Summary
This review discusses various aspects of social disadvantage and their association with poor asthma control, including socioeconomic status, exposure to psychosocial stress and violence, minority affiliation, environmental concerns such as allergens and pollution, and poverty in rural settings. Each of these elements has been linked with worsened asthma outcomes in children. Known and hypothesized mechanisms behind these associations are described in an effort to further understand the complex entity of poorly controlled asthma among socially deprived children. Intervention studies to improve asthma outcomes in these vulnerable populations are also described.
Keywords: Asthma, Ethnic Groups, Paediatrics, Social Class, Socioeconomic Factors, Stress, Psychological
Introduction
Social disadvantage is defined as being subjected to racial or ethnic prejudice or discrimination because of identification as a member of a group, while neglecting the person’s qualities as an individual.1 In the medical literature this description has been expanded to include other social inequalities among the population associated with health disparities, such as socioeconomic status (SES).2 Poor asthma control includes asthma symptoms, activity limitations, rescue medication use, missed school or work, exacerbations requiring systemic corticosteroids and health care utilization. In this review, we will dissect social disadvantage into its individual elements and explore their relationships with asthma control in children (see Box 1). Additionally, we will describe interventions that have been designed to improve asthma morbidity in this vulnerable population.
Socioeconomic Status and Asthma Control
SES defines the complex relationship of the individual or group within the hierarchy of society. While SES is not a single finite entity, the measurement of a child’s SES can be approximated by consideration of household income, caregiver employment or education status, living conditions, or habitation in geographic locations with a predominantly poor population.2 These variables have each been linked with childhood asthma control.
On a global scale, ecological data suggest that while wheezing is more prevalent in children from high-income countries, severe symptoms among current-wheezers are more prevalent in less affluent countries.3 In the United States (US), studies have shown clearly that asthmatic children living in impoverished areas and the inner-city have higher rates of emergency department (ED) visits and hospitalizations for asthma.4, 5 Proposed explanations for this phenomenon have included poor access to primary care and maintenance medications6 due to lack of private insurance or disruptions in coverage.7 However, even in Canada and the United Kingdom (UK), where universal healthcare coverage virtually eliminates financial barriers to healthcare access, there are higher hospitalization rates and ED visits among children from low SES backgrounds.8, 9 This suggests that ability to pay for healthcare and medications is not the principal explanation for worsened asthma morbidity among children from lower-income households. The presence of this effect in communities with guaranteed access to healthcare may imply that greater weight is attributable to the impoverished environment and the ability of the family to address the healthcare needs of the child.
Interestingly, caregiver perception of the financial situation at home may play an important role in determining the child’s asthma morbidity. One study demonstrated that among children whose parents perceived financial burden in managing their asthma, there were increased odds of ED visits, hospitalizations, and missed school due to asthma in the prior year. This increase in exacerbations and absenteeism was independent of disease severity, access to healthcare, and the actual financial status of the family.10 This highlights a key role for parental perception of the social situation and indicates that there is likely a complex interplay between the actual financial climate in the home and the perceived threat of that climate, which is ultimately influencing health outcomes among asthmatic children.
Educational status of the caregiver has been shown to be a risk factor for asthma exacerbations. A study segregating communities by zipcodes in impoverished regions demonstrated that those who live in zip codes with the lowest adult educational attainment rates are more likely to visit the ED or be admitted for asthma.4 Adult education may be a true risk factor for poor management of childhood asthma, perhaps through lack of understanding of the disease and its treatments or easily manoeuvring through the medical system. However, it is difficult to disentangle the effect from the potential association with lower level of employment, financial instability and healthcare access, each of which may independently lead to increased asthma morbidity.
Environmental exposures specific to social disadvantage are discussed below. However, while exposure to environmental tobacco smoke (ETS) pervades many parts of society, there is a disproportionately high exposure rate among low-income youth. 11 In the National Cooperative Inner-City Asthma Study (NCICAS), 59% of families included at least one smoker, 39% of caretakers reported that they smoked, and 48% of the asthmatic children had significant tobacco smoke exposure in the previous 24 hours, as measured by urinary cotinine/creatinine ratio.12
Other risk factors for poor asthma control related to SES that have been identified include household crowding and health status of the caregiver.
Psychosocial Stress, Exposure to Violence, and Asthma Control
Psychosocial stress among children with asthma and/or their caregivers is linked to asthma morbidity.13 It is conceivable that social disadvantage itself represents a group of stressors which influence this relationship. Parental panic, fear, sense of being alone, and lack of confidence in the general practitioner were shown to be major determinants of use of emergency services for asthmatic children in London.9 Children with asthma, themselves, who experience an acute negative life event are at increased risk for a subsequent asthma attack, and the risk is increased among those children with chronic stress.14
Exposure to violence is pervasive in inner-city children15 and has been linked to asthma morbidity.16. Caregiver report of violence and perception of unsafe neighbourhoods have been associated with increased asthma symptoms in inner-city children.17, 18 Across cultures, children who report being victimized or feeling unsafe have higher odds of having an asthma episode, medication and healthcare use.19, 20 The healthcare use tends to be weighted towards emergency services, despite reportedly good access to the primary physician’s office.21
The reasons for worsened asthma morbidity among children exposed to stressful or violent environments are not fully understood. One prevailing theory is that stress affects the inflammatory response. Young children exposed to higher degrees of caregiver stress during infancy have heightened IgE expression, allergen-specific proliferative responses, and inflammatory markers.22 Clinical evidence for the relationship to inflammation was demonstrated by Chen and colleagues as they reported an increase in exhaled nitric oxide in asthmatic subjects after an acutely stressful event compared to prior – an effect that was not seen in healthy children - and the effect was augmented in children of low SES.23 Biologic mechanisms relating poverty, inflammation and psychosocial stress have demonstrated increased allergic inflammatory markers and overexpression of inflammatory genes in children from low SES backgrounds. This suggests that, while stress itself affects asthma morbidity through effects on airway inflammation, socially disadvantaged children are particularly susceptible.
