Abstract
Background
Little is known if the levels of physical activity required for the prevention of incident heart failure (HF) and other cardiovascular events vary in community-dwelling older adults.
Methods
We studied 5503 Cardiovascular Health Study (CHS) participants, age ≥65 years, free of baseline HF. Weekly metabolic equivalent task-minutes (MET-minutes), estimated using baseline total leisure-time energy expenditure, were used to categorize participants into four physical activity groups: inactive (0 MET-minutes; n=489; reference), low (1–499; n=1458), medium (500–999; n=1086) and high (≥1000; n=2470).
Results
Participants had a mean (±SD) age of 73 (±6) years, 58% were women, and 15% African American. During 13 years of follow-up, centrally-adjudicated incident HF occurred in 26%, 23%, 20%, and 19% of participants with no, low, medium and high physical activity, respectively (trend p <0.001). Compared with inactive older adults, age-sex-race-adjusted hazard ratios (95% confidence intervals) for incident HF associated with low, medium and high physical activity were 0.87 (0.71–1.06; p=0.170), 0.68 (0.54–0.85; p=0.001) and 0.60 (0.49–0.74; p<0.001), respectively (trend p <0.001). Only high physical activity had significant independent association with lower risk of incident HF (HR, 0.79; 95% CI, 0.64–0.97; p=0.026). All levels of physical activity had significant independent association with lower risk of incident acute myocardial infarction (AMI), stroke and cardiovascular mortality.
Conclusion
In community-dwelling older adults, high level of physical activity was associated with lower risk of incident HF, but all levels of physical activity were associated with lower risk of incident AMI, stroke, and cardiovascular mortality.
Keywords: Physical activity, MET-minutes, Incident heart failure, Older adults
1. Introduction
Physical activity has been shown to reduce the risk of incident cardiovascular events including incident heart failure (HF) [1–4]. However, the association of physical activity expressed as metabolic equivalent task-minutes (MET-minutes) with incident HF and other cardiovascular events in community-dwelling older adults has not been previously studied. The United States Department of Health and Human Services’ 2008 Physical Activity Guidelines for Americans categorized physical activity into three categories based on weekly MET-minutes: 1–499, 500–999, and ≥1000 and recommended that physical activity at 1–499 MET-minutes per week would provide some health benefits, physical activity at 500–999 MET-minutes per week would provide substantial health benefits, and physical activity at ≥1000 MET-minutes per week would provide additional health benefits [5]. Therefore, the purpose of the current study is to determine the association of physical activity by weekly MET-minutes categories with incident HF and other cardiovascular events in community-dwelling older adults and to examine if these associations varied by levels of physical activity.
2. Methods
2.1. Data source and study participants
Sponsored by the National Heart, Lung and Blood Institute (NHLBI), the Cardiovascular Health Study (CHS) is an ongoing, prospective, community-based epidemiologic study of cardiovascular disease risk factors in older adults. CHS participants included 5888 community-dwelling older adults, aged 65 years and older, and were recruited from Forsyth County, North Carolina, Sacramento County, California, Washington County, Maryland, and Pittsburgh County, Pennsylvania. The rationale and design of the CHS have been previously reported [6]. Participants were recruited from a random sample of Medicare-eligible older adults in two phases. An initial cohort of 5201 participants was recruited between 1989 and 1990, and a second cohort of 687 African American participants were recruited between 1992 and 1993 [6]. The current analysis is based on a public-use copy of the CHS data. Of the 5888 CHS participants, 93 did not consent to be included in the de-identified public-use data. Of the remaining 5795 participants, 20 without data on baseline physical activity (kilocalories of energy expended per week in leisure-time) and 272 with baseline prevalent HF were excluded and the final cohort was comprised of 5503 CHS participants.
2.2. Physical activity and other baseline characteristics
Baseline leisure-time physical activity was assessed using a modified Minnesota Leisure-Time Activities questionnaire, which evaluated frequency and duration of 15 different activities during a 2 week period and was used to estimate kilocalories of energy expended per week [7]. MET-minutes were calculated by following formula, total kilocalories per week = total MET-minutes per week × 0.0175 × body weight in kilogram. Based on the MET-minutes cutoffs used in the 2008 Physical Activity Guidelines for Americans, we categorized participants into four physical activity groups: inactive (0; n=489), low (1–499; n=1458), medium (500–999; n=1086), and high (≥1000; n=2470) [5]. Data on other characteristics (Table 1) were collected at baseline. Missing values for covariates were imputed based on values predicted by age, sex and race.
Table 1.
