Abstract
Objectives
To determine neonatal morbidity rates for early term birth compared to full term birth by precursor leading to delivery.
Study Design
This was a retrospective study of 188,809 deliveries from 37 0/7 to 41 6/7 weeks of gestation with electronic medical record data from 2002 to 2008. Precursors for delivery were categorized as spontaneous labor, premature rupture of membranes (PROM), indicated, and no recorded indication. After excluding anomalies, rates of neonatal morbidities by precursor were compared at each week of delivery.
Results
Early term births (37 0/7 – 38 6/7 weeks) accounted for 34.1% of term births. Overall, 53.6% of early term births were due to spontaneous labor, followed by 27.6% indicated, 15.5% with no recorded indication, and 3.3% with PROM. Neonatal intensive care unit (NICU) admission and respiratory morbidity were lowest at or beyond 39 weeks compared to the early term period for most precursors, although indicated deliveries had the highest morbidity compared to other precursors. The greatest difference in morbidity was between 37 and 39 weeks for most precursors, while most differences in morbidities between 38 and 39 weeks were not significant. Respiratory morbidity was higher at 37 than 39 weeks regardless of route of delivery.
Conclusion
Given the higher neonatal morbidity at 37 compared to 39 weeks regardless of delivery precursor, our data support recent recommendations for designating early term to include 37 weeks. Prospective data is urgently needed to determine the optimal timing of delivery for common pregnancy complications.
Keywords: Early term birth, neonatal morbidity, precursors for delivery
Introduction
Neonatal morbidity due to physiologic immaturity has been studied primarily in preterm infants less than 37 weeks’ gestation.1,2,3,4 However, more recent evidence indicates that neonatal morbidity decreases with delivery at later gestational ages and that infants delivered at 37 and 38 weeks’ gestation, are at increased risk for morbidity compared to infants delivered at 39 weeks.5,6,7,8 Specifically, rates of respiratory distress syndrome, transient tachypnea of the newborn, pneumonia, hypothermia, and feeding difficulties are increased in infants born at 37 to 38 weeks compared to infants born after 38 weeks.8,9,10 An increased rate of cerebral palsy, a more severe complication, has also been observed in infants born at 37 weeks compared to 38 weeks’ gestation.11 Long term childhood morbidities including increased risk of problems with school performance and behavior, increased hospital admission up to 5 years of age, and increased rates of asthma and wheezing have also been observed in children born at 37 to 38 weeks compared to those born after 38 weeks’ gestation.12
The small but measurable increased risk of neonatal morbidity for infants born at 37 and 38 compared to 39 weeks’ gestation led Fleischman et al13 to suggest adoption of an “early term” delivery category. Subsequently, the American College of Obstetrics and Gynecology (ACOG) recommended designating 37 to 38 completed weeks’ gestation as “early term” and 39 to 40 weeks’ gestation as “full term”.14 The potential public health impact of early term delivery is large as 27% of all deliveries in the United States occurred at 37 and 38 weeks’ gestation in 201015 and in one study, approximately 50% of 20,973 elective term cesarean deliveries occurred during the early term period.16
Both the reason and gestational age at delivery are likely important factors contributing to morbidity, as neonatal morbidity has been found to vary depending on the underlying indication for delivery between 34 and 36 weeks of gestation.17 However, there has been a paucity of data regarding whether increased morbidity in early term neonates is a consequence of physiologic immaturity at earlier gestation or due to the underlying precursor leading to early term delivery.
Therefore, our objectives were to determine if morbidity differed in neonates born during the early term and full term period by delivery precursor and to describe the precursors leading to early term birth using data from a large U.S. obstetrical cohort. We further explored incidence of respiratory morbidity according to planned versus actual route of delivery for different precursors.
Materials and Methods
This was a retrospective study based on data from the Consortium on Safe Labor (CSL) which has been described elsewhere.18 The study included 12 sites (including 19 hospitals) across the United States with deliveries between 2002 and 2008. Institutional review board approval was obtained from each facility within the CSL. Maternal demographic data, labor and delivery information, birth records, and neonatal information were extracted from the patient electronic medical records and supplemented with discharge summary codes. Validation studies comparing discharge codes with medical chart review confirmed high level of accuracy. Overall, there was 91.1% to 95% concordance with the medical chart for 20 variables examined.18
Data was also collected from chart review for all infants delivered >37 weeks’ gestation who required respiratory support in the delivery room with oxygen or ventilation and were admitted to the neonatal intensive care unit (NICU) with a respiratory diagnosis. Gestational age at delivery as recorded in the medical record was based on the best obstetrical estimate available.
There were 228,438 deliveries from 208,695 women in the CSL. We limited the current analysis to 188,809 singleton deliveries from 173,569 women with gestational ages between 37 0/7 to 41 6/7 weeks. Precursors for delivery were categorized as previously described1 into four exclusive categories: spontaneous labor, premature rupture of membranes (PROM), indicated, and no recorded indication. We classified the precursors for delivery according to the following hierarchy: women who presented in spontaneous labor with and without pregnancy complications or rupture of membranes were only included in the spontaneous labor category. A pregnancy was determined to be PROM exclusive of spontaneous labor if a woman presented with premature rupture of membranes and underwent an induction of labor or prelabor cesarean delivery. Indicated deliveries included women without spontaneous labor or PROM who underwent an induction of labor or prelabor cesarean delivery for maternal, fetal, or obstetric complications of pregnancy. If an induction of labor or indication for prelabor cesarean delivery was not recorded, but the pregnancy had other complications such as hypertensive disease or diabetes, it was also categorized as indicated. Therefore, a woman could potentially have multiple pregnancy conditions in the indicated category. Finally, admission for a fetal or maternal reason not specified in the above categories, as well as history of fetal or maternal condition not present in the current pregnancy were considered indicated. Postdates, defined as 41 0/7 to 41 6/7 weeks of gestation, was also counted as an indicated delivery exclusive of other indications. In a previous study1, we determined that birth outcomes for deliveries that had “elective” stated as the indication were similar to that for uncomplicated pregnancies with no recorded indication. Therefore, we combined elective cesarean deliveries and labor inductions with no other complications noted in the medical record along with deliveries without a recorded indication into the no recorded indication category.