Other proposed hypotheses to explain the link between stress and asthma morbidity in children include increased susceptibility to viral infections,14 lower cortisol levels which lead to loss of the inhibitory response to inflammation,24 and effects of stress on the hypothalamic-pituitary-adrenal axis and the sympathetic-adrenal-medullary axis.25
Minority Affiliations and Asthma Control
Asthma severity is worse among particular racial and ethnic groups. For instance, in the US, African Americans and Puerto Ricans have higher rates of exacerbations and ED visits for asthma.26 In the UK, Black African and Black Caribbean inner-city asthmatic children are also more likely to visit the ED compared with White children.9 It has been hypothesized that since ethnicity and SES are related and low SES is associated with worsened asthma outcomes, that SES may explain ethnic health disparities in minority populations. However, in reality, the reasons for worsened asthma outcomes among ethnic minorities are complex, incompletely understood, and likely multifactorial.
Lack of adequate insurance has been proposed as a possible explanation; among children who visited the ED or were admitted for asthma in a single U.S. county, Black children were over twice as likely and Hispanic children were over 5 times as likely to be without private insurance compared to Non-Hispanic White children.4 However, in universal healthcare systems such as the UK, similar disparities exist, with South Asian and Black patients having higher risk of admission.27
Though there are many potential confounding influences to racial disparity, like type of insurance, family history of asthma, and healthcare access, carefully designed studies indicate that these do not adequately explain health disparities in minority children with asthma.28 However, caregiver attitudes and behaviours toward healthcare and less use of asthma medications may vary among disadvantaged populations.29
In addition to the factors outlined above, exposure to allergens or pollutants may be at least partially responsible for worsened asthma outcomes among minority children. Hispanic and Black households are associated with higher levels of cockroach allergens as compared with White households.30, 31 The NCICAS also found that African American children have greater odds of cockroach, dust mite, and Alternaria alternata sensitivity, and Mexican American children have increased odds of cockroach and dust mite sensitivity compared to White children.32 Other suggested explanations for worsened asthma control among ethnic minorities include higher rates of obesity, stress exposure, and depression/anxiety in these populations.33 Finally, since disparities in asthma prevalence and severity have not been fully clarified by financial, social, and environmental issues, genetic predisposition has also been investigated.34, 35 Genetic admixture plays an important role in the interaction of race, ethnicity and asthma outcomes at different levels of SES.36–38 The multiplicity of these factors are currently being evaluated in the NHLBI AsthmaNet protocol focused on best response to therapeutics in African American children and adults with asthma (clinicaltrials.gov NCT01967173).
Environmental Risk Factors and Asthma Control
The role of environmental exposures in childhood asthma development and morbidity is indisputable. Many socially disadvantaged populations inhabit low socioeconomic housing developments and cluster in urban environments. The indoor environment may be a source for high concentrations of allergen and non-allergen exposures that exacerbate respiratory symptoms in children with asthma. Similarly, ambient air pollution in industrial or high traffic density areas may contribute to poor asthma control.
Allergens
While house dust mite is the most common allergen sensitization in children with asthma and has a clear relationship with loss of control,39 cockroach and mouse allergen have emerged as particular problems in the inner-city. Factors that increase cockroach and mouse infestation include low SES, building degradation and high population density.40 Both allergens are found in house dust particles and are particularly high in kitchens, though they are also found in bedrooms.
As with the other allergens, studies have shown that increased cockroach exposure leads to sensitization. The NCICAS studied children with asthma from 8 US inner-city environments to determine the relationship between environmental exposure, sensitization and asthma morbidity. In a subset of 500 children, cockroach allergen was present in 85% of bedrooms. Allergy testing showed that one third of children were allergic to cockroach and that exposure was significantly related to sensitization.41 Furthermore, children who were sensitized and exposed to high levels of cockroach antigen had significantly higher rates of hospitalization, medical visits, days of wheezing, missed school and lost sleep compared to other indoor allergens.42 These findings were confirmed in the subsequent ICAS consortium which demonstrated even higher sensitization rates, up to 80%, in children with moderate persistent asthma.43 Mouse allergen is also highly prevalent in inner-city homes, particularly multifamily homes with physical damage. Phipatanakul et al reported that 95% of all homes in a subset of 499 subjects from the NCICAS had detectable levels of mouse allergen in at least one room with the highest levels found in the kitchen.44
High levels of mouse allergen in the home can lead to sensitization.44 Increased exposure in sensitized children is a risk factor for asthma morbidity. Matsui et al. found that in mouse sensitized preschool children from inner-city Baltimore, exposure to high levels of home mouse allergen increased the likelihood of unscheduled physician visits, ED visits and hospitalizations and increased asthma symptom days and medication use.45 More recent studies have shown mouse to be more important to inner-city asthma morbidity than cockroach in some areas.46 As children spend a large portion of time in the school environment, inner-city schools have emerged as a source of significant exposure to allergens,47 mould,48 and endotoxin,49 which may all contribute to asthma outcomes.