Baseline characteristics by physical activity categories
| Mean (±SD) or n (%) | Physical Activity in MET-minutes/week |
||||
|---|---|---|---|---|---|
| 0 (n=489) |
1–499 (n=1458) |
500–999 (n=1086) |
≥1000 (n=2470) |
P value for linear trend |
|
| Age, years | 75 (±6) | 74 (±6) | 73 (±5) | 73 (±5) | <0.001 |
| Female | 316 (65%) | 877 (60%) | 612 (56%) | 1375 (56%) | <0.001 |
| African American | 103 (21%) | 358 (25%) | 154 (14%) | 225 (9%) | <0.001 |
| Education higher than high school | 186 (38%) | 577 (40%) | 475 (44%) | 1130 (46%) | <0.001 |
| Income >25K | 157 (32%) | 477 (33%) | 401 (37%) | 1012 (41%) | <0.001 |
| Alcohol, drinks per week | 2.0 (±6.5) | 2.3 (±6.6) | 2.6 (±6.6) | 2.6 (±6.2) | 0.134 |
| Smoke, pack-years | 19 (±31) | 18 (±26) | 18 (±27) | 17 (±26) | 0.277 |
| Never eat chicken skin | 325 (67%) | 942 (65%) | 733 (68%) | 1799 (73%) | <0.001 |
| Body mass index, kg/m2 | 27 (±4) | 28 (±4) | 27 (±4) | 26 (±4) | <0.001 |
| Systolic blood pressure, mmHg | 140 (±23) | 138 (±22) | 136 (±21) | 135 (±21) | <0.001 |
| Diastolic blood pressure, mmHg | 72 (±12) | 72 (±11) | 71 (±11) | 70 (±11) | <0.001 |
| Medical problems | |||||
| Coronary heart diseases | 111 (23%) | 272 (19%) | 183 (17%) | 393 (16%) | <0.001 |
| Acute myocardial infarction | 52 (11%) | 122 (8%) | 84 (8%) | 184 (7%) | 0.032 |
| Angina pectoris | 96 (20%) | 231 (16%) | 147 (14%) | 321 (13%) | <0.001 |
| Hypertension | 326 (67%) | 923 (63%) | 636 (59%) | 1330 (54%) | <0.001 |
| Diabetes mellitus | 106 (22%) | 272 (19%) | 165 (15%) | 315 (13%) | <0.001 |
| Stroke | 42 (9%) | 65 (4%) | 35 (3%) | 71 (3%) | <0.001 |
| Atrial fibrillation | 16 (3%) | 36 (2%) | 17 (2%) | 46 (2%) | 0.038 |
| Left ventricular hypertrophy by electrocardiogram | 37 (8%) | 69 (5%) | 42 (4%) | 91 (4%) | 0.001 |
| Left ventricular systolic dysfunction by echocardiogram | 44 (9%) | 111 (8%) | 90 (8%) | 165 (7%) | 0.070 |
| Arthritis | 306 (63%) | 773 (53%) | 548 (51%) | 1228 (50%) | <0.001 |
| Chronic obstructive pulmonary disease | 81 (17%) | 200 (14%) | 140 (13%) | 265 (11%) | <0.001 |
| Cancer | 67 (14%) | 230 (16%) | 161 (15%) | 335 (14%) | 0.208 |
| Geriatric problems | |||||
| Activity of daily living | 0.39 (±0.9) | 0.15 (±0.5) | 0.08 (±0.4) | 0.06 (±0.3) | <0.001 |
| Instrumental activity of daily living | 0.86 (±1.2) | 0.43 (±0.8) | 0.30 (±0.6) | 0.18 (±0.5) | <0.001 |
| Blocks walked last week | 13 (±30) | 20 (±32) | 38 (±46) | 56 (±66) | <0.001 |
| Time to walk 15 ft | 6.9 (±3.1) | 6.1 (±2.4) | 5.7 (±1.8) | 5.4 (±2.0) | <0.001 |
| Mini mental state examination score | 26.8 (±3.4) | 27.3 (±3.0) | 27.8 (±2.4) | 27.8 (±2.4) | <0.001 |
| Depression score | 6.0 (±5.3) | 5.2 (±4.7) | 4.5 (±4.3) | 4.1 (±4.2) | <0.001 |
| Loss of balance | 150 (31%) | 377 (26%) | 237 (22%) | 502 (20%) | <0.001 |
| Frequent fall | 35 (7%) | 54 (4%) | 34 (3%) | 57 (2%) | <0.001 |
| Orthostatic dizziness | 149 (31%) | 317 (22%) | 235 (22%) | 425 (17%) | <0.001 |
| Laboratory measures | |||||
| Serum cholesterol, mg/dL | 219 (±42) | 211 (±40) | 211 (±38) | 212 (±38) | 0.001 |
| Serum triglyceride, mg/dL | 152.7 (±96.4) | 141.3 (±70.8) | 142.0 (±82.5) | 134.7 (±72.8) | <0.001 |
| Serum creatinine, mg/dL | 1.01 (±0.46) | 0.98 (±0.45) | 0.95 (±0.39) | 0.93 (±0.31) | <0.001 |
