Abstract
Clinical documentation and health information portability pose unique challenges in urban and rural areas of India. This article presents findings of a pilot study conducted in a primary health center in rural India. In this article, we focus on primary care in rural India and how a portable health record system could facilitate the availability of medical information at the point of care. We followed a geriatric cohort and a maternal cohort of 308 participants over a nine-month period. Physician encounters were entered into a web-based electronic health record. This information was made available to all study participants through a short messaging service (SMS). Additionally, 135 randomly selected participants from the cohort were issued a USB-based memory card that contained their detailed health records and could be viewed on most computers. The dual portability model implemented in the pilot study demonstrates the utility of the concept.
Key words: electronic health record (EHR), health information technology, health information portability, portable health record, SMS, primary care
Introduction
The quality of healthcare depends on many factors, including timely availability of a patient's medical information. A wide gap in healthcare services exists between rural and urban areas of India. More than 70 percent of healthcare providers are concentrated in urban settings, which house less than 30 percent of the overall population.1 Also, literacy rates vary between rural and urban areas in India. Rural areas report a literacy rate of 68.9 percent, whereas urban areas report 85 percent.2 However, mobile phones have high penetration rates in rural as well as urban areas of the country. Of the total telecom subscriber base in India, close to 94 percent are wireless subscribers.3 A new mobile connection can be attained and activated for as low as 15 cents per month.4 Therefore, the use of low-cost, easy-to-use technologies using mobile telephony may help bridge some of the gaps in patient-provider interactions.
Traditionally in India, patient medical records have been paper based and continue to be confined to the facility that the patient has attended. Because of the nature of the healthcare system in India, which includes primary, secondary, and tertiary healthcare facilities spread across both government and private sectors, the options of healthcare providers are practically endless.5 What might have started off as a few lines of medical notes are transformed into multiple records spanning several hundred pages over a patient's lifetime. From the perspective of the physician, availability of information in a timely manner would have a substantial impact on patient outcomes. Since the introduction of the electronic health record (EHR) in developed countries, substantial improvements have been made in the cost and quality of care,6 although the same cannot be said in resource-constrained settings. No conclusive data regarding adoption rates of EHRs in India are available. This lack of data can be attributed to challenges such as long implementation time, security and privacy issues, user resistance to adoption, complex organizational environment, overpopulation, and lack of resources and infrastructure.7, 8, 9
The healthcare system in India is highly dichotomous because of the country's economic disparities. Although some secondary and tertiary care organizations have adopted state-of-the-art healthcare information technology (IT) systems, a vast majority have only basic, legacy information systems in place, if any.10 A majority of healthcare providers in India still use paper-based documentation. Even less information regarding the use of EHRs in a primary care setting is available. Some of the major challenges to implementation of EHRs in primary care in India include the paucity of funds for healthcare IT infrastructure and development, lack of technical standards, and lack of appropriate initiatives from public health governance authorities.11
Earlier attempts to implement EHRs or computerized health information systems in the primary care setting in India have been made. For example, in 1990, a primary care informatics project was initiated in the district of Bhorugram,12 in the state of Rajasthan, India. The objective of this project was to collect information regarding maternal and child health. This project resulted in improvements in maternal and child health outcomes such as increased acceptance of antenatal services and marked improvement in immunization status, among others. However, the current state of this program is not known. An earlier attempt to introduce EHRs in the primary care setting resulted in a system that has been operational in rural India since 1988. This project is the Comprehensive Rural Health Services Project at Ballabgarh in the state of Haryana, run by the All India Institute of Medical Sciences in New Delhi.13 This system has been operational for more than two decades. Its success can be attributed to steady national and international funding.
Similar initiatives in the states of Tamil Nadu14 and Maharashtra15 have received substantial funding from the respective governments of their state and have resulted in successful implementation. For example, the system implemented in the state of Tamil Nadu connects more than 1,589 primary health centers, 267 secondary care hospitals, and 17 medical colleges. However, the system is integrated only across the government-owned facilities. Although these systems are mostly hospital information management systems rather than complete EHRs, they include the basic EHR functionalities that are necessary for current patient care and continuity of care. All these initiatives, however, have been limited to implementation of a computerized medical record and have not attempted to address issues related to data portability and accessibility by healthcare providers and patients themselves.