The incidences of neonatal outcomes for the specific delivery precursors by gestational week were calculated. Neonatal outcomes included neonatal intensive care unit (NICU) admission; respiratory morbidity; sepsis or evaluation to rule out sepsis; hypoxic ischemic encephalopathy (HIE), asphyxia, or seizures; and birth trauma. Neonatal respiratory morbidity included any of the following conditions requiring NICU admission: oxygen therapy with nasal cannula, continuous positive airway pressure (CPAP), bilevel positive airway pressure (BPAP), ventilator use, or diagnosis of respiratory distress syndrome (RDS), hyaline membrane disease (HMD), pneumonia, apnea, bradycardia, pulmonary hypertension, pneumothorax, meconium aspiration, or pulmonary hypoplasia. Birth trauma included epicranial subaponeurotic hemorrhage, scalp injury, clavicular fracture, facial nerve or brachial plexus injury, other cranial or peripheral nerves injuries, and other specified or unspecified birth trauma. Composite neonatal morbidity, which included NICU admission, respiratory morbidity, sepsis or evaluation to rule out sepsis, neurological morbidity, and birth trauma was calculated at each week gestational age for each major precursor. Since cesarean delivery is an independent risk factor for respiratory morbidity19, we compared estimates of planned and actual route of delivery on neonatal respiratory morbidity by gestational age at delivery and precursor.
Characteristics of mothers and newborns according to precursor for delivery were calculated for early term (37 – 38 6/7 weeks) and full term (39 – 41 6/7 weeks) birth. Significance testing was performed to compare characteristics across the four major precursors of early term birth using either ordinal (categorical variables) or logistic (binary variables) regression with generalized estimating equations (GEE) to account for correlations between pregnancies to the same mother (PROC GENMOD). The rates of deliveries for each gestational week were calculated according to precursor with significance testing performed using generalized linear models (GLMs) with GEE. Deliveries with anomalies (n=11,559) and antepartum stillbirth prior to onset of labor (n=228) were then excluded. There were 7 deliveries associated with both anomalies and stillbirth leaving 177,029 deliveries in our analyses of morbidities. The neonatal morbidity rates for each precursor were calculated for each gestational week at delivery and tested for significance using GLMs with GEE to obtain a global P-value with contrast statements to calculate for significant differences between individual weeks of gestation (e.g. 37 versus 39 and 38 versus 39 weeks). A similar analysis was performed to calculate rates of serious respiratory morbidity by gestational age at delivery and precursor according to planned and actual route of delivery. The incidences of stillbirth or perinatal mortality in ongoing pregnancies reaching a specific week of gestation were compared using Cox proportional hazard models. Given the number of comparisons, a P value of <.01 was considered significant. Statistical analysis was performed using SAS 9.3.
Results
Among term deliveries, 64,476 (34.1%) were early term between 37 0/7 and 38 6/7 weeks’ gestation while 124,333 (65.9%) were full term between 39 0/7 and 41 6/7 weeks. Characteristics of mothers and newborns according to precursor for delivery are presented in Table 1. Women who underwent an indicated delivery during the early term period were more likely to be non-Hispanic black, have a history of preterm birth, and have an infant weighing <2,500 or >4,000 grams compared to deliveries among the other three precursors for early term birth (P<.001).
Table 1.
Characteristics of mothers and newborns according to precursor for delivery.
| Characteristic | Full
Term Birth (39–41 6/7 weeks) n=124,333 % |
Early Term Birth
n=64,476 (37–38 6/7 weeks) |
No
Recorded Indicationa n=6,691 % |
P-valuea | ||
|---|---|---|---|---|---|---|
| Spontaneousa n=35,209 % |
PROMa n=2,851 % |
Indicateda n=19,725 % |
||||
| Maternal age (yr) | ||||||
| <18 | 3.0 | 3.3 | 2.7 | 2.2 | 3.1 | |
| 18–34 | 82.4 | 83.9 | 74.9 | 76.0 | 80.8 | <.001 |
| >35 | 14.4 | 12.7 | 22.4 | 21.7 | 15.8 | |
| Missing | 0.1 | 0.1 | 0.04 | 0.1 | 0.3 | |
| Body mass index(kg/m2) | ||||||
| <25 | 10.2 | 14.5 | 12.1 | 8.7 | 15.2 | |
| 25–29.9 | 30.7 | 32.6 | 31.0 | 23.8 | 34.7 | <.001 |
| >30 | 37.0 | 32.8 | 38.7 | 46.8 | 35.9 | |
| Missing | 22.2 | 20.1 | 18.2 | 20.7 | 14.2 | |
| Race | ||||||
| Non-Hispanic white | 51.7 | 51.2 | 47.6 | 45.2 | 46.3 | |
| Non-Hispanic black | 19.7 | 20.6 | 21.8 | 26.8 | 23.6 | <.001 |
| Hispanic | 17.5 | 16.9 | 16.6 | 17.9 | 19.9 | |
| Asian or Pacific Islander | 4.2 | 4.9 | 7.7 | 4.3 | 4.0 | |
| Other | 6.8 | 6.4 | 6.2 | 5.8 | 6.3 | |
| Marital status | ||||||
| Married | 61.5 | 60.1 | 61.4 | 60.2 | 60.3 | |
| Divorced/widowed | 1.3 | 1.7 | 1.3 | 1.9 | 1.7 | .054 |
| Single | 34.0 | 34.8 | 33.3 | 34.4 | 34.7 | |
