Abstract
The incidence of clinical fat embolism syndrome (FES) is low (<1%) whilst fat embolism (FE) of marrow fat appears to occur more often (Mellor and Soni (2001)). Paradoxical brain FE may occur in patients undergoing hip orthopedic surgery who have an undocumented patent foramen ovale (PFO). We report a case of an eighty-year-old male patient, who underwent a scheduled revision hip surgery suffering a paradoxical cerebral FE.
1. Introduction
Fat embolism (FE) is defined as the presence of fat within the circulatory system, with or without clinical impact [1]. This entity may occur following long bone fractures, intramedullary nailing, and arthroplasty and may lead to coma or death [2–4]. Fat emboli might pass into the systemic circulation in the presence of venous to arterial (v-a) circulation shunt, a patent foramen ovale (PFO) being the most common cause [5].
Fat embolism syndrome (FES) is characterized by a set of respiratory, neurological, cutaneous, and hematological symptoms that may establish gradually or suddenly [6].
We report a case of a patient who sustained a paradoxical cerebral FE during revision hip surgery.
2. Case Report
An eighty-year-old male patient with multiple comorbidities (hypertension, dyslipidemia, hypothyroidism, myocardial reperfusion surgery 20 years ago, and type 2 second-degree AV block) underwent a scheduled revision hip surgery due to aseptic acetabular loosening.
Surgery was performed, under hypotensive epidural anesthesia, in lateral decubitus position using a posterolateral approach. Acetabular component was revised with a trabecular metal cup while the femoral component was done with a cement-cement technique. There were no abnormal intraoperative findings, particularly no decrease of oxygen saturation, no circulatory instability, normal heart rate, and no drop in arterial blood pressure (measured by noninvasive blood pressure).
Having completed the surgical procedure, the patient was transferred to the anesthesia recovery room, where fifteen minutes after arrival evolved stuporous with sensory impairment associated with left faciobrachiocrural hemiplegia. Immediately, tracheal intubation, mechanical respiratory assistance, and hemodynamic stabilization were established.
Within the first hour, a head computed angiotomography scan was conducted. This study showed a hypointense image, with the same intensity as fat tissue, at the middle cerebral artery (MCA) birth consistent with FE (Figure 1). With presumptive diagnosis of FE and being in 6-hour window from the time of the incision, we decided to perform an intra-arterial mechanical thrombolysis.
Figure 1.
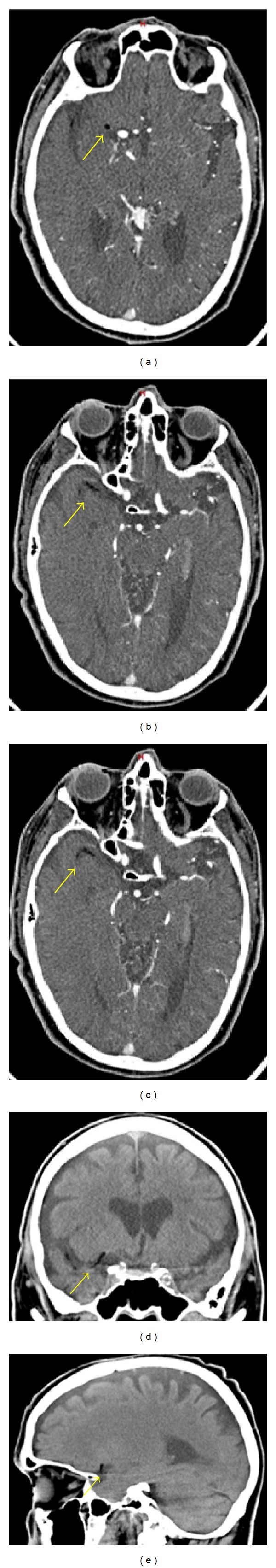
Computed tomography: axial ((a), (b), and (c)), coronal (d), and sagittal section images (e). Hypointense image is observed at the birth of the MCA (yellow arrow).
We proceeded to perform a digital angiography that showed an amputation of MCA prior to its bifurcation (Figures 2(a) and 2(c)). The artery occlusion was recanalized with a microcatheter, through which thrombectomy was done with a Solitaire AB stent (Covidien, USA), retrieving material that was sent for pathological examination (Figure 3(a)). After this procedure, coplete reperfusion of the MCA and its branches was obtained, achivieng a Grade 3 Thrombolysis in cerebral infarcion score (TICI score). Then the patient was transferred to the adult intensive care unit.
Figure 2.