Air pollution
Both ambient (outdoor) and indoor air pollution contribute to respiratory health effects in children with asthma. Ambient pollutants tend to be concentrated in urban or industrial environments, putting low income housing and inner-city inhabitants at highest risk. Indoor pollutants emanate from combustion for home heating, cooking, tobacco smoke and other activities. The adverse health effects are not necessarily linked to inner-city children and are prevalent in homes with poor ventilation or use of unclean biomass fuels that may affect disadvantaged populations in a variety of settings. Additionally, children may be at high risk of exposure to these pollutants as they can spend as much as 90% of their time indoors50 and indoor behaviours can lead to doubling the respirable levels by resuspending particles.51 While numerous specific particulate and gaseous materials may contribute to the health effects, relatively few have been well studied.
Nitrogen dioxide (NO2) is a gaseous pollutant emitted from outdoor and indoor combustion such as motor vehicle use, gas stoves, heaters and furnaces. Inner-city homes may have high levels of NO2 associated with ambient pollution or indoor sources, such as poorly ventilated gas stoves 52 or other home characteristics.53
In children with asthma, exposure to NO2 worsens asthma symptoms and lung function.54 It also has a synergistic effect with allergen exposures to elicit airway inflammation and symptoms in allergen-sensitized individuals.55
Particulate air pollution (particulate matter, PM) is found in traffic-related and industrial combustion, as well as indoor sources such as cooking exhaust and environmental tobacco smoke.51, 56 Fine particles (PM2.5) ≤ 2.5μm are primarily produced by industrial or motor vehicle combustion and are able to enter the respiratory tract and deposit in the alveoli.57 Coarse particles, PM2.5 – 10, more frequently settle in dust and soil and because of their particle size are primarily deposited in the proximal airways57.
Both coarse and fine particles affect respiratory symptoms in children with asthma.58, 59 The majority of studies have focused on home indoor or ambient exposures. Data from the ICAS demonstrated that particulate matter from outdoor pollution is highly prevalent in urban homes 56 and that elevated levels of ambient PM is associated with asthma symptoms, lower lung function and missed school days.54 Other home-based studies corroborate these findings with personal exposure measurements.60–62
Rural environments and asthma control
There are less published data concerning asthma outcomes in children from low-income families living in rural environments compared with urban inner-city environments.63 However, rural patients with asthma may have worsened asthma morbidity compared to urban patients.64 In children from impoverished rural counties in the Arkansas’ Delta region, 43% had an unscheduled acute care visit in the last 3 months, 28% had at least 1 ED visit for asthma in the last 6 months, and the majority met criteria for poorly controlled asthma.63 The authors of this study postulated that caregiver characteristics, poor access to healthcare due to distance and lack of transportation, scarcity of paediatric subspecialty care, shortage of community resources, and allergen exposure and sensitization are possibly responsible for poor asthma control in the rural population.
Environmental exposures in rural, particularly farming, environments have been noted to decrease the risk of developing asthma, but little is known about asthma control in these communities.
Worldwide, poor rural communities may be at higher risk of asthma morbidity due to poor indoor ventilation and the burning of unrefined fuels. Rural environments may be relatively devoid of traffic and industry related pollution, however, exposure to woodsmoke in Guatemala 65 and biomass in India 66 have been shown to significantly affect respiratory health in these environments.
Interventions to improve asthma control among socially disadvantaged children
Interventions to address the modifiable factors leading to poor asthma control in socially disadvantaged communities have had mixed results. Examples include asthma education and self-management taught through trained community health workers (CHW), environmental control in the home, culture-specific programs, technology-based interventions that target adolescents, school-based programs, or some combination of these.67
Successful community-based intervention programs have generally used strategies such as home visits by CHW, provision of asthma education, stress reduction strategies, environmental remediation within the home, and frequent follow-up. Table 1 summarizes a selected group of studies describing specific community interventions and outcomes.
Table 1.
Summary of selected intervention studies for children with asthma and social disadvantage
| Study | Type | Target population | Description of interventions | Outcomes |
|---|---|---|---|---|
| National Cooperative Inner-City Asthma Study1 | RCT | Inner-city children with asthma, multiple sites, USA |
|
|
| Inner-City Asthma Study2 | RCT | Inner city children with atopic asthma, 7 cities, USA |
|
|
| Allies Against Asthma Initiative3,4 | Comparison group cohort | Children with asthma from low-income communities of colour, 7 regions, USA |
|
|
| La Red de Asma Infantil5 | Case study | Children with moderate - severe asthma living in 2 housing projects, San Juan, Puerto Rico, USA |
|
|
| Children’s Hospital Boston Community Asthma Initiative6 | Controlled trial | Urban children with high risk asthma, underserved community, Boston, MA, USA |
|
|
| Neighborhood Asthma Coalition7 | Controlled trial | African American children with high risk asthma, two predominantly low-income African American neighbourhoods, St Louis, Missouri, USA |
|
|
| The East London Randomised Controlled Trial for High Risk Asthma (ELECTRA)8 | RCT | Children and adults with history of acute asthma, 44 general practices in London boroughs which served deprived, multi-ethnic population, UK |
|
|
AC, asthma counsellor; AAP, asthma action plan; CHW, community health worker; ED, emergency department; IPM, integrated pest management; OCS, oral corticosteroids; PCP, primary care physician, RCT, Randomized Controlled Trial
Evans R, 3rd, Gergen PJ, Mitchell H, et al. A randomized clinical trial to reduce asthma morbidity among inner-city children: results of the National Cooperative Inner-City Asthma Study. The Journal of pediatrics 1999;135: 332–338.
Morgan WJ, Crain EF, Gruchalla RS, et al. Results of a home-based environmental intervention among urban children with asthma. The New England journal of medicine 2004;351: 1068–1080.
