Abstract
Objective:
PMBCL is a distinct type of nonhodgkins lymphoma with specific clinicopathological features. To clarify clinical features, treatment alternatives and outcomes, we evaluated 28 Arab patients treated with chemotherapy or radiotherapy between 2006 and 2011.
Patients and Methods:
PMBCL lymphoma patients identified according to WHO classification and treated at KCCC between 2006 and 2011 were included in this study. Demographic and clinical data are presented as means or medians. Overall survival was estimated using the Kaplan-Meier method. Survival rates were compared using the log-rank test. A P < 0.05 was considered significant.
Results:
The median age of the patients was 31 years and the male to female ratio was 2:1. Majority of the patients (75%) presented with stage I/II disease. Most had features of local extension like pleural effusion (18%) and SVCO (39%). Only 11% of the patients had bone marrow involvement at presentation. 96% of the patients required biopsy from the mediastinal mass either by image guided core biopsy (75%) or by surgical biopsy. Most patients were treated by RCHOP and involved field radiotherapy. Patients with positive PET scan after RCHOP chemotherapy received salvage chemotherapy and BEAM autologous marrow transplant. The five year OS for the entire group was 85% while the PFS was 73%. Patients who had PET scan for response evaluation had better OS [P = 0.013] and PFS [P = 0.039] when compared with those patients who received only radiotherapy based on CT scan evaluation.
Conclusion:
PMBCL is a specific lymphoma entity seen in the young with good survival. The role of PET scan for response evaluation and the type of consolidation therapy needs to be further clarified
Keywords: Mediastinal tumors, Non hodgkins lymphoma, positron emission tomography scan
INTRODUCTION
Primary mediastinal large B-cell lymphoma (PMBCL) is a distinct subtype of lymphoma according to the WHO classification.[1] The disease is more common in females and is overrepresented in the young.[2] It usually presents as bulky tumor in the anterior mediastinum giving rise to local compressive effects.[3] Pleural and pericardial effusions are common. Extra thoracic involvement including bone marrow involvement at the time of initial diagnosis is rare.
International Prognostic Index (IPI) scoring is not very useful in determining prognosis for these patients due to their young age and early stage of presentation. Various prognostic factors like elevated lactate dehydrogenase (LDH), age, performance status, male sex and stage have however been described in different studies.[4,5] R-CHOP (rituximab-CHOP) followed by involved field radiotherapy has been the standard treatment in most series. High dose chemotherapy (HDCT) and autologous bone marrow transplant in first remission as consolidation has been tried in view of the young age of patients. For patients with residual mediastinal disease at the end of treatment, positron emission tomography (PET) scan has become the investigation of choice, with majority of relapses occurring in those with positive PET scan.[6,7]
PATIENTS AND METHODS
PMBCL is a distinct WHO subtype with unique clinico-pathological features. We evaluated clinical characteristics, prognostic factors and survival in 28 consecutive Arab patients treated with R-CHOP between 2006 and 2011. Diagnostic workup included patient history, performance status according to Eastern Cooperative Oncology Group scale, physical examination, complete blood counts, blood biochemistries, CT scan of chest, abdomen and pelvis and bone marrow studies. Diagnosis was established by either image-guided core biopsy or by mediastinoscopy and biopsy. Immunohistochemistry was available for all patients. PET scan was done at the baseline and the end of treatment for all patients from 2009 onwards.
We defined low hemoglobin as less than 120 g/l, low albumin as less than 35 g/l and high LDH as more than 245 U/l. Complete response (CR) was defined as disappearance of all clinical evidence of disease with all lesions becoming FDG (fludeoxyglucose) non-avid on PET scan. If patient satisfies criteria for partial response (PR) by CT scan, but remains PET positive, it was taken as PR and patients advised re-biopsy whenever feasible. Overall survival (OS) was measured from the date of diagnosis until death or date of final follow up for survivors. Event-free survival (EFS) was calculated from date of diagnosis to relapse or death. Primary end points for analysis were OS and EFS. Survival curves were analyzed by Kaplan Meir and log rank tests. Prognostic value of different variables for OS and EFS was determined by multivariate analysis using the Cox regression model.
RESULTS
There were 19 males and 9 females in the study. A majority of the patients presented with chest pain, cough or dyspnea. Eight patients (28%) had B symptoms at presentation, while only 10% of the patients had bone marrow involvement. The patient characteristics are detailed in Table 1 and Figure 1. 25% of the patients required mediastinoscopy and biopsy for diagnosis.
Table 1.
Baseline characteristics of the 28 patients with PMBCL

Figure 1.
