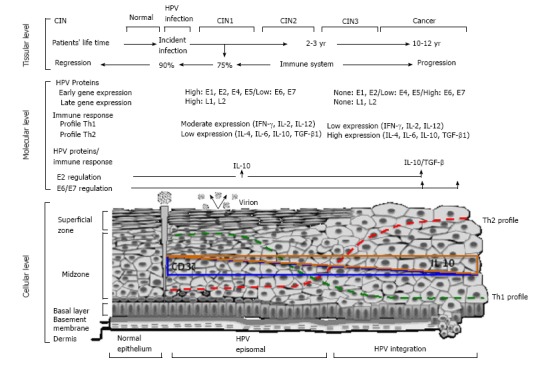
Systematic representation for cervical human Papillomavirus-carcinogenesis: Role of immune response. The main event is the human Papillomavirus (HPV) infection of epithelial cells in the basal membrane. HPV can turn into episomal bodies, which will be in charge of, on one part, producing infective virions and, on the other, integrating into the genome of epithelial cells. Upon infection, an average of 2-3 yr are necessary to develop of CIN 1/2 and/or high-grade (CIN3), often characterized by the integration of the viral genome, one key event for disease progression as this frequently triggers the deregulation of the E6 and E7 oncogenes, major chromosomal alterations and cellular immortalization[10]. The immune system plays a key role during HPV-carcinogenesis since the majority of high-risk HPV infections (90%), as well as most of low-grade lesions (75%) regress[5,6]. Due to this, and the long periods of time between viral infection and the progression to invasive disease, the fail of immune response is necessary to cancer development. Since the beginning of HPV infection, there are augment in the immunosuppressive cytokine IL-10 at the cervical level, and this increased according with the grade of lesion, being the highest concentration at cancer stage[25]. A shift to Th2-type cytokines in the course of development of cervical cancer is reflected with an increased serum concentration of Th2-type cytokines[22,23]. Inversely, the presence of CD3zeta chain in the tumor infiltrating T-lymphocytes, decreases as the grade of lesion progress, this is due to a reduction of Th1-type cytokines at the late stages of the disease[24]. These are key elements for the impairment of immune responses that allows HPV-persistence, viral integration into the genome epithelial cells, and cellular transformation and immortalization.