Clark NM, Lachance L, Doctor LJ, et al. Policy and system change and community coalitions: outcomes from allies against asthma. American journal of public health 2010;100: 904–912.
Clark NM, Lachance LL, Benedict MB, et al. Improvements in health care use associated with community coalitions: long-term results of the allies against asthma initiative. American journal of public health 2013;103: 1124–1127.
Lara M, Ramos-Valencia G, Gonzalez-Gavillan JA, et al. Reducing quality-of-care disparities in childhood asthma: La Red de Asma Infantil intervention in San Juan, Puerto Rico. Pediatrics 2013;131 Suppl 1: S26–37.
Woods ER, Bhaumik U, Sommer SJ, et al. Community asthma initiative: evaluation of a quality improvement program for comprehensive asthma care. Pediatrics 2012;129: 465–472.
Fisher EB, Strunk RC, Sussman LK, Sykes RK, Walker MS. Community organization to reduce the need for acute care for asthma among African American children in low-income neighborhoods: the Neighborhood Asthma Coalition. Pediatrics 2004;114: 116–123.
Griffiths C, Foster G, Barnes N, et al. Specialist nurse intervention to reduce unscheduled asthma care in a deprived multiethnic area: the east London randomised controlled trial for high risk asthma (ELECTRA). BMJ 2004;328: 144.
Conclusion
Socially disadvantaged children with asthma have elevated asthma morbidity. The reasons for this are multifactorial and many inextricable from each other (see Figure 1). Specific factors such as SES, minority affiliation, psychosocial stress, and environmental exposures are the most well-described. It is difficult to tease out the magnitude of effect of each of these issues, as they are likely to interact in a complex manner to ultimately influence asthma outcomes. There have been promising social, behavioural, environmental, and medical interventions studied in recent years, trying to improve asthma outcomes among various socially disadvantaged populations. Multifaceted approaches that are culturally sensitive and that target several aspects of asthma control will likely be the most successful.
Figure 1.
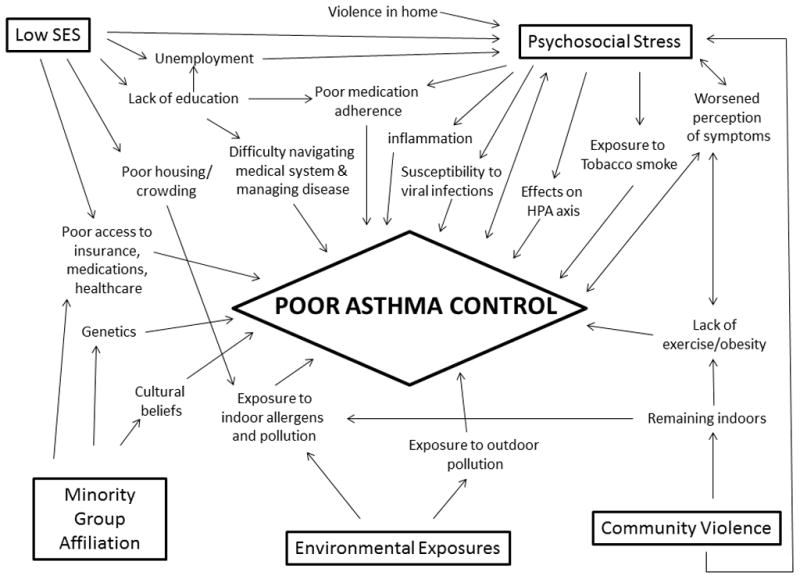
Possible Mechanisms for the Association Between Social Disadvantage and Poor Asthma Control
Educational Aims
To define social disadvantage and the elements that constitute it
To describe the most recent and relevant literature linking elements of social disadvantage (socioeconomic status, psychosocial stress/violence exposure, minority affiliation, and environmental exposures) with asthma control in children
To explore possible mechanisms explaining why these associations exist
To draw the reader’s attention to community-based and environmental interventions that have reported asthma outcomes among socially disadvantaged paediatric patients
Practice Points
Low socioeconomic status, exposure to psychosocial stress, exposure to violence, racial or ethnic minority group affiliation, exposure to environmental risks such as allergens and pollution, and poor rural environments are risk factors for worsened asthma control in children
The mechanisms behind these associations are not entirely clear and there is likely interaction between the various risk factors
Interventions designed to address these factors have been studied and show promising outcomes
Research Directions
The effectiveness of stress-reduction techniques in improving asthma outcomes in children
Further studies of cost effectiveness of community intervention strategies in socially disadvantaged children
Interaction between genetics, race, and social disadvantage
Acknowledgments
The authors would like to acknowledge the following funding sources: Grants R01 073964, R01 A1 073964-02S1, K24 A1 106822 (PI Phipatanakul) and K23AI106945-01 (PI Gaffin) from the National Institutes of Health, U10HL098102, and Aerocrine, Inc. (Kopel). This work was conducted with the support from Harvard Catalyst/The Harvard Clinical and Translational Science Center (NIH Award # UL1 TR001102 and financial contributions from Harvard University and its affiliated academic healthcare centers. The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic healthcare centers, the National Center for Research resources, or the National Institutes of Health. These funding sources had no involvement in the writing of the manuscript.
Footnotes
Conflict of Interest Statement:
The authors do not have any conflicts of interest to disclose.
References
- 1.Administration USSB. Social Disadvantage Eligibility. [cited 2013 November 3]; Available from: http://www.sba.gov/content/social-disadvantage-eligibility.