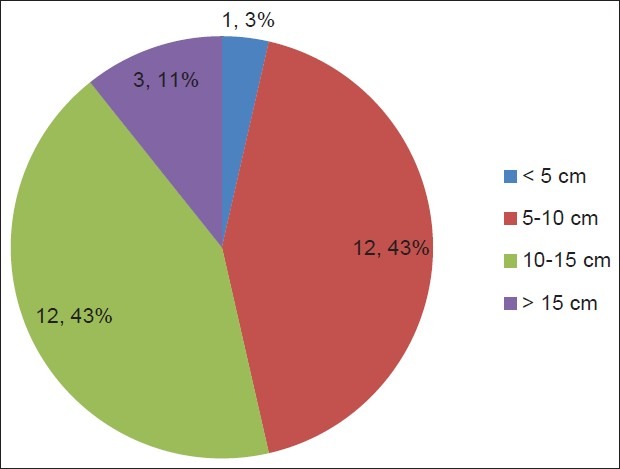
Size of mediastinal mass at presentation
All patients were treated with R-CHOP chemotherapy. Prior to the use of PET scan for response evaluation, all patients with CR or PR by CT scan were treated with involved field radiotherapy. After the advent of PET scan, radiotherapy was used to treat patients who had achieved CR. There were four patients who remained PET positive after six cycles of chemotherapy and they were offered salvage chemotherapy with ESHAP regimen followed by BEAM auto transplant. Two of these patients had a positive cytology after R-CHOP chemotherapy.
Three of the total 28 patients (10.7%) died in a median follow up of 40 months. The mean survival period was 69 months for the entire group with a 5-year overall survival of 85% [Figure 2]. We could not identify any prognostic factors for survival like sex, ECOG status or biochemical parameters. Bone marrow involvement at presentation was the only factor identified to predict response with a P value of 0.045. The 5 year EFS was 73% for the entire group [Figure 3].
Figure 2.
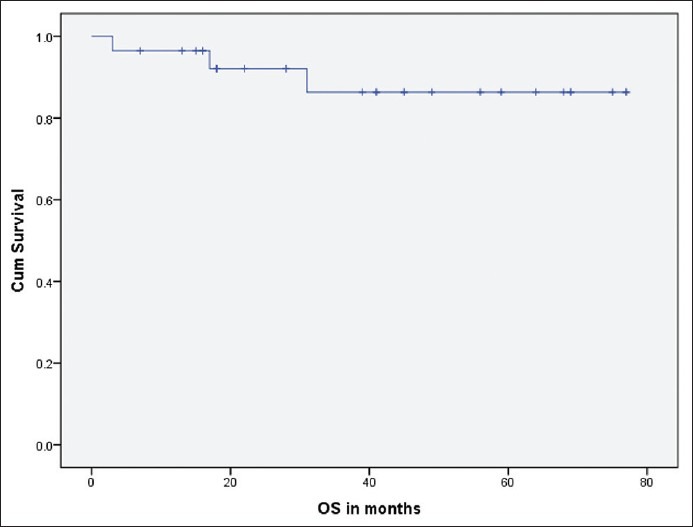
Overall survival (OS) for the entire group
Figure 3.
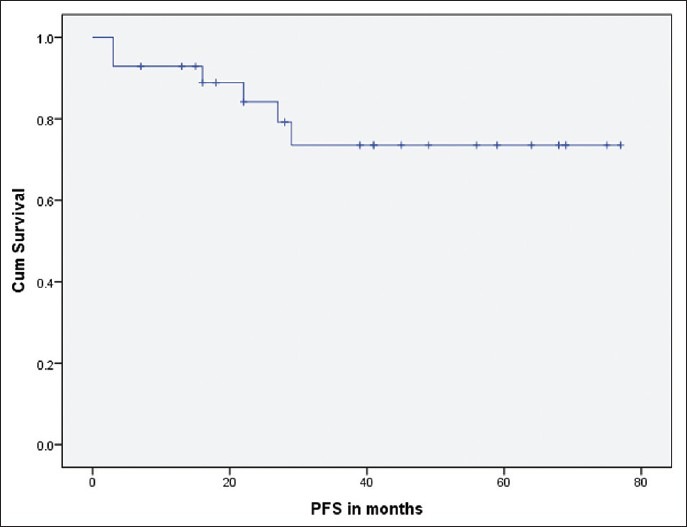
PFS for the entire group
Role of PET scan in determining therapy post R-CHOP chemotherapy
PET scan was done in 20 patients, both for initial staging and for disease re-evaluation. Four patients were deemed to be in PR by PET scan and received salvage chemotherapy followed by autologous stem cell transplant. Sixteen patients were considered as CR by PET scan and received consolidation radiotherapy. One patient in each group relapsed but is still alive at the end of follow up. There were eight patients who did not have PET scan for evaluation and received consolidation radiotherapy. Four of these eight patients relapsed including three who died of progressive lymphoma [Figure 4]. The log rank test for PFS (P = 0.039) and OS (P = 0.013) were significant when compared among patients who had PET scan to those without PET scan for response evaluation.
