Fig. 1.
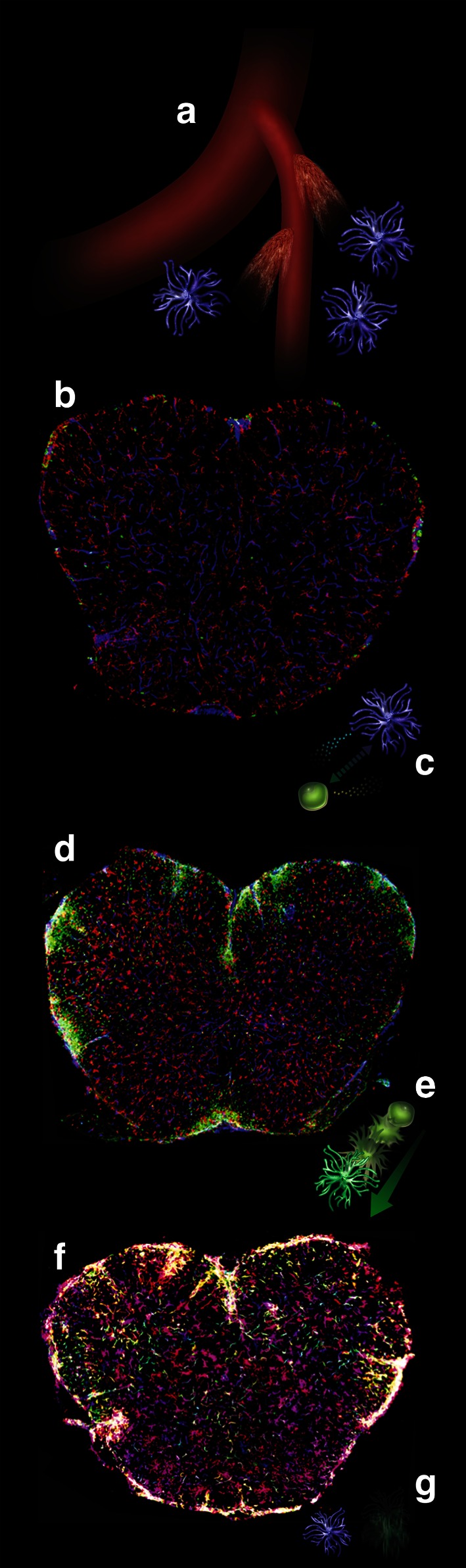
Illustration of the multiple roles of microglia during the initiation, progression and resolution of experimental autoimmune encephalitis. The spinal cord sections are derived from mice in which circulating cells and their progeny are marked by GFP expression (green), while tissue-resident microglia are not (see text). a Microscopic leaks in the CNS vasculature allow the extravasation of plasma components such as fibrinogen, which contributes to the induction of microglia expansion. b This leads to microgliosis well before circulating cells are capable of crossing the blood–brain barrier. Staining for the mature microglia/macrophage marker IBA-1 is shown in red, staining for CD31 (endothelium) in blue, circulating cells are green. c Expanded microglia play a role in attracting circulating inflammatory monocytes, possibly by the expression of chemokines such as CCL2/MCP1. d Inflammatory monocytes infiltrate the CNS parenchyma and, through a variety of mechanisms likely to involve myelin stripping and secretion of neurotoxic cytokines, exacerbate the damage and trigger progression toward severe disease. e, f Next, inflammatory monocytes mature into IBA-1 expressing macrophages, adopting a microglia-like morphology. This signals the beginning of remission. g Eventually, macrophages derived from circulating monocytes are completely cleared from the CNS, while microglia is reduced in numbers but persists to maintain the resident population of innate immune cells