- 2.Braveman P. Health disparities and health equity: concepts and measurement. Annu Rev Public Health. 2006;27:167–94. doi: 10.1146/annurev.publhealth.27.021405.102103. [DOI] [PubMed] [Google Scholar]
- 3.Lai CK, Beasley R, Crane J, Foliaki S, Shah J, Weiland S. Global variation in the prevalence and severity of asthma symptoms: phase three of the International Study of Asthma and Allergies in Childhood (ISAAC) Thorax. 2009;64:476–83. doi: 10.1136/thx.2008.106609. [DOI] [PubMed] [Google Scholar]
- 4.Largent J, Nickerson B, Cooper D, Delfino RJ. Paediatric asthma hospital utilization varies by demographic factors and area socio-economic status. Public Health. 2012;126:928–36. doi: 10.1016/j.puhe.2012.04.011. [DOI] [PubMed] [Google Scholar]
- 5.McConnochie KM, Russo MJ, McBride JT, Szilagyi PG, Brooks AM, Roghmann KJ. Socioeconomic variation in asthma hospitalization: excess utilization or greater need? Pediatrics. 1999;103:e75. doi: 10.1542/peds.103.6.e75. [DOI] [PubMed] [Google Scholar]
- 6.Amre DK, Infante-Rivard C, Gautrin D, Malo JL. Socioeconomic status and utilization of health care services among asthmatic children. J Asthma. 2002;39:625–31. doi: 10.1081/jas-120014927. [DOI] [PubMed] [Google Scholar]
- 7.Shields AE. Trends in private insurance, Medicaid/State Children’s Health Insurance Program, and the health-care safety net: implications for asthma disparities. Chest. 2007;132:818S–30S. doi: 10.1378/chest.07-1903. [DOI] [PubMed] [Google Scholar]
- 8.Dales RE, Choi B, Chen Y, Tang M. Influence of family income on hospital visits for asthma among Canadian school children. Thorax. 2002;57:513–7. doi: 10.1136/thorax.57.6.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Forbes L, Harvey S, Newson R, Jarvis D, Luczynska C, Price J, Burney P. Risk factors for accident and emergency (A&E) attendance for asthma in inner city children. Thorax. 2007;62:855–60. doi: 10.1136/thx.2006.058362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patel MR, Brown RW, Clark NM. Perceived parent financial burden and asthma outcomes in low-income, urban children. J Urban Health. 2013;90:329–42. doi: 10.1007/s11524-012-9774-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kit BK, Simon AE, Brody DJ, Akinbami LJ. US prevalence and trends in tobacco smoke exposure among children and adolescents with asthma. Pediatrics. 2013;131:407–14. doi: 10.1542/peds.2012-2328. [DOI] [PubMed] [Google Scholar]
- 12.Kattan M, Mitchell H, Eggleston P, Gergen P, Crain E, Redline S, Weiss K, Evans R, 3rd, Kaslow R, Kercsmar C, Leickly F, Malveaux F, Wedner HJ. Characteristics of inner-city children with asthma: the National Cooperative Inner-City Asthma Study. Pediatr Pulmonol. 1997;24:253–62. doi: 10.1002/(sici)1099-0496(199710)24:4<253::aid-ppul4>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 13.Wright RJ, Cohen S, Carey V, Weiss ST, Gold DR. Parental stress as a predictor of wheezing in infancy: a prospective birth-cohort study. Am J Respir Crit Care Med. 2002;165:358–65. doi: 10.1164/ajrccm.165.3.2102016. [DOI] [PubMed] [Google Scholar]
- 14.Sandberg S, Paton JY, Ahola S, McCann DC, McGuinness D, Hillary CR, Oja H. The role of acute and chronic stress in asthma attacks in children. Lancet. 2000;356:982–7. doi: 10.1016/S0140-6736(00)02715-X. [DOI] [PubMed] [Google Scholar]
- 15.Turyk ME, Hernandez E, Wright RJ, Freels S, Slezak J, Contraras A, Piorkowski J, Persky VW. Stressful life events and asthma in adolescents. Pediatr Allergy Immunol. 2008;19:255–63. doi: 10.1111/j.1399-3038.2007.00603.x. [DOI] [PubMed] [Google Scholar]
- 16.Wright RJ, Steinbach SF. Violence: an unrecognized environmental exposure that may contribute to greater asthma morbidity in high risk inner-city populations. Environmental Health Perspectives. 2001;109:1085–9. doi: 10.1289/ehp.011091085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wright RJ, Mitchell H, Visness CM, Cohen S, Stout J, Evans R, Gold DR. Community violence and asthma morbidity: the Inner-City Asthma Study. Am J Public Health. 2004;94:625–32. doi: 10.2105/ajph.94.4.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kopel LS, Gaffin JM, Ozonoff A, Rao DR, Sheehan WJ, Friedlander JL, Permaul P, Baxi SN, Fu C, Subramanian SV, Gold DR, Phipatanakul W. Perceived neighborhood safety and asthma morbidity in the School Inner-City Asthma Study. Pediatr Pulmonol. 2014 doi: 10.1002/ppul.22986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Swahn MH, Bossarte RM. The associations between victimization, feeling unsafe, and asthma episodes among US high-school students. Am J Public Health. 2006;96:802–4. doi: 10.2105/AJPH.2005.066514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cohen RT, Canino GJ, Bird HR, Celedon JC. Violence, abuse, and asthma in Puerto Rican children. Am J Respir Crit Care Med. 2008;178:453–9. doi: 10.1164/rccm.200711-1629OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Walker J, Lewis-Land C, Kub J, Tsoukleris M, Butz A. The effect of violence on asthma: are our children facing a double-edged sword? J Community Health. 2008;33:384–8. doi: 10.1007/s10900-008-9113-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wright RJ, Finn P, Contreras JP, Cohen S, Wright RO, Staudenmayer J, Wand M, Perkins D, Weiss ST, Gold DR. Chronic caregiver stress and IgE expression, allergen-induced proliferation, and cytokine profiles in a birth cohort predisposed to atopy. Journal of Allergy and Clinical Immunology. 2004;113:1051–7. doi: 10.1016/j.jaci.2004.03.032. [DOI] [PubMed] [Google Scholar]