Pilot projects using smart cards that store patient information have been attempted in countries such as the United States,16 Australia,17 Turkey,18 Taiwan,19 and Sweden.20 Most of these projects found that smart cards were conceptually effective in capturing health data but were not a very efficient tool for portability because of barriers such as lack of infrastructure, low consumer confidence, competing and ever-changing standards, and high operating costs.21
Given these issues, the situation warrants a health record system that is simple enough for adoption by primary care physicians and hospitals. Portability was also necessary because of the multiplicity of healthcare providers and healthcare facilities and for maintaining the patient care continuum. We addressed some of these challenges in a field experiment that was conducted in a rural primary healthcare center in southern India. The aim of this experiment was to evaluate the feasibility of implementing an EHR system and deploying a data portability solution using a USB-based health card and mobile-based Short Messaging Service (SMS) messages. This article presents a descriptive account of the process of design, development, and implementation of a multimodal data portability solution in a rural primary health center in rural India.
Methods
The study was conducted at the Community Health Training Centre (CHTC) of St. John's Medical College in Bangalore, India. The CHTC is situated in a village called Mugalur, approximately 20 miles from the city of Bangalore. This center also serves as the rural outreach center for the medical college. The CHTC provides primary care and has facilities to conduct normal deliveries and minor surgical procedures. It provides basic medical facilities to a population of approximately 25,000 either at no cost or for a nominal fee. This population consists of people living in Mugalur and 35 surrounding villages. Besides a general outpatient clinic, special clinics are conducted on designated days of each month by specialists from the medical college. The special clinics include ophthalmology, otorhinolaryngology, obstetrics, gynecology, pediatrics, oncology, neurology, geriatrics, and psychiatry, among others. The study was conducted over a nine-month period between April and December 2011.
The study participants included patients attending (1) the geriatric clinic and (2) the Maternal and Child Health (MCH) clinic. The participants at the MCH clinic included antenatal and postnatal women. These groups were chosen specifically because of a relatively large pool of patients with regular follow-up. All patients who attended these clinics and who were willing to participate in the study were enrolled. A written informed consent was obtained from all participants prior to enrollment.
Clinic workflows were studied, and interviews were conducted with the physicians and multipurpose health workers as well as with the village chairman and his wife. In rural settings in India, the village chairman, also known as a Sarpanch in parts of northern India, is a representative chosen by the people of the community to represent them publicly. By virtue of the chairman's position, his wife represents the female population of the community. The chairman and his wife, besides being key opinion figures, represent the collective voice of the citizens and influence the behavior of the people in the community. Discussions with them helped in designing a solution that addressed the needs of the village community.
On the basis of these inputs, a solution (named iVaidya) consisting of three components, namely a browser-based EHR, a USB-based memory card (see Figure 1), and an interactive SMS feature, was developed using open-source tools. The EHR was the primary component of patient data input. The application was developed in a way that emulated the health center's workflow. This information was made accessible to the physician through a secure login. The EHR was designed to collect the following information:
Figure 1.
USB-based Memory Card
General information collected from both cohorts
Demography
Socioeconomic details
Literacy status
Problem list
Blood group
Family and social history
History of past hospitalization
History of present illness
Examination
Lab investigations (requested and results)
Medications prescribed
Information specific to the geriatric cohort
Functional status (vision, hearing, mobility, bowel and bladder incontinence)
Activities of daily living
Mental status examination
Information specific to the maternal cohort
Present and past obstetric history
Complete obstetric examination
Risk factors identified
Anthropometry
Immunization status and schedule
Two data entry clerks (DECs) were recruited from the local community and trained on medical terminologies two months prior to the study's initiation. They had studied up to the 10th grade and had reading and writing skills in English and up to three regional languages (Kannada, Telugu, and Tamil). They had also undergone basic computer skills training at a local training center. We chose to hire DECs so as not to interfere with the physicians’ workflow and interaction with patients.
To achieve data portability, an interactive SMS-based system and a USB-based memory card were implemented. All study participants were given access to the SMS functionality by registering a valid mobile number in the EHR. In addition to demographic information, patients could access key health data such as their problem list, recent investigations, and medication list using their mobile phones.
Randomly chosen participants from the two cohorts were additionally issued a USB-based memory card. The USB-based memory card was used to synchronize and store patient details from the EHR database. The card was designed in a way that allowed the contents to be read on any computer that had a Windows operating system.