| Serum potassium, mEq/L | 4.1 (±0.40) | 4.1 (±0.39) | 4.2 (±0.37) | 4.2 (±0.37) | 0.001 |
| Serum glucose, mg/dL | 116 (±42) | 115 (±40) | 111 (±38) | 107 (±32) | <0.001 |
| Serum albumin, g/dL | 4.0 (±0.3) | 4.0 (±0.3) | 4.0 (±0.3) | 4.0 (±0.3) | 0.176 |
| Serum uric acid, mg/dL | 6.0 (±1.7) | 5.8 (±1.5) | 5.7 (±1.5) | 5.5 (±1.4) | <0.001 |
| Serum C-reactive protein, mg/dL | 5.7 (±7.8) | 5.6 (±9.3) | 4.4 (±8.0) | 4.0 (±7.3) | <0.001 |
| Serum interleukin-6, pg/mL | 2.6 (±1.7) | 2.4 (±1.9) | 2.1 (±1.6) | 2.0 (±1.8) | <0.001 |
| Serum insulin, µIU/mL | 18.8 (±25.3) | 18.9 (±29.6) | 16.1 (±20.7) | 15.2 (±21.6) | <0.001 |
| Fibrinogen, mg/dL | 337 (±74) | 331 (±69) | 320 (±65) | 316 (±62) | <0.001 |
| Serum coagulation factor-VII, % | 129 (±33) | 124 (±29) | 124 (±28) | 122 (±29) | <0.001 |
| Hemoglobin, g/dL | 13.9 (±1.38) | 13.9 (±1.43) | 14.1 (±1.29) | 14.1 (±1.31) | <0.001 |
| Platelet count, 103/µL | 260 (±89) | 250 (±72) | 245 (±69) | 252 (±76) | 0.001 |
Abbreviation: MET, metabolic equivalent task; SD, standard deviation
2.3. Incident heart failure and other cardiovascular events
The primary outcome for this study was incident HF during 13 years of follow-up. Incident HF was centrally-adjudicated by the CHS Events Committee [8–15]. The process began with self-reports of physician-diagnosed HF, which was then confirmed by review of medical records for symptoms, signs, medications, and other evidence of HF. The CHS criteria for HF diagnosis have been shown to be more stringent than those used in the Framingham Heart Study [16]. Secondary outcomes included incident acute myocardial infarction (AMI), angina pectoris, stroke, all-cause mortality and cause-specific mortality.
2.4. Statistical analysis
For descriptive analyses, we used Pearson’s Chi-square test for categorical variables and ANOVA analysis for continuous variables. Kaplan Meier survival analysis was used to determine the association of physical activity with incident HF during 13 years of follow-up. Hazard ratios (HR) and 95% confidence intervals (CI) for centrally-adjudicated incident HF and other secondary outcomes were estimated using Cox proportional hazard models adjusting for all variables in Table 1. Trend tests were conducted using median values for the four MET-minutes categories. In addition, we also separately examined the effect of physical activity using kilocalories of energy expended per week in leisure-time [17]. All statistical tests were two-sided, and tests with p-value <0.05 were considered significant. SPSS for Windows (Version 20) was used for data analysis.
3. Results
3.1. Baseline characteristics
Participants (n=5503) had a mean (±SD) age of 73 (±6) years, 58% were women, and 15% were African American. Participants with higher levels of prevalent physical activity were more likely to be younger, male, Caucasians, and have higher levels of education and income (Table 1). They were also more likely to have lower prevalence of cardiovascular risk factors such as hypertension, diabetes, coronary artery disease, AMI, stroke, left ventricular hypertrophy, and have lower mean blood pressure, serum cholesterol, serum creatinine and serum C-reactive protein (Table 1).
