Introduction
Obesity rates have increased significantly in children in many parts of the world, especially in North America.1 According to data from the most recent National Health and Nutrition Examination Survey, approximately 17% (or 12.5 million) of US children and adolescents 2 to 9 years old are obese.2 The impact that childhood obesity has on pediatric diseases has become a major prevention initiative by the Obama administration and several public health organizations. Children with obesity are at increased risk for developing asthma, one of the most common chronic diseases in children.3 Childhood asthma accounts for more than 14 million missed school days per year and is the primary cause of school absences in the United States.4 A relation between obesity and asthma is supported by prospective studies in adults and children suggesting that being overweight and obese can precede the onset of asthma5 and studies in adults showing alleviation of asthma symptoms with weight loss.6 Despite consistent evidence linking obesity to the incidence and prevalence of asthma and several postulated hypotheses to explain this association, a definitive mechanism remains a mystery.
Genetic and Environmental Factors
Asthma and obesity are likely to be connected in a multifactorial fashion. Although genetic susceptibility can contribute to the development of asthma and obesity, the rapid increase in a relatively short period suggests that changes in lifestyle, such as diet, physical activity, early life exposures, and other environmental interactions, also can play a role. Epigenetic mechanisms associated with obesity and asthma have been proposed.
Obesity and asthma likely have their beginnings in utero and in early childhood. Diet and nutrition, especially prenatal and early infant diet, may play a part in these diseases. Greater consumption of fruits and vegetables, antioxidants, minerals and vitamins, fish, and legumes during pregnancy seems to confer protection against childhood asthma and wheeze7 and may influence the neonatal immune system and lung development.8 However, 1 study showed that fatty acid dietary supplementation during pregnancy did not lower the overall incidence of asthma.9 To further support the idea that intrauterine nutrition is important, associations between low birth weight and resulting obesity and asthma have been shown. In 1 study, low birth weight led to the development of asthma and excess body mass increased the risk.10 Rapid growth in body mass index (BMI) during the first 2 years of life increased the risk of asthma up to 6 years of age based on published data from 8 European birth cohorts.11
Mechanical Effects
Physical or mechanical effects of obesity on the respiratory system are likely to play a part in the connection between childhood obesity and asthma. Obesity affects lung function in adults with and without asthma. The most consistent data show a decrease in functional residual capacity and lower tidal volumes in obese adults, primarily because of changes in the elastic properties of the chest wall. A large prospective study enrolling children and adults with asthma reported a significantly decreased baseline forced vital capacity in obese adults but not in children.12 In fact, the Childhood Asthma Management Program showed a significantly decreased ratio of forced expiration volume in 1 second to forced vital capacity in children at or above the 85th BMI percentile compared with healthy-weight children.13 A recent study reported an overestimation of poor asthma control in obese children with asthma because of an enhanced perception of dyspnea owing to altered mechanical properties of the chest wall.14 The data for obese children are conflicting and suggest the need for more lung volume assessments in childhood obesity studies.
Further, it has been shown that the onset and duration of obesity and the composition of the excess weight (lean vs fat) also can affect lung function. For instance, 1 study showed that a higher BMI in infancy, likely owing to the deposition of lean body mass, was associated with a lower risk of asthma and greater lung function as a child, whereas the development of obesity at 5 years of age led to an increased risk of asthma and poorer lung function at 6 and 8 years of age.15 To this end, the BMI, which measures excess mass, including lean and fat, does not take into consideration the changes in body composition that occur as a child grows, which can have an effect on lung function. However, there does not seem to be strong evidence for the use of adiposity measurements other than the BMI. Forno et al16 examined the relation among atopy, asthma, and measurements of adiposity in Puerto Rican children and found that although BMI was significantly associated with asthma, the percentage of body fat, waist circumference, and waist-to-hip ratio were not significant.
Airway Hyperresponsiveness
Although there is a substantial amount of literature on airway hyperresponsiveness (AHR) as it relates to asthma and obesity in adults, data in children are lacking. AHR is a cardinal feature of asthma. When lung volumes are reduced in obese individuals, there is an associated decrease in airway diameter that, over time, can disturb smooth muscle function and increase airway obstruction and hyperresponsiveness.17 To date, the available clinical data in children on the association between obesity and AHR are inconsistent. For instance, 1 study did not find a significant difference in the prevalence of AHR between obese and normal-weight children with asthma after an exercise challenge test,18 whereas another study showed that weight loss in obese children with asthma led to a significant decrease in the severity of exercise-induced bronchoconstriction and a better quality of life.19
Inflammation
Increased systemic inflammation has been touted as a possible link between childhood asthma and obesity by potentiating airway inflammation. Obesity in humans is associated with low-grade systemic inflammation, giving rise to this idea that obesity is a “proinflammatory state.” Adipose tissue secretes adipokines, namely leptin and adiponectin, which in turn can have significant effects on metabolism and inflammation. Obese adults have higher circulating levels of leptin and interleukin-6 (which are proin-flammatory) and lower adiponectin levels, secreted inversely in relation to obesity, compared with nonobese adults.20 Similar findings have been reported in obese children with asthma compared with nonobese children with asthma, except for no differences in interleukin-6 or tumor necrosis factor-α levels.21 Higher levels of adiponectin have been associated with better asthma control in children as measured by forced expiratory flow at 25% to 75% and the ratio of forced expiration volume in 1 second to forced vital capacity and lower levels with asthma exacerbations and increased exercise-induced bronchoconstriction.21,22 In contrast, another study found no differences in leptin or adiponectin levels in obese and nonobese children with asthma.23 The effect of low-grade systemic inflammation on airway inflammation in asthma is debatable and not fully understood in the pediatric population.