- 23.Chen E, Strunk RC, Bacharier LB, Chan M, Miller GE. Socioeconomic status associated with exhaled nitric oxide responses to acute stress in children with asthma. Brain Behav Immun. 2010;24:444–50. doi: 10.1016/j.bbi.2009.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen E, Fisher EB, Bacharier LB, Strunk RC. Socioeconomic status, stress, and immune markers in adolescents with asthma. Psychosom Med. 2003;65:984–92. doi: 10.1097/01.psy.0000097340.54195.3c. [DOI] [PubMed] [Google Scholar]
- 25.Chen E, Miller GE. Stress and inflammation in exacerbations of asthma. Brain Behav Immun. 2007;21:993–9. doi: 10.1016/j.bbi.2007.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Oraka E, Iqbal S, Flanders WD, Brinker K, Garbe P. Racial and ethnic disparities in current asthma and emergency department visits: findings from the National Health Interview Survey, 2001–2010. J Asthma. 2013;50:488–96. doi: 10.3109/02770903.2013.790417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Netuveli G, Hurwitz B, Levy M, Fletcher M, Barnes G, Durham SR, Sheikh A. Ethnic variations in UK asthma frequency, morbidity, and health-service use: a systematic review and meta-analysis. Lancet. 2005;365:312–7. doi: 10.1016/S0140-6736(05)17785-X. [DOI] [PubMed] [Google Scholar]
- 28.McDaniel M, Paxson C, Waldfogel J. Racial disparities in childhood asthma in the United States: evidence from the National Health Interview Survey, 1997 to 2003. Pediatrics. 2006;117:e868–77. doi: 10.1542/peds.2005-1721. [DOI] [PubMed] [Google Scholar]
- 29.Smith LA, Bokhour B, Hohman KH, Miroshnik I, Kleinman KP, Cohn E, Cortes DE, Galbraith A, Rand C, Lieu TA. Modifiable risk factors for suboptimal control and controller medication underuse among children with asthma. Pediatrics. 2008;122:760–9. doi: 10.1542/peds.2007-2750. [DOI] [PubMed] [Google Scholar]
- 30.Leaderer BP, Belanger K, Triche E, Holford T, Gold DR, Kim Y, Jankun T, Ren P, McSharry Je JE, Platts-Mills TA, Chapman MD, Bracken MB. Dust mite, cockroach, cat, and dog allergen concentrations in homes of asthmatic children in the northeastern United States: impact of socioeconomic factors and population density. Environ Health Perspect. 2002;110:419–25. doi: 10.1289/ehp.02110419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kitch BT, Chew G, Burge HA, Muilenberg ML, Weiss ST, Platts-Mills TA, O’Connor G, Gold DR. Socioeconomic predictors of high allergen levels in homes in the greater Boston area. Environ Health Perspect. 2000;108:301–7. doi: 10.1289/ehp.00108301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stevenson LA, Gergen PJ, Hoover DR, Rosenstreich D, Mannino DM, Matte TD. Sociodemographic correlates of indoor allergen sensitivity among United States children. J Allergy Clin Immunol. 2001;108:747–52. doi: 10.1067/mai.2001.119410. [DOI] [PubMed] [Google Scholar]
- 33.Forno E, Celedon JC. Asthma and ethnic minorities: socioeconomic status and beyond. Curr Opin Allergy Clin Immunol. 2009;9:154–60. doi: 10.1097/aci.0b013e3283292207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mathias RA, Grant AV, Rafaels N, Hand T, Gao L, Vergara C, Tsai YJ, Yang M, Campbell M, Foster C, Gao P, Togias A, Hansel NN, Diette G, Adkinson NF, Liu MC, Faruque M, Dunston GM, Watson HR, Bracken MB, Hoh J, Maul P, Maul T, Jedlicka AE, Murray T, Hetmanski JB, Ashworth R, Ongaco CM, Hetrick KN, Doheny KF, Pugh EW, Rotimi CN, Ford J, Eng C, Burchard EG, Sleiman PM, Hakonarson H, Forno E, Raby BA, Weiss ST, Scott AF, Kabesch M, Liang L, Abecasis G, Moffatt MF, Cookson WO, Ruczinski I, Beaty TH, Barnes KC. A genome-wide association study on African-ancestry populations for asthma. J Allergy Clin Immunol. 2010;125:336–46. e4. doi: 10.1016/j.jaci.2009.08.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Galanter J, Choudhry S, Eng C, Nazario S, Rodriguez-Santana JR, Casal J, Torres-Palacios A, Salas J, Chapela R, Watson HG, Meade K, LeNoir M, Rodriguez-Cintron W, Avila PC, Burchard EG. ORMDL3 gene is associated with asthma in three ethnically diverse populations. Am J Respir Crit Care Med. 2008;177:1194–200. doi: 10.1164/rccm.200711-1644OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Choudhry S, Burchard EG, Borrell LN, Tang H, Gomez I, Naqvi M, Nazario S, Torres A, Casal J, Martinez-Cruzado JC, Ziv E, Avila PC, Rodriguez-Cintron W, Risch NJ. Ancestry-environment interactions and asthma risk among Puerto Ricans. Am J Respir Crit Care Med. 2006;174:1088–93. doi: 10.1164/rccm.200605-596OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Reibman J, Liu M. Genetics and asthma disease susceptibility in the US Latino population. Mt Sinai J Med. 2010;77:140–8. doi: 10.1002/msj.20171. [DOI] [PubMed] [Google Scholar]