| Unknown | 3.2 | 3.4 | 4.1 | 3.5 | 3.4 | |
| Insurance type | ||||||
| Private | 58.6 | 59.8 | 55.0 | 56.0 | 50.9 | |
| Public | 29.0 | 32.0 | 23.8 | 33.9 | 24.8 | <.001 |
| Self Pay | 1.2 | 1.0 | 1.7 | 1.2 | 1.1 | |
| Other | 11.2 | 7.2 | 19.5 | 8.9 | 23.2 | |
| Parity | ||||||
| Nulliparous | 42.3 | 34.1 | 51.5 | 32.4 | 41.7 | <.001 |
| 1 | 30.0 | 32.9 | 27.5 | 35.4 | 30.9 | |
| >2 | 27.8 | 33.1 | 21.1 | 32.2 | 27.3 | |
| History of preterm birth | ||||||
| Yes | 4.0 | 9.4 | 6.5 | 10.3 | 6.1 | <.001 |
| No/unknown | 96.1 | 90.6 | 93.5 | 89.7 | 93.9 | |
| History of cesarean delivery | ||||||
| Yes | 11.5 | 10.8 | 15.4 | 33.7 | 0 | <.001 |
| No/unknown | 88.5 | 89.2 | 84.6 | 66.3 | 100.0 | |
| Smoker | ||||||
| Yes | 5.5 | 6.4 | 6.8 | 6.5 | 5.0 | <.001 |
| No/unknown | 94.5 | 93.6 | 93.2 | 93.5 | 95.0 | |
| Birth weight (gm) | ||||||
| <2,500 | 0.8 | 3.8 | 6.4 | 7.3 | 2.9 | |
| 2,500–4,000 | 87.9 | 92.2 | 90.2 | 85.8 | 93.7 | <.001 |
| >4,000 | 10.2 | 3.0 | 2.6 | 6.1 | 2.9 | |
| Unknown | 1.1 | 1.0 | 0.8 | 0.9 | 0.5 | |
| Birth attendant | <.001 | |||||
| Attending | 80.8 | 79.1 | 86.8 | 90.1 | 86.6 | |
| Midwife | 6.7 | 6.7 | 4.6 | 1.4 | 0.8 | |
| Attending and Midwife | 10.9 | 12.6 | 7.6 | 7.0 | 11.4 | |
| Unknown | 1.6 | 1.7 | 1.0 | 1.5 | 1.1 | |
| Physician age (yr) | ||||||
| <40 | 23.1 | 23.0 | 26.5 | 23.7 | 23.3 | |
| 40–49 | 30.2 | 31.5 | 28.1 | 37.2 | 35.5 | <.001 |
| 50–59 | 21.4 | 22.6 | 16.9 | 18.0 | 17.5 | |
| >60 | 12.9 | 11.8 | 10.5 | 11.6 | 11.5 | |
| Unknown | 12.5 | 11.1 | 18.1 | 9.5 | 12.3 | |
| Hospital Type | ||||||
| University | 37.4 | 31.8 | 53.1 | 53.9 | 63.9 | <.001 |
| Community teaching | 54.1 | 57.3 | 44.8 | 42.8 | 32.4 | |
| Community nonteaching | 8.5 | 10.9 | 2.1 | 3.3 | 3.8 | |
| Region | ||||||
| West | 33.4 | 38.3 | 32.6 | 19.1 | 23.1 | |
| Midwest | 11.5 | 12.0 | 10.9 | 12.9 | 6.1 | <.001 |
| South | 27.4 | 26.7 | 25.4 | 44.5 | 54.8 | |
| Northeast | 27.6 | 23.1 | 31.1 | 23.5 | 16.0 | |
PROM, premature rupture of membranes
Calculated P-values correspond to differences in demographic factors among the four precursor groups for early term birth and are obtained from ordinal or logistic regression with generalized estimating equations.
Overall, 53.6% of term deliveries occurred with spontaneous labor, followed by indicated (27.6%), no recorded indication (15.5%), and PROM (3.3%) (Table 2). With increasing gestational age at delivery until 39 weeks, the percentage of spontaneous labor, PROM, and most indications decreased while those with no recorded indication increased. At 40 weeks of gestation the spontaneous labor rate was highest (58.1%, P<.001).
Table 2.
Precursors for term birth according to completed week of gestation at delivery.
| Precursor for delivery | Total N=188,809 % |
37 weeksa n=20,392 % |
38 weeksa n=44,084 % |
39 weeksa n=66,514 % |
40 weeksa n=43,471 % |
41 weeksa n=14,348 % |
P- valuea |
|---|---|---|---|---|---|---|---|
| Spontaneous labor | 53.6 | 55.2 | 54.3 | 52.2 | 58.1 | 41.7 | <.001 |
| PROM | 3.3 | 5.3 | 4.0 | 2.8 | 2.8 | 2.1 | <.001 |
| Indicatedb | 27.6 | 31.9 | 30.0 | 24.3 | 18.7 | 56.2 | <.001 |
| Chorioamnionitis | 0.3 | 0.2 | 0.2 | 0.2 | 0.4 | 0.7 | <.001 |
| Abruption | 0.6 | 1.0 | 0.6 | 0.6 | 0.4 | 0.6 | <.001 |
| Placenta previa | 0.2 | 0.8 | 0.3 | 0.2 | 0.1 | 0.1 | <.001 |
| Gestational hypertension | 2.7 | 4.6 | 3.5 | 2.3 | 2.0 | 1.4 | <.001 |
| Preeclampsia | 3.5 | 7.3 | 4.2 | 2.7 | 2.8 | 2.5 | <.001 |
| Superimposed preeclampsia | 0.4 | 1.2 | 0.5 | 0.2 | 0.2 | 0.1 | <.001 |
| Eclampsia | 0.1 | 0.2 | 0.1 | 0.04 | 0.1 | 0.04 | <.001 |
| Chronic hypertension | 1.7 | 3.1 | 2.4 | 1.6 | 1.0 | 1.0 | <.001 |
| Unspecified HTN | 0.2 | 0.3 | 0.3 | 0.2 | 0.2 | 0.2 | <.001 |
| Maternal conditionc | 7.1 | 11.2 | 9.4 | 6.8 | 4.3 | 3.9 | <.001 |
| Gestational diabetes | 4.8 | 7.5 | 6.5 | 4.9 | 2.8 | 1.6 | <.001 |
| Pregestational diabetes | 1.2 | 3.2 | 1.7 | 0.8 | 0.4 | 0.3 | <.001 |
| Fetal anomaly | 5431 | 3.48 | 3.1 | 2.8 | 2.4 | 3.3 | <.001 |
| Stillbirth | 142 | 0.21 | 0.1 | 0.0 | 0.1 | 0.1 | <.001 |
| Suspected fetal macrosomia | 1.2 | 1.0 | 1.4 | 1.2 | 1.0 | 1.1 | <.001 |
| Fetal conditiond | 6.0 | 8.5 | 6.0 | 4.3 | 6.5 | 9.2 | <.001 |
| Maternal fever | 0.1 | 0.2 | 0.1 | 0.1 | 0.1 | 0.3 | <.001 |
| Admission for fetal reasone | 0.3 | 0.3 | 0.3 | 0.2 | 0.4 | 0.7 | <.001 |
| Admission for maternal reason | 0.2 | 0.3 | 0.2 | 0.2 | 0.2 | 0.5 | <.001 |
| History of maternal conditionf | 0.1 | 0.1 | 0.1 | 0.1 | 0.04 | 0.03 | <.001 |
| History of fetal condition | 1.7 | 2.0 | 2.0 | 1.9 | 0.9 | 1.2 | <.001 |
| Prior uterine scar | 4.7 | 3.8 | 6.8 | 6.4 | 2.1 | 0 | <.001 |
| Postdates | 2.8 | 0 | 0 | 0 | 0 | 37.0 | <.001 |
| No recorded indication | 15.5 | 7.6 | 11.7 | 20.7 | 20.5 | 0 | <.001 |
PROM, premature rupture of membranes
Data are % unless otherwise specified
Significance testing was performed using generalized linear models (GLMs) with generalized estimating equations (GEE) and represents the global test for any difference in the characteristics across precursors for delivery.