Airway inflammation data from adult populations suggest that obese asthma exhibits a non-eosinophilic pattern with significant neutrophilia.20 Rastogi et al24 showed that, in children 8 to 17 years old, obese asthma was not associated with increased airway or systemic inflammation as measured by exhaled nitric oxide, sputum eosinophils, blood C-reactive protein, and interleukin-6. However, there are few sputum studies in children to date, which underscores the need for more descriptive airway inflammation research in obese children with asthma.
Many studies support that mechanisms underlying obese asthma have nonallergic origins but, unfortunately, most of these studies have looked only at adults. The association between obesity and asthma exists in children with and without atopy but is evidently stronger in the absence of atopy.25 Nonetheless, the results are conflicting in the literature. Yoo et al26 reported that overweight children were more likely to be atopic compared with children with a normal BMI. Atopy also was recently shown to significantly mediate the effect of adiposity on asthma outcomes in Puerto Rican children.16
Basic Science Mouse Model Studies
A new study looking at mouse models of obesity reported a novel finding of inflammasome activation and production of interleukin-17 by innate lymphoid cells in the lung.27 In another recent mice study, Arteaga-Solis et al28 described a noninflamma-tory mechanism relevant to obese asthma from disruption of the autonomic nervous system mediated by leptin. The lack of leptin signaling in the brain as a result of leptin resistance in obesity leads to increased parasympathetic signaling in airway smooth muscles in mice and subsequent bronchoconstriction.28 This mechanism might explain why patients with obesity and asthma might be resistant to steroids as reported by Forno et al13 who found a significant decrease in steroid efficacy in children with a higher BMI, similar to previously reported findings in the adult population. Whether these results from mice studies are applicable to humans remain to be seen and require more translational studies. However, within obese asthma, there may be subphenotypes of atopic and nonatopic and inflammatory and noninflammatory forms of disease. Such characterization would have important implications for the diagnosis and treatment of obesity plus asthma.
Conclusion
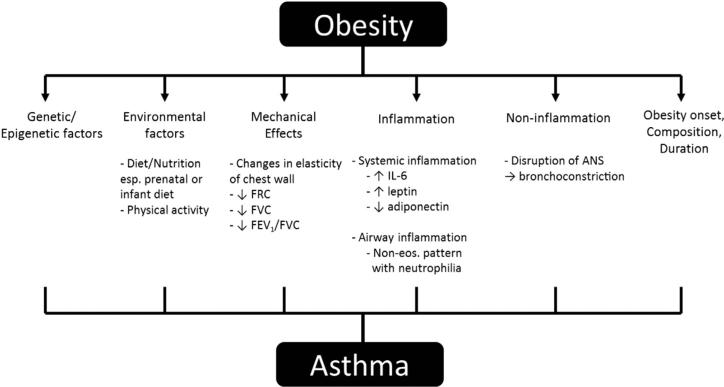
For many years researchers have been describing associations between obesity and asthma in adults. More recently, various theories to explain the connection between childhood obesity and asthma have been reported (Fig 1). There is no doubt that an association exists between these 2 conditions, although the true link remains elusive. It seems more probable that childhood obesity antedates the onset of asthma. Furthermore, the connection is likely due to more than 1 physiologic etiology and an interplay of factors. Low-grade systemic and airway inflammation, postulated to play a major role in obese asthma, may not be the only answer. Although the data are conflicting, there is mounting research evidence to support that the associated mechanism is a pathway that does not concern atopy or T-helper cell type 2. Moreover, nonin-flammatory mechanisms are emerging as an etiology in obese asthma mouse models with resulting airway bronchoconstriction. If this indeed translates to humans, the way obese children with asthma are treated will need to change from inhaled corticosteroids to bronchodilators and/or anticholinergics. Future translational studies need to be performed.
Figure 1.