- 38.Scirica CV, Celedon JC. Genetics of asthma: potential implications for reducing asthma disparities. Chest. 2007;132:770S–81S. doi: 10.1378/chest.07-1905. [DOI] [PubMed] [Google Scholar]
- 39.IOM; Committee on the Assessment of Asthma and Indoor Air IoM, editor. Clearing the air: asthma and indoor air exposures. Washington, DC: National Academy Press; 2000. [Google Scholar]
- 40.Sheehan WJ, Rangsithienchai PA, Wood RA, Rivard D, Chinratanapisit S, Perzanowski MS, Chew GL, Seltzer JM, Matsui EC, Phipatanakul W. Pest and allergen exposure and abatement in inner-city asthma: a work group report of the American Academy of Allergy, Asthma & Immunology Indoor Allergy/Air Pollution Committee. J Allergy Clin Immunol. 2010;125:575–81. doi: 10.1016/j.jaci.2010.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Eggleston PA, Rosenstreich D, Lynn H, Gergen P, Baker D, Kattan M, Mortimer KM, Mitchell H, Ownby D, Slavin R, Malveaux F. Relationship of indoor allergen exposure to skin test sensitivity in inner-city children with asthma. J Allergy Clin Immunol. 1998;102:563–70. doi: 10.1016/s0091-6749(98)70272-6. [DOI] [PubMed] [Google Scholar]
- 42.Rosenstreich DL, Eggleston P, Kattan M, Baker D, Slavin RG, Gergen P, Mitchell H, McNiff-Mortimer K, Lynn H, Ownby D, Malveaux F. The role of cockroach allergy and exposure to cockroach allergen in causing morbidity among inner-city children with asthma. N Engl J Med. 1997;336:1356–63. doi: 10.1056/NEJM199705083361904. [DOI] [PubMed] [Google Scholar]
- 43.Gruchalla RS, Pongracic J, Plaut M, Evans R, 3rd, Visness CM, Walter M, Crain EF, Kattan M, Morgan WJ, Steinbach S, Stout J, Malindzak G, Smartt E, Mitchell H. Inner City Asthma Study: relationships among sensitivity, allergen exposure, and asthma morbidity. J Allergy Clin Immunol. 2005;115:478–85. doi: 10.1016/j.jaci.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 44.Phipatanakul W, Eggleston PA, Wright EC, Wood RA. Mouse allergen. II. The relationship of mouse allergen exposure to mouse sensitization and asthma morbidity in inner-city children with asthma. J Allergy Clin Immunol. 2000;106:1075–80. doi: 10.1067/mai.2000.110795. [DOI] [PubMed] [Google Scholar]
- 45.Matsui EC, Eggleston PA, Buckley TJ, Krishnan JA, Breysse PN, Rand CS, Diette GB. Household mouse allergen exposure and asthma morbidity in inner-city preschool children. Ann Allergy Asthma Immunol. 2006;97:514–20. doi: 10.1016/S1081-1206(10)60943-X. [DOI] [PubMed] [Google Scholar]
- 46.Ahluwalia SK, Peng RD, Breysse PN, Diette GB, Curtin-Brosnan J, Aloe C, Matsui EC. Mouse allergen is the major allergen of public health relevance in Baltimore City. J Allergy Clin Immunol. 2013;132:830–5. e2. doi: 10.1016/j.jaci.2013.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sheehan WJ, Rangsithienchai PA, Muilenberg ML, Rogers CA, Lane JP, Ghaemghami J, Rivard DV, Otsu K, Hoffman EB, Israel E, Gold DR, Phipatanakul W. Mouse allergens in urban elementary schools and homes of children with asthma. Ann Allergy Asthma Immunol. 2009;102:125–30. doi: 10.1016/S1081-1206(10)60242-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Baxi SN, Muilenberg ML, Rogers CA, Sheehan WJ, Gaffin J, Permaul P, Kopel LS, Lai PS, Lane JP, Bailey A, Petty CR, Fu C, Gold DR, Phipatanakul W. Exposures to molds in school classrooms of children with asthma. Pediatr Allergy Immunol. 2013;24:697–703. doi: 10.1111/pai.12127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sheehan WJ, Hoffman EB, Fu C, Baxi SN, Bailey A, King EM, Chapman MD, Lane JP, Gaffin JM, Permaul P, Gold DR, Phipatanakul W. Endotoxin exposure in inner-city schools and homes of children with asthma. Ann Allergy Asthma Immunol. 2012;108:418–22. doi: 10.1016/j.anai.2012.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Klepeis NE, Nelson WC, Ott WR, Robinson JP, Tsang AM, Switzer P, Behar JV, Hern SC, Engelmann WH. The National Human Activity Pattern Survey (NHAPS): a resource for assessing exposure to environmental pollutants. Journal of Exposure Analysis and Environmental Epidemiology. 2001;11:231–52. doi: 10.1038/sj.jea.7500165. [DOI] [PubMed] [Google Scholar]