3.2. Association of baseline physical activity with incident heart failure
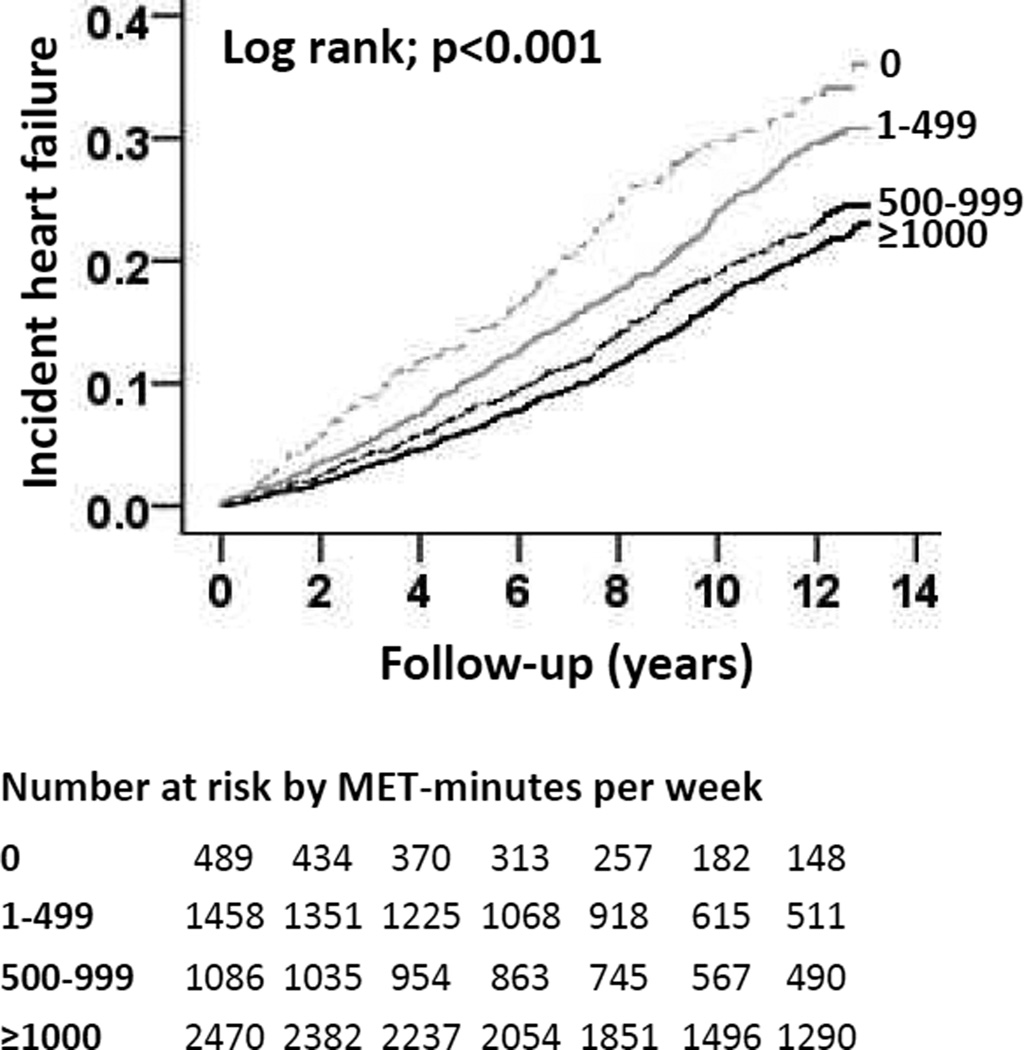
During 13 years of follow-up, centrally-adjudicated incident HF occurred in 26%, 23%, 20%, and 19% of participants with no, low, medium and high physical activity, respectively, with corresponding HRs of 1.00 (reference), 0.79 (95% CI, 0.64–0.97; p=0.022), 0.61 (95% CI, 0.49–0.75; p<0.001) and 0.53 (95% CI, 0.44–0.65; p<0.001; Table 2 and Figure 1). When adjusted for age, sex, and race, only medium (HR, 0.68; 95% CI, 0.54–0.85; p=0.001) and high (HR, 0.60; 95% CI, 0.49–0.74; p<0.001) levels of physical activity were associated with reduced risk of incident HF (Table 2). After additional adjustment for other risk factors, only high level physical activity was associated with a significant independent reduction in the risk of incident HF (HR, 0.79; 95% CI, 0.64–0.97; p=0.026; Table 2). In all models, there were significant dose-response relationships between levels of physical activity and risk of incident HF (Table 2).
Table 2.
Association of physical activity across MET-minutes/week categories with incident heart failure
| MET-minutes/week | % (events/total) | Hazard ratio (95% confidence interval) |
||
|---|---|---|---|---|
| Unadjusted | Age-sex-race-adjusted | Multivariable-adjusted* | ||
| 0 | 26 (128/489) | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| 1–499 | 23 (338/1458) | 0.79 (0.64–0.97); p=0.022 | 0.87 (0.71–1.06); p=0.170 | 0.97 (0.79–1.20); p=0.807 |
| 500–999 | 20 (213/1086) | 0.61 (0.49–0.75); p<0.001 | 0.68 (0.54–0.85); p=0.001 | 0.86 (0.69–1.08); p=0.201 |
| ≥1000 | 19 (458/2470) | 0.53 (0.44–0.65); p<0.001 | 0.60 (0.49–0.74); p<0.001 | 0.79 (0.64–0.97); p=0.026 |
| P trend# | <0.001 | <0.001 | <0.001 | 0.003 |
Abbreviation: MET, metabolic equivalent task
Adjusted with age, sex, race, education, income, alcohol, smoking, body mass index, coronary artery disease, acute myocardial infarction, hypertension, diabetes, stroke, atrial fibrillation, left ventricular hypertrophy, left ventricular systolic dysfunction, systolic blood pressure, diastolic blood pressure, depression score, Mini-mental state examination score, serum cholesterol, serum albumin, serum creatinine and serum C-reactive protein
Median value for each category: 0 = 0, 1–499 = 253.00, 500–999 = 729.50, ≥1000 = 2054.50
Figure 1.