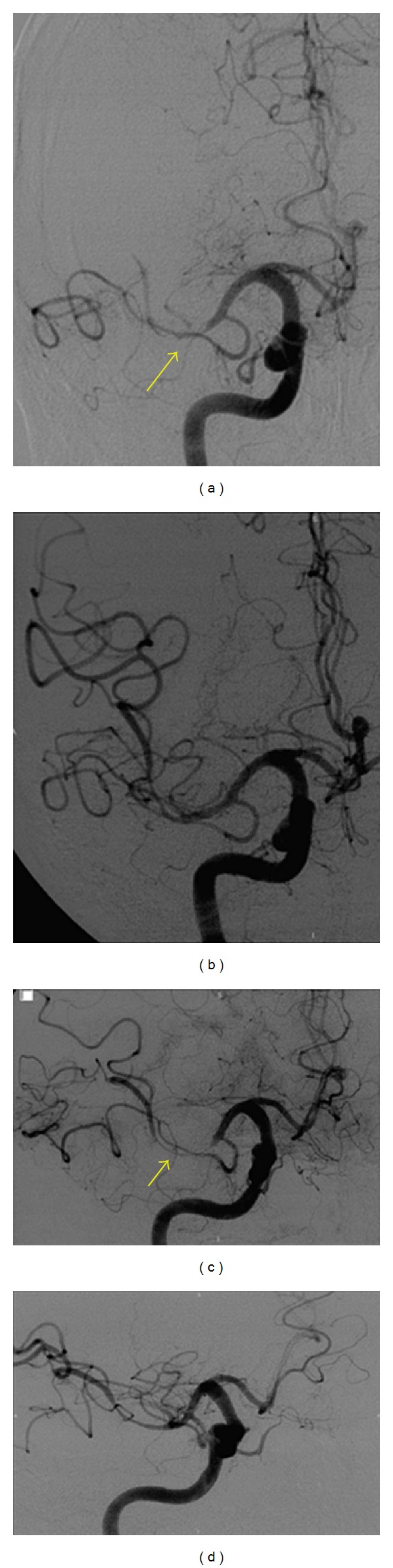
Initial Angiography: anteroposterior view (a) and lateral view (c) evidence complete occlusion of MCA (arrow). Angiography after thrombectomy: anteroposterior view (b) and lateral view (d) show permeable MCA.
Figure 3.
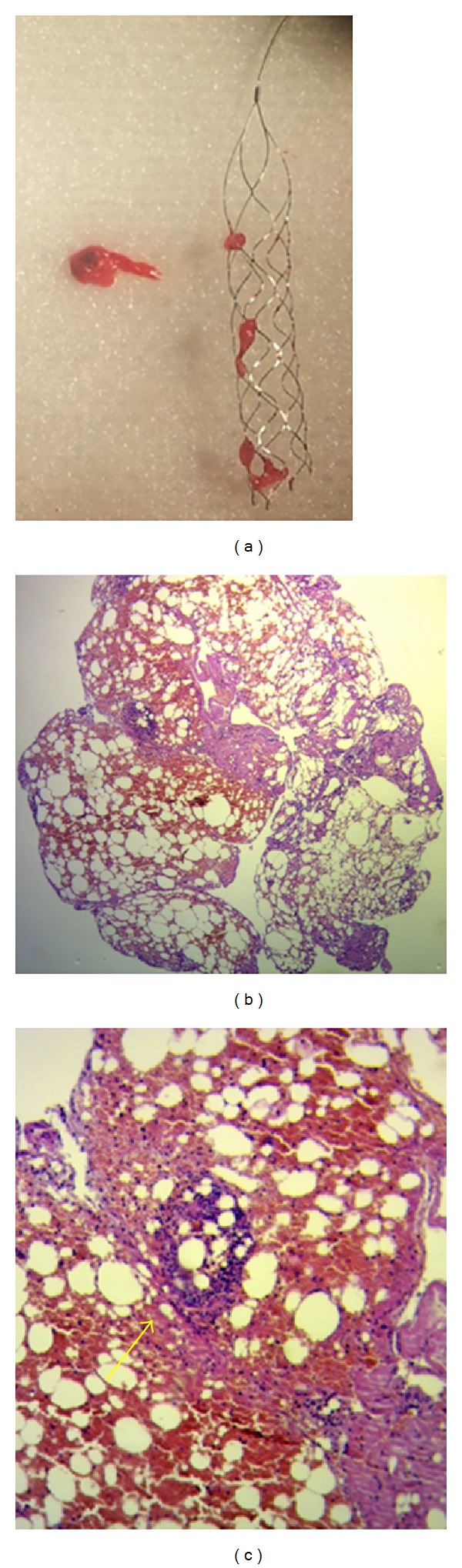
A macroscopic photograph of the fat emboli (a). Histological simple photograph with hematoxylin and eosin at 4x (b) and 10x (c) where an adipose fragment of bone morrow interspersed with fibrin is seen. In addition image (c) shows a bone marrow lymphoid accumulation (arrow).