Categories for the “indicated” precursors can add up to more than 100% because multiple obstetric or fetal conditions were included for the same pregnancy.
Maternal conditions included maternal medical problems such as cardiac or renal disease.
Fetal conditions included intrauterine growth restriction and abnormal antenatal testing.
Admission for fetal or maternal reason was included only if there was no other pregnancy condition.
History of maternal or fetal condition included pregnancy complications in a previous pregnancy only.
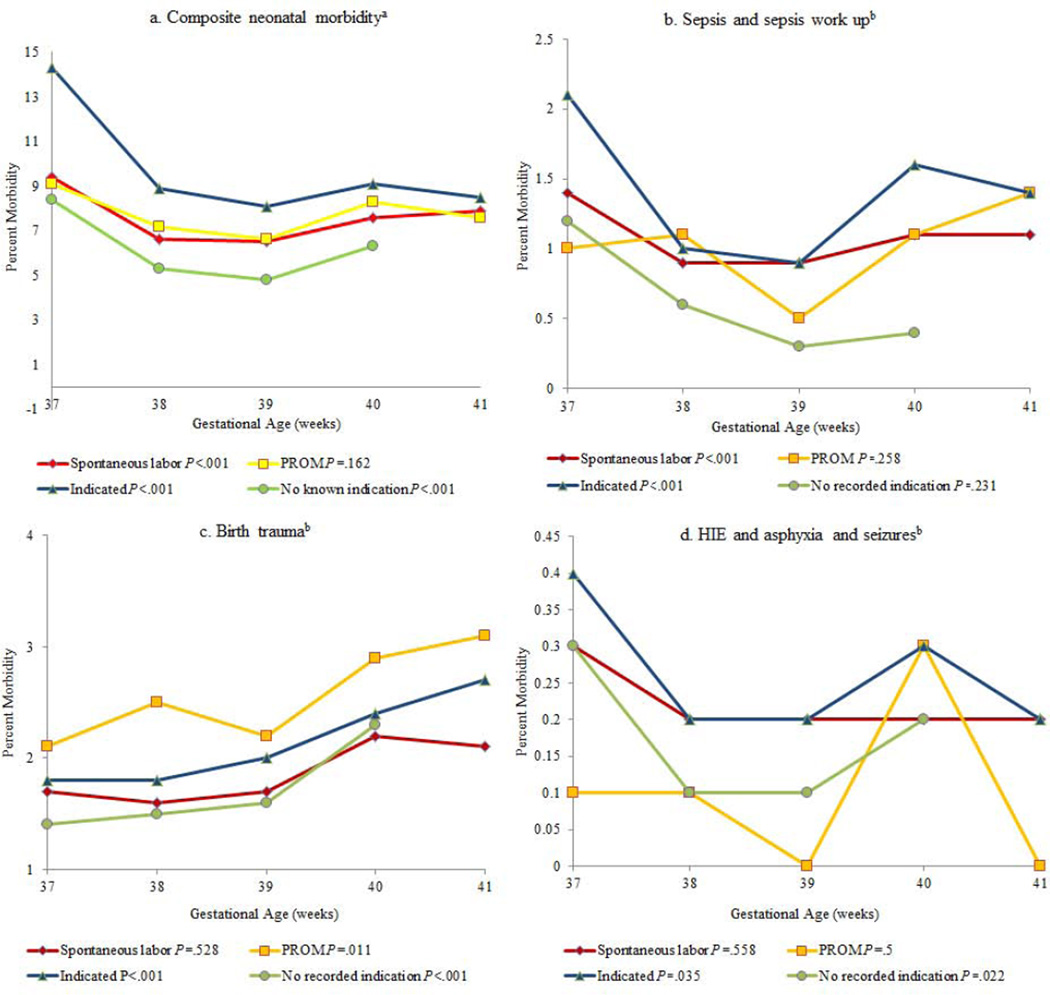
We calculated composite neonatal morbidity across gestational age for each major precursor (Figure 1, Panel a). Composite neonatal morbidity for spontaneous labor, indicated, and no known indication decreased for neonates delivered at 39 weeks compared to 37 weeks (P<.001). There was no difference in composite morbidity for PROM deliveries across term gestation (P=.162). Furthermore, there was no significant decrease in composite neonatal morbidity between 38 and 39 weeks for any major delivery precursor (P>.01 for all comparisons). The majority of neonatal morbidities were lowest at 39 weeks’ gestation (Figure 1, Panel a). We therefore used 39 week’s gestation as our reference group for statistical comparison.