Workflow
All patients were issued a token number on a first-come, first-served basis and would wait for their turn. While the patients waited, their vital signs would be noted and entered into a notebook that belonged to them. The patient was required to bring this notebook during every visit to have the information updated. The physicians would subsequently document their findings, orders for investigations, and medication prescriptions in this notebook. Prior to the implementation of the system described in this article, the patient's notebook was the only record of the patient's medical information. This notebook, being a physical copy, was susceptible to damage and degradation over time, yet it was the only portability solution for the patients.
The patient was required to hand the notebook to the DECs, who would transcribe its contents into the appropriate sections of the EHR. As a one-time process, the DEC would enter the patient's sociodemographic information and a valid mobile number that belonged to either the patient or anyone from the patient's family. A welcome message would be sent confirming the patient's registration. Upon completion of transcription, the DEC would insert the USB card into the computer and synchronize the information onto it. The card would be issued to the patient. At this point, the DEC would instruct the patient regarding the use of the SMS system and would explain how the card could be used if the patient wished to see a private or government practitioner outside the CHTC. An information sheet in the regional language was also issued to the patient as a reference should the patient wish to use the system at any point. A poster was also put up at the clinic for the patients’ reference.
SMS System
Whenever patients wished to access their information, they were required to type a specific alphabetic code and send the SMS to a toll-free number from their registered mobile number. For example, to access the medications list, the patient would key in the letter d. When the server received this request, it would query the database and send an appropriate response. Depending on the length of the text, the message would be sent as either a single text message or multiple text messages. A list of the codes and the queries they execute is given in Table 1. The number could be updated if the patient decided to change the mobile number.
Table 1.
Association between the Codes and the Response Sent from the Server
| Code | Response |
|---|---|
| A | Demographic details |
| B | Problem list |
| C | Results of last updated tests and investigations |
| D | Last updated pharmacy prescription list |
USB-based Card Solution
In cases where the patient wanted to see a private or government practitioner outside the CHTC, the practitioner could use the card to look up the patient's health data. The card could be used on any Windows-based computer that had a standard USB 2.0 port. An application that would automatically open a browser window displaying basic information about the patient, such as name, age, sex, and blood type, was programmed on the card. Should the physician wish to access detailed information such as present and past history, investigations, and treatment, the patient would have to authorize access by typing in a user ID and password known only to the patient.
Unique to the maternal cohort was the presence of a mother-child link that allowed the details of the child, such as immunization and growth history, to be linked to the mother's record. In effect, this link meant that we did not have to issue another card to the child.
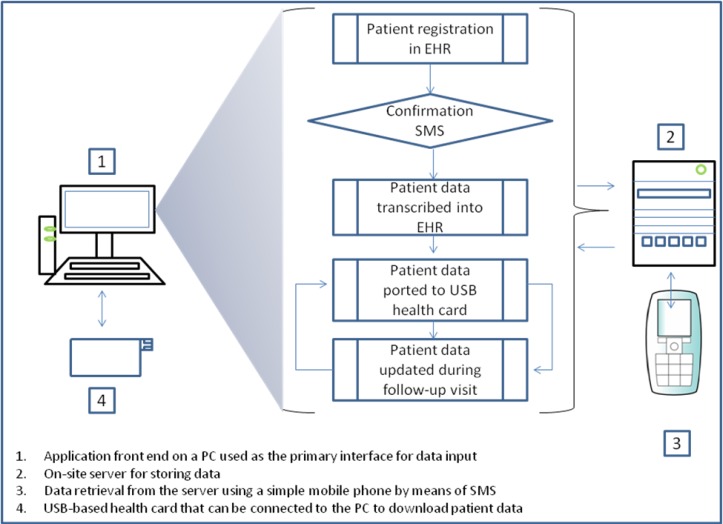
A detailed workflow of the solution can be seen in Figure 2.
Figure 2.
System Workflow
The study was performed on two distinct groups, that is, the geriatric and the maternal cohorts. Each group was further subdivided into two portability subgroups. One group received the USB card and the SMS solution, whereas the other group received only the SMS solution.
On the basis of the availability of the USB cards from a vendor, we sourced 135 such cards and randomly issued them to participants in the geriatric and maternal cohorts. Because of the limited availability of the USB cards, we used a sealed-envelope technique to decide whether a study participant would receive the USB card. Those who did not receive the card were allocated to the SMS-only group.