Kaplan-Meier plot displaying unadjusted association of physical activity levels by metabolic equivalent task-minutes (MET-minutes) per week categories and incident heart failure in the Cardiovascular Health Study (CHS)
3.3. Association of baseline physical activity with other incident cardiovascular events
Compared with no physical activity, all levels of prevalent physical activity were associated with unadjusted and age-sex-race-adjusted reduced risk of incident angina pectoris, AMI and stroke (Table 3). In addition, all levels of physical activity had significant multivariable-adjusted independent associations with reduced risk of AMI and stroke (Table 3).
Table 3.
Association of physical activity across MET-minutes/week categories with other incident cardiovascular events
| MET-minutes/week | % (events/total) | Hazard ratio (95% confidence interval) |
||
|---|---|---|---|---|
| Unadjusted | Age-sex-race-adjusted | Multivariable-adjusted** | ||
| Acute myocardial infarction* (n=5061) | ||||
| 0 | 15 (67/437) | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| 1–499 | 11 (146/1336) | 0.63 (0.48–0.85); p=0.002 | 0.63 (0.47–0.85); p=0.002 | 0.68 (0.51–0.91); p=0.010 |
| 500–999 | 11 (107/1002) | 0.57 (0.42–0.78); p<0.001 | 0.56 (0.41–0.76); p<0.001 | 0.65 (0.47–0.89); p=0.007 |
| ≥1000 | 12 (266/2286) | 0.60 (0.46–0.78); p<0.001 | 0.58 (0.44–0.76); p<0.001 | 0.68 (0.51–0.91); p=0.008 |
| P trend# | 0.331 | 0.065 | 0.038 | 0.361 |
| Angina pectoris* (n=4708) | ||||
| 0 | 22 (88/393) | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| 1–499 | 19 (230/1227) | 0.75 (0.59–0.96); p=0.021 | 0.74 (0.58–0.95); p=0.017 | 0.79 (0.62–1.01); p=0.062 |
| 500–999 | 19 (176/939) | 0.70 (0.54–0.91); p=0.007 | 0.68 (0.53–0.88); p=0.004 | 0.79 (0.61–1.03); p=0.079 |
| ≥1000 | 19 (406/2149) | 0.67 (0.54–0.85); p=0.001 | 0.66 (0.52–0.83); p<0.001 | 0.79 (0.62–1.01); p=0.056 |
| P trend## | 0.347 | 0.018 | 0.013 | 0.459 |
| Stroke* (n=5290) | ||||
| 0 | 19 (84/447) | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| 1–499 | 14 (188/1393) | 0.64 (0.50–0.83); p=0.001 | 0.71 (0.55–0.92); p=0.011 | 0.76 (0.59–0.99); p=0.042 |
| 500–999 | 12 (127/1051) | 0.53 (0.40–0.70); p<0.001 | 0.60 (0.46–0.80); p<0.001 | 0.68 (0.52–0.91); p=0.008 |
| ≥1000 | 14 (323/2399) | 0.56 (0.44–0.72); p<0.001 | 0.66 (0.52–0.85); p=0.001 | 0.75 (0.58–0.96); p=0.022 |
| P trend### | 0.060 | 0.006 | 0.096 | 0.376 |
Abbreviation: MET, metabolic equivalent task
Exclude prevalent disease events
Adjusted with age, sex, race, education, income, alcohol, smoking, body mass index, coronary artery disease, acute myocardial infarction, hypertension, diabetes, stroke, atrial fibrillation, left ventricular hypertrophy, left ventricular systolic dysfunction, systolic blood pressure, diastolic blood pressure, depression score, Mini-mental state examination score, serum cholesterol, serum albumin, serum creatinine and serum C-reactive protein
Median value for each category: 0 = 0, 1–499 = 254.00, 500–999 = 725.45, ≥1000 = 2061.63
Median value for each category: 0 = 0, 1–499 = 255.89, 500–999 = 729.73, ≥1000 = 2051.98
Median value for each category: 0 = 0, 1–499 = 254.17, 500–999 = 724.50, ≥1000 = 2051.65
3.4. Association of baseline physical activity with mortality
Compared with no physical activity, all levels of physical activity were associated with unadjusted and age-sex-race-adjusted lower risk all-cause and cardiovascular mortality (Table 4). All levels of physical activity also had significant multivariable-adjusted associations with lower risk of cardiovascular mortality (Table 4). In all models, there were significant dose-response relationship between levels of physical activity and risk of total and cardiovascular mortality (Table 4).
Table 4.