Figure 1.
Composite neonatal morbidity along with rates of sepsis, birth trauma, and hypoxic ischemic encephalopathy by gestational age and precursor.
HIE, Hypoxic ischemic encephalopathy; PROM, Premature rupture of membranes
a P-values for legend correspond to composite morbidity across all weeks gestational age for each major delivery precursor. P-value <.001 for deliveries at 37 compared to 39 weeks for all major precursors except for PROM (P=.016). P-values non-significant for 38 vs. 39 weeks for each major delivery precursor (P=.029–.545)
b P-values for legends in panels b–d correspond to morbidity across all weeks gestational age for each major delivery precursor.
NICU admission rates were higher for deliveries at 37 compared to 39 weeks for spontaneous labor, PROM, indicated, and no recorded indication (P<.001 for all), but were not different for delivery at 38 versus 39 weeks except for indicated deliveries (7.5% versus 6.6%, P=.003) (Table 3). There was a 35% to 54% decrease in NICU admission from 37 to 39 weeks depending on the precursor with the largest absolute decrease occurring between weeks 37 to 38 for most precursors. NICU admission rates were not significantly different for deliveries at 38 versus 39 weeks except for pregnancies complicated by gestational diabetes (9.7% versus 7.1%, P=.008). Even in the low-risk group of deliveries with no recorded indication, NICU admission rates were increased for deliveries at 37 compared to 39 weeks (7.2% versus 3.3%, P<.001), but not significantly different for deliveries at 38 versus 39 weeks (4.0% versus 3.3%, P=.035) (Table 3).
Table 3.
NICU admission rates by gestational age and precursor for delivery.
| Precursor for deliverya N=177,029 |
37 weeks n=18,870 9.4%b % |
38
weeks n=41,111 5.8% % |
39
weeks n=62,570 5.0% % |
40
weeks n=40,973 5.6% % |
41
weeks n=13,505 6.3% % |
P- valuec 37 vs. 39 weeks |
P- valuec 38 vs. 39 weeks |
|---|---|---|---|---|---|---|---|
| Spontaneous labor (n=5,454;5.7%) | 8.1 | 5.3 | 5.1 | 5.8 | 6.3 | <.001 | .230 |
| PROM (n=315; 5.4%) | 7.1 | 4.9 | 4.6 | 6.0 | 5.4 | .005 | .636 |
| Indicated (n=3556;7.7%) | 12.8 | 7.5 | 6.6 | 7.1 | 6.4 | <.001 | .003 |
| Chorioamnionitis (n=96) | 18.6 | 18.4 | 16.0 | 21.6 | 25.6 | .693 | .657 |
| Abruption (n=127) | 17.0 | 13.4 | 11.4 | 9.0 | 12.2 | .073 | .477 |
| Placenta previa (n=45) | 14.5 | 10.2 | 7.9 | 13.0 | 16.7 | .127 | .558 |
| Gestational hypertension (n=324) | 8.9 | 6.6 | 6.0 | 6.2 | 7.3 | .008 | .516 |
| Preeclampsia (n=602) | 13.2 | 9.0 | 8.8 | 7.6 | 12.5 | .001 | .840 |
| Superimposed preeclampsia (n=82) | 15.4 | 11.3 | 7.7 | 8.9 | 11.1 | .029 | .270 |
| Eclampsia (n=18) | 24.1 | 9.7 | 11.5 | 18.2 | 16.7 | .242 | .819 |
| Chronic hypertension (n=267) | 12.6 | 8.3 | 7.8 | 6.3 | 12.2 | .002 | .700 |
| Unspecified HTN (n=39) | 18.2 | 8.0 | 6.3 | 6.4 | 21.7 | .015 | .601 |
| Maternal conditiond (n=1079) | 12.0 | 8.6 | 7.2 | 8.3 | 10.7 | <.001 | .016 |
| Gestational diabetes (n=731) | 11.7 | 9.7 | 7.1 | 7.4 | 8.2 | <.001 | .008 |
| Pregestational diabetes (n=266) | 18.5 | 12.6 | 11.0 | 6.8 | 14.7 | .005 | .315 |
| Suspected fetal macrosomia (n=177) | 13.0 | 9.9 | 6.9 | 8.2 | 8.8 | .007 | .052 |
| Fetal conditione (n=1003) | 15.2 | 8.1 | 8.6 | 8.4 | 10.1 | <.001 | .497 |
| Maternal fever (n=46) | 24.4 | 11.5 | 20.0 | 17.8 | 12.8 | .578 | .179 |
| Admission for fetal reasonf (n=31) | 16.1 | 8.0 | 2.9 | 2.1 | 2.1 | .003 | .058 |
| Admission for maternal reason (n=23) | 7.1 | 3.1 | 4.0 | 4.3 | 10.8 | .374 | .742 |
| History of maternal conditiong (n=9) | 9.1 | 8.5 | 3.4 | 0 | 0 | .271 | .216 |
| History of fetal condition (n=229) | 11.1 | 8.5 | 7.7 | 4.3 | 4.4 | .044 | .523 |
| Prior uterine scar (n=617) | 14.2 | 6.8 | 5.8 | 6.3 | 0 | <.001 | .070 |
| Postdates (n=268) | 5.0 | - | - | ||||
| No recorded indication (n=1133;3.9%) | 7.2 | 4.0 | 3.3 | 4.1 | <.001 | .035 |
PROM, Premature rupture of membranes; NICU, Neonatal intensive care unit
Fetal anomalies (n=11,559), antepartum stillbirth prior to onset of labor (n=228), and deliveries associated with both fetal anomalies and stillbirth (n=7) excluded from analysis.
Column heading percent is percent of neonates admitted to the NICU for each week gestational age. Row heading percent is percent of neonates admitted to the NICU among deliveries with that precursor.
P-values based on generalized linear models (GLMs) with generalized estimating equations (GEE) and contrast statements to calculate for significant differences between individual weeks of gestation (e.g. 37 versus 39 and 38 versus 39 weeks).