Results
Data from 308 participants from the study site and surrounding villages were analyzed. Of these participants, 233 participants belonged to the geriatric cohort and 75 belonged to the maternal cohort (see Table 2). The 75 participants in the maternal cohort included only the pregnant women and postnatal mothers. The details of the children of the postnatal mothers were linked to their mother's ID through the mother-child link. Data from 45 such children were collected via the mother-child link. Of the 135 USB cards, 86 were issued to the geriatric cohort and 49 were issued to the maternal cohort. All study participants were given access to the SMS functionality (see Table 3).
Table 2.
Study Participant Characteristics
| Cohort | n | Male | Female | Mean Age in Years |
|---|---|---|---|---|
| Geriatric | 233 | 109 | 124 | 67 (M), 63 (F) |
| Maternal | 75a | 0 | 75 | 24 |
| Total | 308 | 109 | 199 |
Includes only the pregnant women and postnatal mothers. Additional data from 45 children belonging to the postnatal mothers were captured during the course of the study.
Table 3.
Portability Cohort Distribution
| USB Card and SMS | SMS Only | Total | |
|---|---|---|---|
| Geriatric cohort | 86 | 147 | 233 |
| Maternal cohort | 49 | 26 | 75 |
| Total | 135 | 173 | 308 |
The EHR was able to capture, store, and retrieve patient details. The EHR was successful in creating a community-level database that had deep insights into the community's sociodemographic as well as medical profile. For example, analysis of the medical data revealed that 171 study participants (55.5 percent) did not know their blood type. Ninety-seven participants (31.5 percent) reported not to have any allergies, whereas 67 participants (21.75 percent) did not know if they had any allergies.
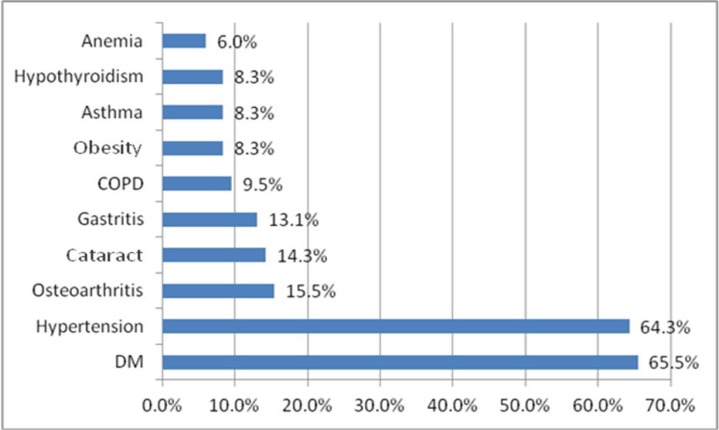
The commonly diagnosed noncommunicable diseases in the geriatric cohort included diabetes mellitus, hypertension, osteoarthritis, cataract, and gastritis, among others (see Figure 3).
Figure 3.
Disease Conditions among the Geriatric Study Population
Abbreviations: COPD, chronic obstructive pulmonary disease; DM, diabetes mellitus.
Within the maternal cohort, the place of delivery was available from 18 participants (24 percent). Ten women underwent deliveries in private hospitals, seven delivered at home, and one delivered in a government hospital (see Table 4). About 51 percent of the deliveries were assisted vaginal delivery or normal vaginal delivery, followed by C-sections (7 percent). The data also revealed that 80 percent of the babies registered in the EHR (n = 45) were breastfed, of which 75 percent received their first feed immediately after birth (see Table 5). Average duration of breastfeeding was 7 months. Besides clinical information, analysis of sociodemographic parameters of the maternal cohort also revealed that only 5 percent (n = 4) were illiterate, while 41 percent (n = 30) had completed high school. From an epidemiological and health resource planning perspective, these data, which were previously difficult to extract from books and ledgers, are now available on demand and can be retrieved with ease.
Table 4.
Place of Delivery (n = 27)
| Place of Delivery | Number of Deliveries |
|---|---|
| Private hospital | 10 |
| Home | 7 |
| Government hospital | 1 |
| Not known | 9 |
Table 5.