- 51.McCormack MC, Breysse PN, Hansel NN, Matsui EC, Tonorezos ES, Curtin-Brosnan J, Williams DL, Buckley TJ, Eggleston PA, Diette GB. Common household activities are associated with elevated particulate matter concentrations in bedrooms of inner-city Baltimore pre-school children. Environ Res. 2008;106:148–55. doi: 10.1016/j.envres.2007.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Diette GB, Hansel NN, Buckley TJ, Curtin-Brosnan J, Eggleston PA, Matsui EC, McCormack MC, Williams DL, Breysse PN. Home indoor pollutant exposures among inner-city children with and without asthma. Environ Health Perspect. 2007;115:1665–9. doi: 10.1289/ehp.10088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Belanger K, Holford TR, Gent JF, Hill ME, Kezik JM, Leaderer BP. Household levels of nitrogen dioxide and pediatric asthma severity. Epidemiology. 2013;24:320–30. doi: 10.1097/EDE.0b013e318280e2ac. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.O’Connor GT, Neas L, Vaughn B, Kattan M, Mitchell H, Crain EF, Evans R, 3rd, Gruchalla R, Morgan W, Stout J, Adams GK, Lippmann M. Acute respiratory health effects of air pollution on children with asthma in US inner cities. J Allergy Clin Immunol. 2008;121:1133–9. e1. doi: 10.1016/j.jaci.2008.02.020. [DOI] [PubMed] [Google Scholar]
- 55.Strand V, Rak S, Svartengren M, Bylin G. Nitrogen dioxide exposure enhances asthmatic reaction to inhaled allergen in subjects with asthma. Am J Respir Crit Care Med. 1997;155:881–7. doi: 10.1164/ajrccm.155.3.9117021. [DOI] [PubMed] [Google Scholar]
- 56.Wallace LA, Mitchell H, O’Connor GT, Neas L, Lippmann M, Kattan M, Koenig J, Stout JW, Vaughn BJ, Wallace D, Walter M, Adams K, Liu LJ. Particle concentrations in inner-city homes of children with asthma: the effect of smoking, cooking, and outdoor pollution. Environ Health Perspect. 2003;111:1265–72. doi: 10.1289/ehp.6135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Diette GB, McCormack MC, Hansel NN, Breysse PN, Matsui EC. Environmental issues in managing asthma. Respir Care. 2008;53:602–15. discussion 16–7. [PMC free article] [PubMed] [Google Scholar]
- 58.McCormack MC, Breysse PN, Matsui EC, Hansel NN, Williams D, Curtin-Brosnan J, Eggleston P, Diette GB. In-home particle concentrations and childhood asthma morbidity. Environ Health Perspect. 2009;117:294–8. doi: 10.1289/ehp.11770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Holguin F, Flores S, Ross Z, Cortez M, Molina M, Molina L, Rincon C, Jerrett M, Berhane K, Granados A, Romieu I. Traffic-related exposures, airway function, inflammation, and respiratory symptoms in children. Am J Respir Crit Care Med. 2007;176:1236–42. doi: 10.1164/rccm.200611-1616OC. [DOI] [PubMed] [Google Scholar]
- 60.Koenig JQ, Mar TF, Allen RW, Jansen K, Lumley T, Sullivan JH, Trenga CA, Larson T, Liu LJ. Pulmonary effects of indoor- and outdoor-generated particles in children with asthma. Environ Health Perspect. 2005;113:499–503. doi: 10.1289/ehp.7511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Delfino RJ, Quintana PJ, Floro J, Gastanaga VM, Samimi BS, Kleinman MT, Liu LJ, Bufalino C, Wu CF, McLaren CE. Association of FEV1 in asthmatic children with personal and microenvironmental exposure to airborne particulate matter. Environ Health Perspect. 2004;112:932–41. doi: 10.1289/ehp.6815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.McCormack MC, Breysse PN, Matsui EC, Hansel NN, Peng RD, Curtin-Brosnan J, Williams DL, Wills-Karp M, Diette GB. Indoor particulate matter increases asthma morbidity in children with non-atopic and atopic asthma. Ann Allergy Asthma Immunol. 2011;106:308–15. doi: 10.1016/j.anai.2011.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Perry TT, Rettiganti M, Brown RH, Nick TG, Jones SM. Uncontrolled asthma and factors related to morbidity in an impoverished, rural environment. Ann Allergy Asthma Immunol. 2012;108:254–9. doi: 10.1016/j.anai.2012.01.017. [DOI] [PubMed] [Google Scholar]
- 64.Pesek RD, Vargas PA, Halterman JS, Jones SM, McCracken A, Perry TT. A comparison of asthma prevalence and morbidity between rural and urban schoolchildren in Arkansas. Ann Allergy Asthma Immunol. 2010;104:125–31. doi: 10.1016/j.anai.2009.11.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Schei MA, Hessen JO, Smith KR, Bruce N, McCracken J, Lopez V. Childhood asthma and indoor woodsmoke from cooking in Guatemala. J Expo Anal Environ Epidemiol. 2004;14 (Suppl 1):S110–7. doi: 10.1038/sj.jea.7500365. [DOI] [PubMed] [Google Scholar]
- 66.Padhi BK, Padhy PK. Domestic fuels, indoor air pollution, and children’s health. Ann N Y Acad Sci. 2008;1140:209–17. doi: 10.1196/annals.1454.015. [DOI] [PubMed] [Google Scholar]
- 67.Li P, Guttmann A. Recent innovations to improve asthma outcomes in vulnerable children. Curr Opin Pediatr. 2009;21:783–8. doi: 10.1097/MOP.0b013e328332537d. [DOI] [PubMed] [Google Scholar]