Proposed pathways for the association between childhood asthma and obesity. ANS, autonomic nervous system; FCR, functional residual capacity; FEV1, forced expiration volume in 1 second; FVC, forced vital capacity; IL-6, interleukin-6.
It is important to consider the diagnostic criteria used to define asthma within individual studies because these will likely vary from study to study. This could contribute to the inconsistencies seen in the adult and pediatric literature. For many studies, a self-reported asthma diagnosis is used as the main outcome. This could lead to misclassification of asthma in the obese individual with altered physiology, reinforcing the need for studies that go beyond obesity physiology and asthma phenotyping to assess airway inflammation and potential biomarkers.
Pediatric obese asthma is a distinct clinical asthma phenotype, which will require a specialized treatment plan. As the number of obese children in the United States continues to increase, improvement in their asthma management will greatly affect the pediatric population as a whole. Studies in obese adults with asthma should not be extrapolated to children because the pathogenesis may differ. Moreover, if we are to optimize asthma treatment for obese children, it is imperative that we completely understand the nature of the relation between obesity and asthma. Additional studies are needed to more robustly characterize the mechanisms by which asthma phenotypes are altered by obesity in children.
Acknowledgments
Funding: This study was supported by NIH grants R01 AI 073964, R01AI 073964-02S1, K24 AI 106822 and U10HL098102 (PI: Phipatanakul).
This work was conducted with the support from Harvard Catalyst/The Harvard Clinical and Translational Science Center (NIH Award UL1 TR001102) and financial contributions from Harvard University and its affiliated academic healthcare centers. The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic healthcare centers, the National Center for Research Resources, or the National Institutes of Health.
Footnotes
Disclosure: Authors have nothing to report.
References
- 1.Masoli M, Fabian D, Holt S, Beasley R, Program GIfAG The global burden of asthma: executive summary of the GINA Dissemination Committee report. Allergy. 2004;59:469–478. doi: 10.1111/j.1398-9995.2004.00526.x. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA. 2010;303:242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 3.Mannino DM, Homa DM, Akinbami LJ, Moorman JE, Gwynn C, Redd SC. Surveillance for asthma—United States, 1980–1999. MMWR Surveill Summ. 2002;51:1–13. [PubMed] [Google Scholar]
- 4.Silverstein MD, Mair JE, Katusic SK, Wollan PC, O'Connell EJ, Yunginger JW. School attendance and school performance: a population-based study of children with asthma. J Pediatr. 2001;139:278–283. doi: 10.1067/mpd.2001.115573. [DOI] [PubMed] [Google Scholar]
- 5.Beuther DA, Sutherland ER. Overweight, obesity, and incident asthma: a meta-analysis of prospective epidemiologic studies. Am J Respir Crit Care Med. 2007;175:661–666. doi: 10.1164/rccm.200611-1717OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stenius-Aarniala B, Poussa T, Kvarnström J, Grönlund EL, Ylikahri M, Mustajoki P. Immediate and long term effects of weight reduction in obese people with asthma: randomised controlled study. BMJ. 2000;320:827–832. doi: 10.1136/bmj.320.7238.827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chatzi L, Torrent M, Romieu I, et al. Mediterranean diet in pregnancy is protective for wheeze and atopy in childhood. Thorax. 2008;63:507–513. doi: 10.1136/thx.2007.081745. [DOI] [PubMed] [Google Scholar]
- 8.Willers SM, Wijga AH, Brunekreef B, et al. Maternal food consumption during pregnancy and the longitudinal development of childhood asthma. Am J Respir Crit Care Med. 2008;178:124–131. doi: 10.1164/rccm.200710-1544OC. [DOI] [PubMed] [Google Scholar]
- 9.Palmer DJ, Sullivan T, Gold MS, et al. Effect of n-3 long chain polyunsaturated fatty acid supplementation in pregnancy on infants’ allergies in first year of life: randomised controlled trial. BMJ. 2012;344:e184. doi: 10.1136/bmj.e184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lu FL, Hsieh CJ, Caffrey JL, et al. Body mass index may modify asthma prevalence among low-birth-weight children. Am J Epidemiol. 2012;176:32–42. doi: 10.1093/aje/kwr484. [DOI] [PubMed] [Google Scholar]
- 11.Rzehak P, Wijga AH, Keil T, et al. Body mass index trajectory classes and incident asthma in childhood: results from 8 European birth cohorts—a Global Allergy and Asthma European Network initiative. J Allergy Clin Immunol. 2013;131:1528–1536. doi: 10.1016/j.jaci.2013.01.001. [DOI] [PubMed] [Google Scholar]