Breastfeeding in Newborns
| Time of First Breastfeeding | Number |
|---|---|
| Immediately after birth | 30 |
| Within 48 hours | 3 |
| Later than 48 hours | 3 |
| Bottle fed | 9 |
This information is important from an epidemiological perspective of the local community. It gives insights into the health-seeking behavior and healthcare needs of the community. Until the development and implementation of this solution, access to this information was restricted and time consuming. Such data could be found only in the books and ledgers maintained by the staff at the CHTC. Anyone requesting to see such data usually had to wait until the CHTC staff were free from their responsibilities for the day. Collation of data manually also made data entry errors likely.
Health Card Usage
The compliance of the patients in bringing the health card during every visit was initially poor (< 20 percent). By involving the DECs, healthcare workers, and community leaders in educating the patients regarding the card's usefulness, we achieved almost 100 percent compliance by the third clinic visit. The DECs could update the card with the patient's current health data after each visit. The update was confirmed by opening and visualizing the contents of the card using a web browser.
SMS Usage
There were 83 instances of patients accessing their details through SMS by ten registered users. Of these, five users belonged to the geriatric cohort and five to the maternal cohort. Six female participants and four male participants utilized the SMS service (see Table 6). While seven of these participants were in the group with access to the USB card plus SMS service, only three of these participants were in the SMS-only group (see Table 7).
Table 6.
SMS Service Usage among Male and Female Study Participants
| Female | Male | Total | |
|---|---|---|---|
| Geriatric cohort | 1 | 4 | 5 |
| Maternal cohort | 5 | 0 | 5 |
| Total | 6 | 4 | 10 |
Table 7.
SMS Facility Usage by Portability Group
| USB Card Plus SMS | SMS Only | Total | |
|---|---|---|---|
| Geriatric cohort | 3 | 2 | 5 |
| Maternal cohort | 4 | 1 | 5 |
| Total | 3 | 3 | 10 |
Of the SMS usage, 61 percent was attributed to accessing demographic details, 34 percent was to access health issues, and 5 percent was to access current medication details. No requests for lab results were received. The system logs indicated that all message requests were honored and appropriate responses were delivered to the intended recipients.
Discussion
This pilot study is unique because it explores the use of low-cost, readily available, and easy-to-implement technologies using open-source development tools to address health information storage and portability issues in a resource-constrained setting. Also, the clinic's workflows remained relatively unaffected because training the DECs was easy. Compliance with updating the health card was higher among the participants attending the MCH clinic. This finding could be attributed to the higher level of education of these participants.
However, the biggest challenge was the frequent power interruptions. A 2 kVA uninterrupted power supply (UPS) unit was available to support the computer that hosted the EHR and database for up to 2 hours. However, because of the increased frequency and duration of power cuts especially during the monsoons, the UPS unit began to fail. By the end of the study, it provided only 10 minutes of power. A total of 112 hours of work per DEC were lost as a result of the electricity crisis alone. This problem highlights the challenges in the operations and maintenance of such systems in resource-constrained settings. This problem also has implications for the rates of adoption by end users because of issues related to consistency, reliability, and availability of the information due to the factors mentioned above. However, these problems can easily be addressed by adopting alternative or renewable energy sources.
In our discussions with the healthcare providers, we also found that there seems to be a belief within the local community that the presence of computer hardware between the patient and the doctor during the consultation might adversely affect the patient's faith in the doctor and hence the final outcome of the treatment. This concern can be dispelled by conducting group sessions with the participants to create awareness and explain the benefits of using this technology.
Lastly, the epidemiological data captured thus far is of immense value to community health professionals engaged in patient care–related activities in and around the health center. The data previously captured in paper notebooks were not easily accessible for any further analysis; however, the data now available in an electronic, analyzable format will be subsequently studied and used to improve administration as well as clinical outcomes.
Conclusion
Prior to the pilot study, patients’ medical information was recorded in a notebook that was given back to the patient. The patient had to produce this book during subsequent visits. In many instances, it was difficult to retrieve past medical details because of inconsistent charting during patient visits, illegible handwriting, and degradation of the notebooks due to years of use. With the introduction of the EHR, health card, and SMS service, this issue was completely resolved because standardized templates were available to chart information, most of the content was selection based, and data could be stored perpetually and could also be backed up and retrieved in the event of a disaster. Most importantly, the CHTC now has a complete patient record, which previously did not exist. Also, on the basis of the data from the SMS system, we now know the frequency and nature of information that was requested by the patients. This health data–seeking behavior was previously unknown and can be an area for further studies with regard to mobile health interventions.