Association of physical activity across MET-minutes/week categories with mortality
| MET-minutes/week | % (events/total) | Hazard ratio (95% confidence interval) |
||
|---|---|---|---|---|
| Unadjusted | Age-sex-race-adjusted | Multivariable-adjusted* | ||
| All-cause mortality | ||||
| 0 | 59 (286/489) | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| 1–499 | 48 (703/1458) | 0.73 (0.64–0.84); p<0.001 | 0.82 (0.71–0.94); p=0.005 | 0.89 (0.77–1.02); p=0.094 |
| 500–999 | 43 (471/1086) | 0.60 (0.52–0.70); p<0.001 | 0.69 (0.59–0.80); p<0.001 | 0.79 (0.68–0.92); p=0.002 |
| ≥1000 | 39 (966/2470) | 0.50 (0.44–0.57); p<0.001 | 0.59 (0.51–0.67); p<0.001 | 0.67 (0.59–0.77); p<0.001 |
| P trend# | <0.001 | <0.001 | <0.001 | <0.001 |
| Cardiovascular mortality | ||||
| 0 | 28 (136/489) | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| 1–499 | 19 (270/1458) | 0.59 (0.48–0.73); p<0.001 | 0.67 (0.54–0.82); p<0.001 | 0.76 (0.62–0.94); p=0.011 |
| 500–999 | 17 (181/1086) | 0.49 (0.39–0.61); p<0.001 | 0.56 (0.45–0.70); p<0.001 | 0.72 (0.57–0.91); p=0.006 |
| ≥1000 | 16 (390/2470) | 0.43 (0.35–0.52); p<0.001 | 0.50 (0.41–0.61); p<0.001 | 0.65 (0.52–0.79); p<0.001 |
| P trend# | <0.001 | <0.001 | <0.001 | 0.001 |
| Non-cardiovascular mortality | ||||
| 0 | 31 (149/489) | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| 1–499 | 29 (429/1458) | 0.86 (0.71–1.03); p=0.099 | 0.96 (0.79–1.15); p=0.641 | 1.00 (0.83–1.21); p=0.984 |
| 500–999 | 27 (289/1086) | 0.71 (0.58–0.86); p=0.001 | 0.81 (0.66–0.99); p=0.037 | 0.86 (0.70–1.06); p=0.149 |
| ≥1000 | 23 (575/2470) | 0.57 (0.48–0.68); p<0.001 | 0.67 (0.55–0.80); p<0.001 | 0.71 (0.59–0.86); p<0.001 |
| P trend# | <0.001 | <0.001 | <0.001 | <0.001 |
Abbreviation: MET, metabolic equivalent task
Adjusted with age, sex, race, education, income, alcohol, smoking, body mass index, coronary artery disease, acute myocardial infarction, hypertension, diabetes, stroke, atrial fibrillation, left ventricular hypertrophy, left ventricular systolic dysfunction, systolic blood pressure, diastolic blood pressure, depression score, Mini-mental state examination score, serum cholesterol, serum albumin, serum creatinine and serum C-reactive protein
Median value for each category: 0 = 0, 1–499 = 253.00, 500–999 = 729.50, ≥1000 = 2054.50
3.5. Association of baseline physical activity (Kcal/week) with outcomes
When we categorized participants into four physical activity groups using Kcal/week cutoffs: inactive (0; n=489), low (1–499; n=1165), medium (500–999; n=981), and high (≥1000; n=2868), similar associations with outcomes were observed.
4. Discussion
Findings from the current study demonstrate that among community-dwelling older adults, all levels of physical activity had significant independent associations with lower risk of incident AMI, stroke, and cardiovascular mortality. However, only high level of physical activity was associated with significant independent lower risk of incident HF and non-cardiovascular mortality. These findings suggest that although low physical activity may reduce the risk of AMI, a major HF risk factor, to reduce the risk of HF, high level of physical activity may be required.
The modest attenuation of the unadjusted associations of physical activity with incident HF and other outcomes after adjustment for age, sex and race is likely due to younger age of those with higher physical activity. Further attenuation of these associations after multivariable adjustment suggests confounding by other baseline characteristics. Although some of the baseline characteristics such as arthritis, chronic obstructive pulmonary disease and stroke may have affected baseline physical activity, HF risk factors such as hypertension, coronary artery disease, and diabetes may have a bi-directional association with physical activity. Baseline physical activity in CHS was ascertained by that performed during two weeks prior to study baseline. However, if the onset of physical activity was long before baseline, then it may have affected some baseline HF risk factors (mediators), and in that case, an adjustment of these potential mediators may result in underestimation of true associations [18, 19]. Therefore, the age-sex-race-adjusted associations are likely closer to the true associations, which were likely be underestimated by multivariable adjustments of baseline cardiovascular risk factors or mediators that may have been affected by prior physical activity [19].