- 12.Peters JI, McKinney JM, Smith B, Wood P, Forkner E, Galbreath AD. Impact of obesity in asthma: evidence from a large prospective disease management study. Ann Allergy Asthma Immunol. 2011;106:30–35. doi: 10.1016/j.anai.2010.10.015. [DOI] [PubMed] [Google Scholar]
- 13.Forno E, Lescher R, Strunk R, et al. Decreased response to inhaled steroids in overweight and obese asthmatic children. J Allergy Clin Immunol. 2011;127:741–749. doi: 10.1016/j.jaci.2010.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sah PK, Gerald Teague W, Demuth KA, Whitlock DR, Brown SD, Fitzpatrick AM. Poor asthma control in obese children may be overestimated because of enhanced perception of dyspnea. J Allergy Clin Immunol Pract. 2013;1:39–45. doi: 10.1016/j.jaip.2012.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang Z, Lai HJ, Roberg KA, et al. Early childhood weight status in relation to asthma development in high-risk children. J Allergy Clin Immunol. 2010;126:1157–1162. doi: 10.1016/j.jaci.2010.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Forno E, Acosta-Pérez E, Brehm JM, et al. Obesity and adiposity indicators, asthma, and atopy in Puerto Rican children. J Allergy Clin Immunol. 2014;133:1308–1314.e1-5. doi: 10.1016/j.jaci.2013.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fredberg JJ, Inouye DS, Mijailovich SM, Butler JP. Perturbed equilibrium of myosin binding in airway smooth muscle and its implications in bronchospasm. Am J Respir Crit Care Med. 1999;159:959–967. doi: 10.1164/ajrccm.159.3.9804060. [DOI] [PubMed] [Google Scholar]
- 18.Consilvio NP, Di Pillo S, Verini M, et al. The reciprocal influences of asthma and obesity on lung function testing, AHR, and airway inflammation in prepubertal children. Pediatr Pulmonol. 2010;45:1103–1110. doi: 10.1002/ppul.21295. [DOI] [PubMed] [Google Scholar]
- 19.van Leeuwen JC, Hoogstrate M, Duiverman EJ, Thio BJ. Effects of dietary induced weight loss on exercise-induced bronchoconstriction in overweight and obese children [published online ahead of print October 25, 2013]. Pediatr Pulmonol. doi: 10.1002/ppul.22932. http://dx.doi.org/10.1002/ppul.22932. [DOI] [PubMed]
- 20.Scott HA, Gibson PG, Garg ML, Wood LG. Airway inflammation is augmented by obesity and fatty acids in asthma. Eur Respir J. 2011;38:594–602. doi: 10.1183/09031936.00139810. [DOI] [PubMed] [Google Scholar]
- 21.Baek HS, Kim YD, Shin JH, Kim JH, Oh JW, Lee HB. Serum leptin and adiponectin levels correlate with exercise-induced bronchoconstriction in children with asthma. Ann Allergy Asthma Immunol. 2011;107:14–21. doi: 10.1016/j.anai.2011.03.013. [DOI] [PubMed] [Google Scholar]
- 22.Kattan M, Kumar R, Bloomberg GR, et al. Asthma control, adiposity, and adipokines among inner-city adolescents. J Allergy Clin Immunol. 2010;125:584–592. doi: 10.1016/j.jaci.2010.01.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Desai D, Newby C, Symon FA, et al. Elevated sputum interleukin-5 and submucosal eosinophilia in obese individuals with severe asthma. Am J Respir Crit Care Med. 2013;188:657–663. doi: 10.1164/rccm.201208-1470OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rastogi D, Canfield SM, Andrade A, et al. Obesity-associated asthma in children: a distinct entity. Chest. 2012;141:895–905. doi: 10.1378/chest.11-0930. [DOI] [PubMed] [Google Scholar]
- 25.Visness CM, London SJ, Daniels JL, et al. Association of childhood obesity with atopic and nonatopic asthma: results from the National Health and Nutrition Examination Survey 1999–2006. J Asthma. 2010;47:822–829. doi: 10.3109/02770903.2010.489388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yoo S, Kim HB, Lee SY, et al. Association between obesity and the prevalence of allergic diseases, atopy, and bronchial hyperresponsiveness in Korean adolescents. Int Arch Allergy Immunol. 2011;154:42–48. doi: 10.1159/000319207. [DOI] [PubMed] [Google Scholar]
- 27.Kim HY, Lee HJ, Chang YJ, et al. Interleukin-17–producing innate lymphoid cells and the NLRP3 inflammasome facilitate obesity-associated airway hyperreactivity. Nat Med. 2014;20:54–61. doi: 10.1038/nm.3423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arteaga-Solis E, Zee T, Emala CW, Vinson C, Wess J, Karsenty G. Inhibition of leptin regulation of parasympathetic signaling as a cause of extreme body weight-associated asthma. Cell Metab. 2013;17:35–48. doi: 10.1016/j.cmet.2012.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]