On the basis of the pilot study, we believe that such a system can be easily replicated across all healthcare settings. However, the early and successful adoption of such systems depends on a combination of people, technology, and processes.
Study Limitations
The data portability model discussed here is unidirectional in that it only allows visualization of the patient's health data. Any updates to the data had to be performed at the data entry center located within the CHTC. Also, although the mother-child link enabled capture of the child's immunization status and anthropometric data within the mother's card, no mechanism existed to retrieve these data through SMS.
Data portability on the USB cards was 100 percent. However, the usefulness of the health card for accessibility in other care provider settings could not be established because most of the patients did not visit any other healthcare providers for their medical needs.
Other limitations include the availability of the USB-based cards. Because we could only procure 135 such cards, we had to randomly allocate them among the geriatric and maternal cohorts. Finally, having a valid mobile number was a prerequisite for participating in the study. We were therefore unable to explore the possibility of including a portability subgroup who had access to the USB card only.
Scope of Future Studies
This pilot study explored the feasibility of deploying a multimodal strategy to collect health data from the community and make the data accessible at the point of care. As a next step to generate data regarding information portability, we would want the system to capture usage statistics for the USB card, such as the number of times that the card was used and the sections within the patient chart that were accessed by the healthcare provider at the remote location. We would also want the SMS system to be able to retrieve immunization status and anthropometric data of the children through the mobile number used by the mother. Also, to make the USB card truly portable, we would want healthcare providers outside of the CHTC to be able to enter data and store data on this card, which the patient could then bring back to the CHTC to synchronize the data with the rest of the patient's health information.
Acknowledgments
We would like to acknowledge the clinical and nonclinical staff of Mugalur Community Health Training Centre for their support during the requirements gathering, implementation, and participant recruitment phases of the project. We would also like to acknowledge the contributions of Sai Madhukar Sreerama during the manuscript preparation process.
Contributor Information
Kedar Radhakrishna, Kedar Radhakrishna, MBBS, MPhil, is a senior resident at St. John's Research Institute in Bangalore, India..
B. Ramakrishna Goud, B. Ramakrishna Goud, MBBS, MD, is an additional professor at St. John's Medical College in Bangalore, India..
Arvind Kasthuri, Arvind Kasthuri, MBBS, MD, is a professor at St. John's Medical College in Bangalore, India..
Abijeet Waghmare, Abijeet Waghmare, MBBS, is a research associate at St. John's Research Institute in Bangalore, India..
Tony Raj, Tony Raj, MBBS, MD, is head of the Medical Informatics Division of St. John's Research Institute in Bangalore, India..
Notes
- 1.Yadav K., Jarhyan P., Gupta V., Pandav C. S. Revitalizing Rural Health Care Delivery: Can Rural Health Practitioners Be the Answer? Indian Journal of Community Medicine. 2009;34(1):3–5. doi: 10.4103/0970-0218.45368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Census of India. Status of Literacy. 2011. Available at http://censusmp.nic.in/censusmp/All-PDF/6Literacy21.12.pdf (accessed December 26, 2013).
- 3.Telecom Regulatory Authority of India. Telecom Sector in India: A Decadal Profile. 2012. Available at http://www.trai.gov.in/WriteReadData/Publication/Document/201304121052403536675NCAER–Report08june12.pdf (accessed December 26, 2013).
- 4.Government of India, Ministry of Health and Family Welfare, Press Information Bureau. India Is the Second-Largest Mobile Phone User in World. 2011. Available at http://pib.nic.in/newsite/erelease.aspx?relid=85669 (accessed December 23, 2013).
- 5.IMS Institute for Health Informatics. Understanding Healthcare Access in India: What Is the Current State? 2013. Available at http://www.imshealth.com/deployedfiles/imshealth/Global/Content/Corporate/IMS%20Institute/India/Understanding_Healthcare_Access_in_India.pdf (accessed December 26, 2013).