Maternal conditions included maternal medical problems such as cardiac or renal disease.
Fetal conditions included intrauterine growth restriction and abnormal antenatal testing.
Admission for fetal or maternal reason was included only if there was no other pregnancy condition.
History of maternal or fetal condition included pregnancy complications in a previous pregnancy only.
Serious neonatal respiratory morbidity was also higher with delivery at 37 compared to 39 weeks for spontaneous labor, indicated, and no recorded indication deliveries (P<.001) (Table 4). There were no significant differences in neonatal respiratory morbidity for deliveries at 38 compared to 39 weeks of gestation with the exception of deliveries with no recorded indication (1.3% versus 0.7%, P=.004).
Table 4.
Respiratory morbidity rates by gestational age and precursor for delivery.
| Precursor for deliverya N=177,029 |
37 weeks n=18,870 3.0%b % |
38
weeks n=41,111 1.5% % |
39
weeks n=62,570 1.3% % |
40
weeks n=40,973 1.6% % |
41
weeks n=13,505 1.7% % |
P- valuec 37 vs. 39 weeks |
P- valuec 38 vs. 39 weeks |
|---|---|---|---|---|---|---|---|
| Spontaneous labor (n=1499; 1.6%) | 2.7 | 1.4 | 1.3 | 1.6 | 1.8 | <.001 | .519 |
| PROM (n=81; 1.4%) | 1.5 | 1.3 | 1.2 | 1.8 | 1.4 | .528 | .838 |
| Indicated (n=929; 2.0%) | 3.9 | 1.7 | 1.6 | 1.9 | 1.7 | <.001 | .611 |
| Chorioamnionitis (n=13) | 0 | 1.3 | 2.4 | 2.7 | 5.8 | - | .599 |
| Abruption (n=40) | 6.3 | 3.0 | 3.7 | 4.0 | 2.4 | .191 | .657 |
| Placenta previa (n=11) | 4.3 | 0.8 | 2.0 | 8.7 | 0 | .327 | .448 |
| Gestational hypertension (n=86) | 4.3 | 2.0 | 1.8 | 2.2 | 4.1 | .038 | .362 |
| Preeclampsia (n=177) | 2.4 | 1.6 | 1.2 | 2.4 | 2.2 | .017 | .877 |
| Superimposed preeclampsia (n=31) | 4.3 | 2.6 | 2.7 | 1.9 | 3.1 | .057 | .973 |
| Eclampsia (n=5) | 7.5 | 2.8 | 2.8 | 3.3 | 0 | .626 | - |
| Chronic hypertension (n=62) | 6.9 | 0 | 3.8 | 9.1 | 0 | .009 | .686 |
| Unspecified HTN (n=8) | 3.8 | 1.8 | 1.6 | 0.5 | 4.9 | .017 | .928 |
| Maternal conditiond (n=254) | 3.0 | 1.7 | 1.8 | 2.1 | 3.3 | .001 | .818 |
| Gestational diabetes (n=168) | 2.9 | 2.0 | 1.6 | 1.9 | 3.4 | .004 | .219 |
| Pregestational diabetes (n=53) | 4.4 | 1.8 | 2.4 | 1.7 | 0 | .064 | .486 |
| Suspected fetal macrosomia (n=42) | 3.6 | 2.7 | 0.9 | 2.0 | 3.6 | .010 | .019 |
| Fetal conditione (n=256) | 4.1 | 1.9 | 2.2 | 2.5 | 1.8 | .004 | .476 |
| Maternal fever (n=8) | 4.9 | 1.6 | 2.5 | 4.4 | 2.6 | .496 | .728 |
| Admission for fetal reasonf (n=4) | 3.6 | 1.3 | 0 | 0 | 0 | - | - |
| Admission for maternal reason (n=8) | 2.9 | 1.0 | 0 | 2.2 | 4.6 | - | - |
| History of maternal conditiong (n=1) | 0 | 2.1 | 0 | 0 | 0 | - | - |
| History of fetal condition (n=54) | 3.2 | 1.6 | 1.8 | 1.6 | 0.6 | .095 | .715 |
| Prior uterine scar (n=172) | 5.6 | 1.7 | 1.5 | 1.6 | 0 | <.001 | .618 |
| Postdates (n=80) | 1.5 | - | - | ||||
| No recorded indication (n=308) 1.1% | 2.4 | 1.3 | 0.7 | 1.2 | <.001 | .004 |
PROM, Premature rupture of membranes
Respiratory morbidity included neonates admitted to the NICU with any of the following: oxygen therapy with nasal cannula, continuous positive airway pressure, bilevel positive airway pressure, ventilator use, diagnosis of respiratory distress syndrome, hyaline membrane disease, pneumonia, apnea and bradycardia, pulmonary hypertension, pneumothorax, meconium aspiration, or pulmonary hypoplasia.
Fetal anomalies (n=11,559), antepartum stillbirth prior to onset of labor (n=228), and deliveries associated with both fetal anomalies and stillbirth (n=7) excluded from analysis.
Column heading percent is percent of neonates with respiratory morbidity for each week gestational age. Row heading percent is percent of neonates admitted to the NICU among deliveries with that precursor.
P-values based on generalized linear models (GLMs) with generalized estimating equations (GEE) and contrast statements to calculate for significant differences between individual weeks of gestation (e.g. 37 versus 39 and 38 versus 39 weeks).
Maternal conditions included maternal medical problems such as cardiac or renal disease.
Fetal conditions included intrauterine growth restriction and abnormal antenatal testing.
Admission for fetal or maternal indication was included only if there was no other pregnancy condition.
History of maternal or fetal condition included pregnancy complications in a previous pregnancy only.