Five hours after being admitted to the AICU an episode of bradycardia and hypotension led to a new CT scan which visualized a frontotemporal bleeding hematoma with midline deviation. Additionally, a transcranial Doppler revealed bilateral symmetrical blood flow in the MCA. In this situation it was decided to maintain close monitoring and careful observation.
When color Doppler transesophageal echocardiography was done, color flow and bubbles passage with Valsalva maneuver evidenced PFO.
Throughout the patient postoperative course, conservative treatment was pursued trying to diminish poststroke effects. Four weeks after surgery, the patient was discharged with remaining hemiparesis, dysarthria, and cognitive problems and deceased 3 months later.
3. Discussion
The incidence of FES is low (<1%) while FE presents more often [4]. Paradoxical brain FE may occur in patients undergoing hip orthopedic surgery who have an undocumented PFO [5]. Although it has been widely reported, to our knowledge this is the first case report of paradoxical cerebral FE during revision hip surgery.
During hip replacement, acetabular and femur bone preparation, and especially intramedullary instrumentation, cause bone marrow extravasation [7, 8]. Usually fat emboli do not reach systemic circulation as they are retained and filtered in the pulmonary circulation, causing in some cases hypotension, hypoxemia, acute respiratory distress, confusion, coma, or even death [9–11]. Paradoxical embolism occurs when an emboli passes from the pulmonary circulation to the systemic circulation by either a PFO or pulmonary capillaries [9–12].
In a trial done in 1000 consecutive patients with contrast transesophageal echocardiography, the incidence of PFO was 9.2%, and in the decade between 70 and 79 years the incidence was 6.15% [13]. In another trail done by autopsy of 956 normal hearts, a 27.3% incidence of PFO was found, decreasing progressively with increasing age from 34.3% during the first three decades of life to 25.4% during the fourth to eighth decade. In 98% of cases the FOP had 1 to 10 mm diameter with a tendency to increase the size with increasing age, from average of 3.4 mm in the first decade to 5.8 mm in the tenth decade of life [14]. In our patient, the finding of PFO may explain the presence of paradoxical embolism, particularly in the absence of lung involvement.
Riding et al. [12] have detected intraoperative cerebral emboli, with transoesophageal echocardiography, in 18 of 34 (53%) patients with v-a shunt, whereas in patients without shunt they did not detect any episodes of FE. Although FE was not documented intraoperatively by means of transesophageal or transthoracic echocardiography, paradoxical cerebral embolism had to be suspected, when neurologic symptoms were detected, on the basis of the close temporal association between medullary manipulation and the occurrence of symptoms. There are no firm conclusions about the role of Doppler ultrasound to detect embolism during orthopedic surgery [15].
A CT scan was performed immediately because of rapid access, detecting a well-defined hypointense image at birth of the MCA. When cerebral FE is suspected, CT scan and clinical symptoms are not always diagnostic, while MRI is a more sensitive imaging modality and should be performed instead if possible [16]. The use of MRI should be the first step in the diagnostic algorithm to rule out cerebral FE, as it is more sensitive and consistently shows multiple small, scattered lesions that could be negative with other methods [17].
Spinal anesthesia could increase the risk of right-left shunt by altering the circulation volume and arterial and venous pressure due to spasm and in contrast with general anesthesia, by allowing coughs that increase local pressure [18]. In our case an additional risk could have been the left lateral decubitus position, promoting the FE passage through PFO [8].
While PFO can be documented in adults with transthoracic echocardiogram or even better with a transesophageal echocardiography, surgical treatment or closure by catheterization of a PFO should not be considered preoperatively to arthroplasty because of the rare presentation of cerebral embolism [18].
In immediate postoperative orthopedic surgery, while hypotension, tachycardia, or stupor often results from hypovolemic, anemia, or residual sympathetic blockade, it is necessary to consider the possibility of a FE [2]. Close monitoring of the patient is essential during surgery and in the immediate postoperative care. Although neurologic symptoms of cerebral FE are usually transient and entirely reversible, the condition is usually misdiagnosed and fatal if the treatment is delayed. Paradoxical cerebral embolism following revision hip arthroplasty is rare but potentially catastrophic. Early diagnosis requires high index of suspicion and prevents morbidity and mortality with optimal support and immediate treatment.
Consent
Each author certifies that his or her institution approved the reporting of this case report and that all investigations were conducted in conformity with ethical principles of research and that informed consent for participation in the study was obtained.
Conflict of Interests
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, and patent/licensing arrangements, etc.) that might pose a conflict of interests in connection with the submitted paper.