Findings from the current study suggest that older adults beginning low (1–499 MET-minutes) level of physical activity at or after age 65 years may be able to significantly reduce their risk of incident AMI, stroke and cardiovascular mortality. Although there seems to be no additional reduction in the risk of incident AMI and stroke with higher levels of physical activity, the risk for cardiovascular mortality seems to reduce further with higher levels of physical activity. Additionally, high level of physical activity was also associated with the lower risk of non-cardiovascular death. Finally, high level of physical activity (≥1000 MET-minutes; which is equivalent to greater than 300 minutes (5 hours) of moderate-intensity activity or 150 minutes (2.5 hours) of vigorous-intensity physical activity per week) also seemed to reduce the risk of incident HF. Findings from a recent mechanistic study based on CHS suggest that the cardiovascular benefit of physical activity may be mediated by prevention of neurohormonal activation and cardiac injury [4].
The cardiovascular benefits of physical activity in general have been well described [7, 20, 21]. Several previous studies reported the associations between physical activity and reduction in the risk of incident HF [1–4, 22, 23]. However, to the best of our knowledge, this is the first study of the association of baseline physical activity as quantified by MET-minutes per week with HF and other cardiovascular events in community-dwelling older adults. MET is the ratio of the rate of energy expended during an activity to the rate of energy expended at rest [5]. MET-minute is a useful unit for describing the energy expenditure of a specific physical activity and to compare total amount of physical activity across various persons and types of activities. According to the U.S. Department of Health and Human Services 2008 Physical Activity Guidelines for Americans, medium level of physical activity (500 to 1,000 MET-minutes per week) can be accomplished by 150–300 minutes of moderate-intensity physical activity per week, 75–150 minutes of vigorous-intensity physical activity per week, or an equivalent combination of moderate and vigorous-intensity physical activity [5].
Limitations
Our study has several limitations. Despite attempts to adjust for confounding risk factors using multivariate modeling, residual bias and bias due to unmeasured confounders are possible. Further, we were not able to account for the duration and severity of many risk factors in the study population both prior to baseline and during follow-up. Although the Minnesota Leisure Time Physical Activity questionnaire has been well validated with direct measures of physical activity, it may not have adequately captured subject’s level of physical activity over the duration of follow-up in the older population. In addition, the questionnaire is self-reported and may over- or under-estimate physical activity. Finally, we had no data on left ventricular ejection fraction for those with incident HF, which limited our ability to study whether level of physical activity may have any differential effect on incident systolic versus diastolic HF.
In conclusion, in community-dwelling older adults, all levels of physical activity were associated with lower risk of incident AMI, stroke, and cardiovascular mortality. However, high level of physical activity was also associated with additional health benefit of lower risk of incident HF and non-cardiovascular mortality.
Acknowledgement
Funding/Support: Dr. Allman is supported in part by NIH/NCRR grant 5UL1 RR025777.
The Cardiovascular Health Study (CHS) was conducted and supported by the NHLBI in collaboration with the CHS investigators. This manuscript was prepared using a limited access dataset obtained by the NHLBI and does not necessarily reflect the opinions or views of the CHS Study or the NHLBI.
The authors of this manuscript have certified that they comply with the Principles of Ethical Publishing in the International Journal of Cardiology [24].
Footnotes
Conflict of Interest Disclosures: None
References
- 1.Hu G, Jousilahti P, Antikainen R, Katzmarzyk PT, Tuomilehto J. Joint effects of physical activity, body mass index, waist circumference, and waist-to-hip ratio on the risk of heart failure. Circulation. 2010;121:237–244. doi: 10.1161/CIRCULATIONAHA.109.887893. [DOI] [PubMed] [Google Scholar]
- 2.He J, Ogden LG, Bazzano LA, Vupputuri S, Loria C, Whelton PK. Risk factors for congestive heart failure in US men and women: NHANES I epidemiologic follow-up study. Arch Intern Med. 2001;161:996–1002. doi: 10.1001/archinte.161.7.996. [DOI] [PubMed] [Google Scholar]
- 3.Kenchaiah S, Sesso HD, Gaziano JM. Body mass index and vigorous physical activity and the risk of heart failure among men. Circulation. 2009;119:44–52. doi: 10.1161/CIRCULATIONAHA.108.807289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Defilippi CR, de Lemos JA, Tkaczuk AT, et al. Physical Activity, Change in Biomarkers of Myocardial Stress and Injury, and Subsequent Heart Failure Risk in Older Adults. J Am Coll Cardiol. 2012 Dec 18;60(24):2539–2547. doi: 10.1016/j.jacc.2012.08.1006. Epub 2012 Nov 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.U.S. Department of Health and Human Services (HHS) Physical Activity Guidelines for Americans. 2008 http://www.health.gov/paguidelines/guidelines/chapter1.aspx.