We also evaluated whether serious neonatal respiratory morbidity by gestational age differed based on route of delivery (Table 5). Respiratory morbidity was highest at 37 compared to 39 weeks regardless of route of delivery for spontaneous labor, indicated delivery, and deliveries with no recorded indication (P<.001). As expected, cesarean delivery was associated with increased respiratory morbidity across gestational age, but there was a greater absolute difference in respiratory morbidity between cesarean and vaginal delivery at 37 weeks compared to later gestation (Table 5). There was no associated decrease in respiratory morbidity with delivery at 39 weeks compared to 38 weeks for spontaneous labor, PROM, or indicated deliveries. For deliveries with no recorded indication, there was no difference in neonatal respiratory morbidity between 38 and 39 weeks regardless of whether cesarean delivery was planned or not, while 39 weeks was associated with the lowest serious respiratory morbidity for planned or actual vaginal delivery.
Table 5.
Respiratory morbidity according to precursor, gestational age, and mode of delivery.
| Precursor for
delivery N=177,029a |
37 weeks n=18,870 % |
38 weeks n=41,111 % |
39 weeks n=62,570 % |
40 weeks n=40,973 % |
41 weeks n=13,505 % |
P-valueb 37 vs. 39 weeks |
P-valueb 38 vs. 39 weeks |
|---|---|---|---|---|---|---|---|
| Spontaneous labor (n=1499) | 2.7 | 1.4 | 1.3 | 1.6 | 1.8 | <.001 | .519 |
| Planned CD (n=0) | 0 | 0 | 0 | 0 | 0 | - | - |
| Planned VD (n=1499) | 2.7 | 1.4 | 1.3 | 1.6 | 1.8 | <.001 | .519 |
| Cesarean Delivery (n=469)c | 5.8 | 2.5 | 2.5 | 3.2 | 4.1 | <.001 | .934 |
| Vaginal Delivery (n=1030) | 2.1 | 1.2 | 1.1 | 1.3 | 1.4 | <.001 | .236 |
| PROM (n=81) | 1.5 | 1.3 | 1.2 | 1.8 | 1.4 | .528 | .838 |
| Planned CD (n=17) | 2.2 | 1.9 | 2.3 | 1.7 | 0 | .977 | .736 |
| Planned VD (n=64) | 1.3 | 1.1 | 1.0 | 1.8 | 1.5 | .627 | .817 |
| Cesarean Delivery (n=34) | 1.7 | 1.5 | 1.7 | 2.2 | 4.4 | .988 | .777 |
| Vaginal Delivery (n=47) | 1.4 | 1.2 | 1.0 | 1.6 | 0 | .458 | .652 |
| Indicated (n=929) | 3.9 | 1.7 | 1.6 | 1.9 | 1.7 | <.001 | .611 |
| Planned CD (n=352) | 4.8 | 2.1 | 1.8 | 2.6 | 1.9 | <.001 | .406 |
| Planned VD (n=577) | 3.5 | 1.4 | 1.5 | 1.8 | 1.7 | <.001 | .846 |
| Cesarean Delivery (n=595) | 4.7 | 2.1 | 2.0 | 2.8 | 2.8 | <.001 | .751 |
| Vaginal Delivery (n=334) | 3.2 | 1.3 | 1.2 | 1.2 | 1.2 | <.001 | .650 |
| No recorded indication (n=308) | 2.4 | 1.3 | 0.7 | 1.2 | 0 | <.001 | .004 |
| Planned CD (n=33) | 5.0 | 1.4 | 0.7 | 1.9 | 0 | <.001 | .194 |
| Planned VD (n=275) | 2.0 | 1.2 | 0.7 | 1.2 | 0 | <.001 | .001 |
| Cesarean Delivery (n=93) | 5.2 | 1.1 | 1.4 | 2.1 | 0 | <.001 | .388 |
| Vaginal delivery (n=215) | 1.7 | 1.3 | 0.6 | 1.0 | 0 | <.001 | <.001 |
CD, Cesarean delivery; NICU, Neonatal intensive care unit; VD, Vaginal delivery
Respiratory morbidity included neonates admitted to the NICU with any of the following: oxygen therapy with nasal cannula, continuous positive airway pressure, bilevel positive airway pressure, ventilator use, diagnosis of respiratory distress syndrome, hyaline membrane disease, pneumonia, apnea and bradycardia, pulmonary hypertension, pneumothorax, meconium aspiration, or pulmonary hypoplasia.
Fetal anomalies (n=11,559), antepartum stillbirth prior to onset of labor (n=228), and deliveries associated with both fetal anomalies and stillbirth (n=7) excluded from analysis.
P-values based on generalized linear models (GLMs) with generalized estimating equations (GEE) and contrast statements to calculate for significant differences between individual weeks of gestation (e.g. 37 versus 39 and 38 versus 39 weeks).
Row heading number is number of neonates with respiratory morbidity among deliveries with that precursor and mode of delivery.
The greatest decrease in sepsis morbidity also occurred between 37 and 38 weeks with the nadir between 38 and 39 weeks for spontaneous labor and indicated deliveries (P<.001) (Figure 1, panel b). Birth trauma rates were lowest at 37 and 38 weeks for indicated and no recorded indication and increased until 41 weeks gestation (P<.001) (Figure 1, Panel c). Birth trauma rates did not differ across gestational age for spontaneous labor (P=.528) or PROM (P=.011). Rates of HIE, asphyxia, or seizures tended to be lowest at 38 and 39 weeks of gestation, but were not significantly different between early and full term birth for any precursor (P=.022–.558) (Figure 1, Panel d).
Stillbirth (antepartum fetal deaths >23 weeks of gestation) and perinatal mortality (stillbirths and neonatal deaths prior to discharge) rates were calculated per number of ongoing pregnancies reaching a given gestational week. The stillbirth and perinatal mortality rates were as follows: 37 weeks: 0.035% and 0.05%; 38 weeks: 0.034% and 0.06%; 39 weeks: 0.035% and 0.06%; 40 weeks: 0.07% and 0.12%; and 41 weeks: 0.11% and 0.17%, respectively, although rates were not significantly different across weeks (P=.942 for stillbirth and P=.927 for perinatal mortality.)
In order to understand the balance between the risk of severe neonatal respiratory morbidity and the risk of stillbirth with early term delivery, we calculated how many additional cases of severe respiratory morbidity requiring NICU admission would occur in order to prevent one stillbirth. If all women who delivered ≥ 39 weeks had been delivered at 38 weeks’ gestation instead, there would have been an estimated 17 additional cases of serious respiratory morbidity to prevent one stillbirth.