References
- 1.Apostolou CD, Skourtas CE, Tsifetakis SD, Papagelopoulos PJ. Fat embolism after uncemented total hip arthroplasty. Clinical Orthopaedics and Related Research. 2002;(398):153–156. doi: 10.1097/00003086-200205000-00022. [DOI] [PubMed] [Google Scholar]
- 2.Sarmiento Penide A, Rodriguez Velasco A, Lopez Pérez M, Molins Gauna N, Rey Rilo T. Síndrome de embolia grasa tras recambio de vástago femoral de prótesis de cadera. Revista Española de Anestesiología y Reanimación. 2004;51:276–280. [PubMed] [Google Scholar]
- 3.Herndon JH, Bechtol CO, Crickenberger DP. Fat embolism during total hip replacement. A prospective study. Journal of Bone and Joint Surgery. American. 1974;56(7):1350–1362. [PubMed] [Google Scholar]
- 4.Mellor A, Soni N. Fat embolism. Anaesthesia. 2001;56(2):145–154. doi: 10.1046/j.1365-2044.2001.01724.x. [DOI] [PubMed] [Google Scholar]
- 5.Pell AC, Hughes D, Keating J, Christie J, Busuttil A, Sutherland GR. Brief report: fulminating fat embolism syndrome caused by paradoxical embolism through a patent foramen ovale. The New England Journal of Medicine. 1993;329(13):926–929. doi: 10.1056/NEJM199309233291305. [DOI] [PubMed] [Google Scholar]
- 6.Gurd AR. Fat embolism: an aid to diagnosis. Journal of Bone and Joint Surgery B. 1970;52(4):732–737. [PubMed] [Google Scholar]
- 7.Edmonds CR, Barbut D, Hager D, Sharrock NE. Intraoperative cerebral arterial embolization during total hip arthroplasty. Anesthesiology. 2000;93(2):315–318. doi: 10.1097/00000542-200008000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Thienpont E, Kaddar S, Morrison S. Paradoxical fat embolism after imcemented total hip arthroplasty: a case report. Acta Orthopaedica Belgica. 2007;73(3):418–420. [PubMed] [Google Scholar]
- 9.Dive AM, Dubois PE, Ide C, Bulpa PA, Broka SM, Installé E. Paradoxical cerebral fat embolism: an unusual cause of persistent unconsciousness after orthopedic surgery. Anesthesiology. 2002;96(4):1029–1031. doi: 10.1097/00000542-200204000-00037. [DOI] [PubMed] [Google Scholar]
- 10.Gelinas JJ, Cherry R, MacDonald SJ. Fat embolism syndrome after cementless total hip arthroplasty. Journal of Arthroplasty. 2000;15(6):809–813. doi: 10.1054/arth.2000.6631. [DOI] [PubMed] [Google Scholar]
- 11.Koessler MJ, Fabiani R, Hamer H, Pitto RP. The clinical relevance of embolic events detected by transesophageal echocardiography during cemented total hip arthroplasty: a randomized clinical trial. Anesthesia and Analgesia. 2001;92(1):49–55. doi: 10.1097/00000539-200101000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Riding G, Dally K, Hutchinson S, Rao S, Lovell M, McCollum C. Paradoxical cerebral embolisation. An explanation for fat embolism syndrome. Journal of Bone and Joint Surgery. British. 2004;86(1):95–98. [PubMed] [Google Scholar]
- 13.Fisher DC, Fisher EA, Budd JH, Rosen SE, Goldman ME. The incidence of patent foramen ovale in 1,000 consecutive patients: a contrast transesophageal echocardiography study. Chest. 1995;107(6):1504–1509. doi: 10.1378/chest.107.6.1504. [DOI] [PubMed] [Google Scholar]
- 14.Hagen PT, Scholz DG, Edwards WD. Incidence and size of patent foramen ovale during the first 10 decades of life: an autopsy study of 965 normal hearts. Mayo Clinic Proceedings. 1984;59(1):17–20. doi: 10.1016/s0025-6196(12)60336-x. [DOI] [PubMed] [Google Scholar]
- 15.Silbert BS, Evered LA, Scott DA, Rahardja S, Gerraty RP. Review of transcranial doppler ultrasound to detect microemboli during orthopedic surgery. AJNR. American Journal of Neuroradiology. 2013:1–6. doi: 10.3174/ajnr.A3688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gregorakos L, Sakayianni K, Hroni D, et al. Prolonged coma due to cerebral fat embolism: report of two cases. Journal of Accident and Emergency Medicine. 2000;17(2):144–146. doi: 10.1136/emj.17.2.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Parizel PM, Demey HE, Veeckmans G, et al. Early diagnosis of cerebral fat embolism syndrome by diffusion-weighted MRI (starfield pattern) Stroke. 2001;32(12):2942–2944. [PubMed] [Google Scholar]
- 18.Meier B, Lock JE. Contemporary management of patent foramen ovale. Circulation. 2003;107(1):5–9. doi: 10.1161/01.cir.0000046073.34261.c1. [DOI] [PubMed] [Google Scholar]