Figure 4.
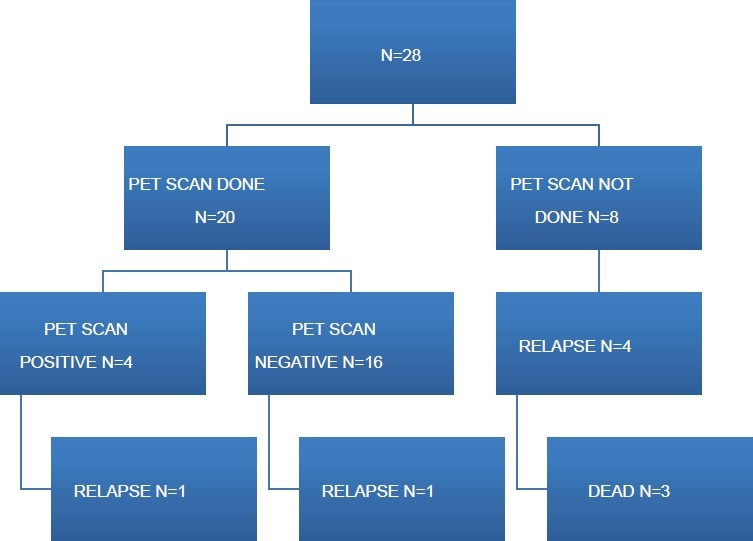
Response evaluation and survival
DISCUSSION
Primary mediastinal large B-cell lymphoma is a distinct clinico-pathological entity under the WHO classification of lymphoid malignancies. It usually occurs in young women and usually presents as bulky mediastinal mass.[8] Tumor extension is local leading to effusions and superior vena cava syndrome (SVCO). Extra-thoracic involvement including bone marrow involvement at presentation is unusual. The median age of our patients was 31 years [range 16-58 years]. 75% of the patients presented with stage I/II disease. Bone marrow involvement was unusual and seen in only 10% of the patients, while 40% had features of SVCO.
PMBCL arises from thymic B cells and can be differentiated from other diffuse large B-cell lymphomas by gene profiling.[9] An important differential diagnosis would be nodular sclerosis classical Hodgkin's lymphoma as it also occurs in young patients and usually presents as bulky mediastinal disease.[10] Most of our patients needed a biopsy from the mediastinum either by CT-guided core biopsy or by mediastinoscopy. Patients presenting with SVCO, thrombosis or effusions needed stabilization before undergoing these diagnostic tests.
IPI risk scoring is of limited value as a majority of patients tend to have low scores due to young age and low stage.[11] We could not identify any negative predictors for survival like sex, ECOG status or biochemical parameters. Bone marrow involvement at presentation was able to identify patients for relapse (P = 0.045) on multivariate analysis.
The optimal therapy for PMBCL is still not defined. Multiagent chemotherapy with R-CHOP followed by involved field radiotherapy is usually the treatment of choice.[12,13,14] HDCT and autologous bone marrow transplantation as consolidation has been tried in first remission in view of young age of patients and relative absence of marrow involvement. A residual mediastinal mass is often found at the end of therapy owing to the predominant fibrotic component. FDG-PET is usually used to assess these lesions and a negative PET scan has more clinical significance. In many series, use of radiotherapy as consolidation was guided by the results of imaging. Patients with partial response as defined by PET has been shown to be salvaged by HDCT.[15] Our study includes four patients who had salvage chemotherapy followed by autologous marrow transplant in view of positive PET scan at the end of treatment. Only one patient in this group later progressed. Various questions still need to be answered in the management of PMBCL like the role of PET scan and consolidation therapy. Being a rare disease, it is essential that multinational trials are designed to answer these questions.