- 6.Fried LP, Borhani NO, Enright P, et al. The Cardiovascular Health Study: design and rationale. Ann Epidemiol. 1991;1:263–276. doi: 10.1016/1047-2797(91)90005-w. [DOI] [PubMed] [Google Scholar]
- 7.Siscovick DS, Fried L, Mittelmark M, Rutan G, Bild D, O'Leary DH. Exercise intensity and subclinical cardiovascular disease in the elderly. The Cardiovascular Health Study. Am J Epidemiol. 1997;145:977–986. doi: 10.1093/oxfordjournals.aje.a009066. [DOI] [PubMed] [Google Scholar]
- 8.Ives DG, Fitzpatrick AL, Bild DE, et al. Surveillance and ascertainment of cardiovascular events. The Cardiovascular Health Study. Ann Epidemiol. 1995;5:278–285. doi: 10.1016/1047-2797(94)00093-9. [DOI] [PubMed] [Google Scholar]
- 9.Filippatos GS, Desai RV, Ahmed MI, et al. Hypoalbuminaemia and incident heart failure in older adults. Eur J Heart Fail. 2011;13:1078–1086. doi: 10.1093/eurjhf/hfr088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ekundayo OJ, Dell'Italia LJ, Sanders PW, et al. Association between hyperuricemia and incident heart failure among older adults: A propensity-matched study. International Journal of Cardiology. 2010;142:279–287. doi: 10.1016/j.ijcard.2009.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guichard JL, Desai RV, Ahmed MI, et al. Isolated diastolic hypotension and incident heart failure in older adults. Hypertension. 2011;58:895–901. doi: 10.1161/HYPERTENSIONAHA.111.178178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bowling CB, Feller MA, Mujib M, et al. Relationship between Stage of Kidney Disease and Incident Heart Failure in Older Adults. American Journal of Nephrology. 2011;34:135–141. doi: 10.1159/000328905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carbone L, Buzkova P, Fink HA, et al. Hip fractures and heart failure: findings from the Cardiovascular Health Study. Eur Heart J. 2010;31:77–84. doi: 10.1093/eurheartj/ehp483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gottdiener JS, Arnold AM, Aurigemma GP, et al. Predictors of congestive heart failure in the elderly: the Cardiovascular Health Study. J Am Coll Cardiol. 2000;35:1628–1637. doi: 10.1016/s0735-1097(00)00582-9. [DOI] [PubMed] [Google Scholar]
- 15.Gottdiener JS, McClelland RL, Marshall R, et al. Outcome of congestive heart failure in elderly persons: influence of left ventricular systolic function. The Cardiovascular Health Study. Ann Intern Med. 2002;137:631–639. doi: 10.7326/0003-4819-137-8-200210150-00006. [DOI] [PubMed] [Google Scholar]
- 16.Schellenbaum GD, Rea TD, Heckbert SR, et al. Survival associated with two sets of diagnostic criteria for congestive heart failure. Am J Epidemiol. 2004;160:628–635. doi: 10.1093/aje/kwh268. [DOI] [PubMed] [Google Scholar]
- 17.Sesso HD, Paffenbarger RS, Ha T, Lee IM. Physical activity and cardiovascular disease risk in middle-aged and older women. Am J Epidemiol. 1999;150:408–416. doi: 10.1093/oxfordjournals.aje.a010020. [DOI] [PubMed] [Google Scholar]
- 18.Hernan MA, Hernandez-Diaz S, Robins JM. A structural approach to selection bias. Epidemiology. 2004;15:615–625. doi: 10.1097/01.ede.0000135174.63482.43. [DOI] [PubMed] [Google Scholar]
- 19.Danaei G, Tavakkoli M, Hernan MA. Bias in observational studies of prevalent users: lessons for comparative effectiveness research from a meta-analysis of statins. Am J Epidemiol. 2012;175:250–262. doi: 10.1093/aje/kwr301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mozaffarian D, Furberg CD, Psaty BM, Siscovick D. Physical activity and incidence of atrial fibrillation in older adults: the cardiovascular health study. Circulation. 2008;118:800–807. doi: 10.1161/CIRCULATIONAHA.108.785626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sui XM, LaMonte MJ, Laditka JN, et al. Cardiorespiratory fitness and adiposity as mortality predictors in older adults. Jama-Journal of the American Medical Association. 2007;298:2507–2516. doi: 10.1001/jama.298.21.2507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Djousse L, Driver JA, Gaziano JM. Relation between modifiable lifestyle factors and lifetime risk of heart failure. JAMA. 2009;302:394–400. doi: 10.1001/jama.2009.1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang Y, Tuomilehto J, Jousilahti P, et al. Occupational, commuting, and leisure-time physical activity in relation to heart failure among finnish men and women. J Am Coll Cardiol. 2010;56:1140–1148. doi: 10.1016/j.jacc.2010.05.035. [DOI] [PubMed] [Google Scholar]
- 24.Shewan LG, Coats AJ. Ethics in the authorship and publishing of scientific articles. Int J Cardiol. 2010;144:1–2. [Google Scholar]