- 6.Walker J., Pan E., Johnston D., Adler-Milstein J., Bates D. W., Middleton B. The Value of Health Care Information Exchange and Interoperability. Health Affairs. 2005. pp. W5-10–W5-18. [DOI] [PubMed]
- 7.Scholl J., Syed-Abdul S., Ahmed L. A. A Case Study of an EMR System at a Large Hospital in India: Challenges and Strategies for Successful Adoption. Journal of Biomedical Informatics. 2011;44(6):958–67. doi: 10.1016/j.jbi.2011.07.008. [DOI] [PubMed] [Google Scholar]
- 8.Sood S. P., Nwabueze S. N., Mbarika V. W. A., Prakash N., Chatterjee S., Ray P., Mishra S. Electronic Medical Records: A Review Comparing the Challenges in Developed and Developing Countries. Proceedings of the 41st Hawaii International Conference on System Sciences. 2008. pp. 1–10.
- 9.Mane R. R., Kulkarni R. V. A Review: Electronic Medical Records (EMR) System for Clinical Data Storage at Health Centers. International Journal of Computer Technology and Applications. 2012;3(5):1837–42. [Google Scholar]
- 10.Ovum. Healthcare IT Adoption in India. September 18, 2012. Available at http://ovum.com/research/healthcare-it-adoption-in-india/ (accessed September 28, 2013).
- 11.Athavale A. V., Zodpey S. P. Public Health Informatics in India: The Potential and the Challenges. Indian Journal of Public Health. 2010;54(3):131–36. doi: 10.4103/0019-557X.75735. [DOI] [PubMed] [Google Scholar]
- 12.Singh A. K., Kohli M., Trell E., Wigertz O., Kohli S. Bhorugram (India): Revisited. A 4 Year Follow-up of a Computer-based Information System for Distributed MCH Services. International Journal of Medical Informatics. 1997;44(2):117–25. doi: 10.1016/S1386-5056(96)01251-8. [DOI] [PubMed] [Google Scholar]
- 13.Krishnan A., Nongkynrih B., Yadav K., Singh S., Gupta V. Evaluation of Computerized Health Management Information System for Primary Health Care in Rural India. BMC Health Services Research. 2010;10:310. doi: 10.1186/1472-6963-10-310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Natarajan S., Panchanathan V., Bansal P. K. Health Management Information System Implemented in Government Hospitals of Tamil Nadu. International Journal of Scientific and Engineering Research. 2013;4(10):282–88. [Google Scholar]
- 15.eMaharashtra. Healthcare & Academics Management & Information System. 2013. Available at http://emaharashtra.eletsonline.com/2013/healthcare-academics-management-information-system-hereinafter-referred-to-as-the-hmis-to-draw-it-enabled-services-for-the-operations-of-14-government-medical-colleges-and-19-t-3/ (accessed December 27, 2013).
- 16.Vijayan J. N.Y. Hospitals, Siemens Launch Smart-Card Pilot. Computerworld. 2005. December 12, Available at http://www.computerworld.com/s/article/106950/N.Y._Hospitals_Siemens_Launch_Smart_Card_Pilot (accessed May 26, 2014).
- 17.Morris S., Cooper J., Bomba D., Brankovic L., Miller M., Pacheco F. Australian Healthcare: A Smart Card for a Clever Country. International Journal of Biomedical Computing. 1995;40(2):101–5. doi: 10.1016/0020-7101(95)01132-x. [DOI] [PubMed] [Google Scholar]
- 18.Kardas G., Tunali E. T. Design and Implementation of a Smart Card Based Healthcare Information System. Computer Methods and Programs in Biomedicine. 2006;28(1):66–78. doi: 10.1016/j.cmpb.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 19.Liu C. T., Yang P. T., Yeh Y. T., Wang B. L. The Impacts of Smart Cards on Hospital Information Systems—an Investigation of the First Phase of the National Health Insurance Smart Card Project in Taiwan. International Journal of Medical Informatics. 2006;75(2):173–81. doi: 10.1016/j.ijmedinf.2005.07.022. [DOI] [PubMed] [Google Scholar]
- 20.Klein G. O. Smart Cards—a Security Tool for Health Information Systems. International Journal of Bio-medical Computing. 1994;35(suppl.):147–51. [PubMed] [Google Scholar]
- 21.Ward S. R. Health Smart Cards: Merging Technology and Medical Information. Medical Reference Services Quarterly. 2003;22(1):57–65. doi: 10.1300/J115v22n01_06. [DOI] [PubMed] [Google Scholar]