CONCLUSION
PMBCL is a discrete clinico-pathological entity clearly distinct from other B-cell lymphomas on gene profiling. The usual treatment of choice is R-CHOP chemotherapy. The role of PET scan needs prospective evaluation as it may offer valuable prognostic information. It is imperative to cure at the first instance as salvage therapy for progression or relapsed disease is disappointing.[5]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Chan JK. The new World Health Organization classification of lymphomas: The past, the present and the future. Hematol Oncol. 2001;19:129–50. doi: 10.1002/hon.660. [DOI] [PubMed] [Google Scholar]
- 2.A clinical evaluation of the International Lymphoma Study Group classification of non-Hodgkin's lymphoma. The Non-Hodgkin's lymphoma classification project. Blood. 1997;89:3909–18. [PubMed] [Google Scholar]
- 3.Van Besien K, Kelta M, Bahaguna P. Primary mediastinal B-cell lymphoma: A review of pathology and management. J Clin Oncol. 2001;19:1855–64. doi: 10.1200/JCO.2001.19.6.1855. [DOI] [PubMed] [Google Scholar]
- 4.Savage KJ, Al-Rajhi N, Voss N, Paltiel C, Klasa R, Gascoyne RD, et al. Favourable outcome of primary mediastinal large B-cell lymphoma in a single institution: The British Columbia experience. Ann Oncol. 2006;17:123–30. doi: 10.1093/annonc/mdj030. [DOI] [PubMed] [Google Scholar]
- 5.Todeschini G, Secchi S, Morra E, Vitolo U, Orlandi E, Pasini F, et al. Primary mediastinal large B-cell lymphoma (PMBCL): Long-term results from a retrospective multicentre Italian experience in 138 patients treated with CHOP or MACOP-B/VACOP-B. Br J Cancer. 2004;90:372–6. doi: 10.1038/sj.bjc.6601460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jerusalem G, Beguin Y, Fassotte MF, Najjar F, Paulus P, Rigo P, et al. Whole-body positron emission tomography using 18F-fluorodeoxyglucose for posttreatment evaluation in Hodgkin's disease and non-Hodgkin's lymphoma has higher diagnostic and prognostic value than classical computed tomography scan imaging. Blood. 1999;94:429–33. [PubMed] [Google Scholar]
- 7.Zinzani PL, Fanti S, Battista G, Tani M, Castellucci P, Stefoni V, et al. Predictive role of positron emission tomography (PET) in the outcome of lymphoma patients. Br J Cancer. 2004;91:850–4. doi: 10.1038/sj.bjc.6602040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cazals-Hatem D, Lepage E, Brice P, Ferrant A, d’Agay MF, Baumelou E, et al. Primary mediastinal large B-cell lymphoma. A clinicopathologic study of 141 cases compared with 916 nonmediastinal large B-cell lymphomas, a GELA (“Groupe d’Etude des Lymphomes de l’Adulte”) study. Am J Surg Pathol. 1996;20:877–88. doi: 10.1097/00000478-199607000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Savage KJ, Monti S, Kutok JL, Cattoretti G, Neuberg D, De Leval L, et al. The molecular signature of mediastinal large B-cell lymphoma differs from that of other diffuse large B-cell lymphomas and shares features with classical Hodgkin lymphoma. Blood. 2003;102:3871–9. doi: 10.1182/blood-2003-06-1841. [DOI] [PubMed] [Google Scholar]
- 10.Dunleavy K, Grant C, Eberle FC, Pittaluga S, Jaffe ES, Wilson WH. Gray zone lymphoma: Better treated like hodgkin lymphoma or mediastinal large B-cell lymphoma? Curr Hematol Malig Rep. 2012;7:241–7. doi: 10.1007/s11899-012-0130-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abou-Elella AA, Weisenburger DD, Vose JM, Kollath JP, Lynch JC, Bast MA, et al. Primary mediastinal large B-cell lymphoma: A clinicopathologic study of 43 patients from the Nebraska Lymphoma Study Group. J Clin Oncol. 1999;17:784–90. doi: 10.1200/JCO.1999.17.3.784. [DOI] [PubMed] [Google Scholar]
- 12.Tai WM, Quah D, Yap SP, Tan SH, Tang T, Tay KW, et al. Primary mediastinal large B-cell lymphoma: Optimal therapy and prognostic factors in 41 consecutive Asian patients. Leuk Lymphoma. 2011;52:604–12. doi: 10.3109/10428194.2010.550073. [DOI] [PubMed] [Google Scholar]
- 13.Avilés A, Neri N, Fernández R, Huerta-Guzmán J, Nambo MJ. Randomized clinical trial to assess the efficacy of radiotherapy in primary mediastinal large B-lymphoma. Int J Radiat Oncol Biol Phys. 2012;83:1227–31. doi: 10.1016/j.ijrobp.2011.09.012. [DOI] [PubMed] [Google Scholar]
- 14.Zhu YJ, Huang JJ, Xia Y, Zhao W, Jiang WQ, Lin TY, et al. Primary mediastinal large B-cell lymphoma (PMLBCL) in Chinese patients: Clinical characteristics and prognostic factors. Int J Hematol. 2011;94:178–84. doi: 10.1007/s12185-011-0898-4. [DOI] [PubMed] [Google Scholar]
- 15.Rodríguez J, Conde E, Gutiérrez A, García JC, Lahuerta JJ, Varela MR, et al. Primary mediastinal large cell lymphoma (PMBL): Frontline treatment with autologous stem cell transplantation (ASCT).The GEL-TAMO experience. Hematol Oncol. 2008;26:171–8. doi: 10.1002/hon.858. [DOI] [PubMed] [Google Scholar]