Comment
Early term delivery at 37 weeks of gestation was associated with a significant increase in neonatal morbidity compared to 39 weeks of gestation. In contrast, neonatal morbidities for deliveries at 38 versus 39 weeks were generally not significantly increased, except for a 2.6% higher NICU admission rate for pregnancies complicated by gestational diabetes and a 0.6% increase in serious respiratory morbidity for deliveries with no recorded indication. Our results demonstrate that the increased neonatal morbidity associated with the early term period could not be explained solely by the underlying conditions leading to delivery prior to 39 weeks as deliveries with no recorded indication and those presenting in spontaneous labor also had increased neonatal morbidity at 37 weeks’ gestation compared to those at 39 weeks’ gestation. Importantly, in planned cesarean deliveries for otherwise healthy pregnancies with no recorded indication, respiratory morbidity was lowest at 39 weeks of gestation.
Previous studies examining neonatal outcomes at 37 weeks’ gestation and later with information on conditions leading to delivery are limited. In a study of 27,514 women in Norway at 37 weeks’ gestation and beyond, neonatal morbidity (reflected in the 5 minute Apgar score and pH less than 7.10) had a U shaped distribution, with lowest rates at 39 weeks of gestation and highest postterm. However, that study lacked information on the specific indications for induction.20 Similarly, using U.S. National Center for Health Statistics live birth–infant death certificate data, rates of low 5-minute Apgar score and mechanical ventilation demonstrated a U-shaped relation across term gestational age.21 The same U-shaped pattern was found for women presenting in spontaneous labor without any medical problems or pregnancy complications as recorded on the birth certificate but neonatal morbidity among different indications for delivery could not be compared as the indication for delivery is not included in U.S. birth records.21
While neonatal morbidity was lower during the full term period, benefits of delivery during the full term period must be weighed against the risk of stillbirth. In another study using infant death data from the National Center for Health Statistics, Mandujano et al22 observed that at 38 weeks of gestation, the number of stillbirths for pregnancies remaining undelivered exceeds the number of neonatal deaths caused by delivery of all subjects by 38 weeks. In our study, the difference in neonatal morbidity between 38 and 39 weeks was not statistically significant for most precursors. Furthermore, stillbirth rates did not differ across gestational age in our cohort but our study was cross sectional in nature and the rate of stillbirth was very low. Longitudinal data is necessary to determine whether the optimal balance of neonatal morbidity versus risk of stillbirth and perinatal mortality is 38 or 39 weeks’ gestation.
Our results should be interpreted with caution, as women with more severe disease were more likely to be delivered earlier which could have contributed to increased neonatal morbidity within our indicated group. We also used pregnancy complications documented in the medical record as precursors for delivery, although these conditions may not have been the actual indication for delivery. Other studies from the CSL support the notion that deliveries with no recorded indication were most likely elective, but we could not determine the true incidence of elective delivery.1,23
The major strength of our study was the ability to analyze the specific conditions leading to delivery which enabled us to determine that the increase in neonatal morbidity was due to earlier delivery within the term period. We also excluded stillbirth and fetal anomalies from the neonatal morbidity analysis in order to focus on delivery precursors for which neonatal morbidity could be affected by timing of delivery. Other strengths include use of electronic medical records instead of vital statistics data with more detailed information known about the conditions associated with delivery and inclusion of a large diverse cohort of deliveries more representative of national obstetric practice in the United States.
Neonatal morbidity was lowest at or beyond 39 weeks gestational age and was significantly lower compared to 37 weeks’ gestation; the differences between 38 and 39 weeks were less clear. Information on neonatal outcomes based on the conditions leading to delivery is useful for patient counseling when discussing the risks and benefits of early term delivery. For uncomplicated singleton pregnancies, our data support the recent American College of Obstetrics & Gynecology Committee Opinion of waiting until 39 weeks’ gestation for delivery as there was clearly increased neonatal morbidity during the early term period.14 Given the large percentage of indicated deliveries at 37 and 38 weeks, prospective data is urgently needed to determine the optimal timing of delivery for common pregnancy complications.
Acknowledgment
This work was supported by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health (contract number HHSN267200603425C). Institutions involved in the Consortium include, in alphabetical order: Baystate Medical Center, Springfield, MA; Cedars-Sinai Medical Center Burnes Allen Research Center, Los Angeles, CA; Christiana Care Health System, Newark, DE; Georgetown University Hospital, MedStar Health, Washington, DC; Indiana University Clarian Health, Indianapolis, IN; Intermountain Healthcare and the University of Utah, Salt Lake City, Utah; Maimonides Medical Center, Brooklyn, NY; MetroHealth Medical Center, Cleveland, OH.; Summa Health System, Akron City Hospital, Akron, OH; The EMMES Corporation, Rockville MD (Data Coordinating Center); University of Illinois at Chicago, Chicago, IL; University of Miami, Miami, FL; and University of Texas Health Science Center at Houston, Houston, Texas. The named authors alone are responsible for the views expressed in this manuscript, which does not necessarily represent the decisions or the stated policy of the NICHD.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest statement: The authors report no conflicts of interest.
References
- 1.Laughon SK, Reddy UM, Sun L, Zhang J. Precursors for Late Preterm Birth in Singleton Gestations. Obstet & Gynecol. 2010;116:1047–1055. doi: 10.1097/AOG.0b013e3181f73f97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Melamed N, Klinger G, Tenenbaum-Gavish K, et al. Short Term Neonatal Outcome in Low-Risk, Spontaneous, Singleton, Late Preterm Deliveries. Obstet Gynecol. 2009;114:253–260. doi: 10.1097/AOG.0b013e3181af6931. [DOI] [PubMed] [Google Scholar]
- 3.Catalano PM, Sacks DA. Timing of Indicated Late Preterm and Early-Term Birth in Chronic Medical Complications: Diabetes. Semin Perinatol. 2011;35:297–301. doi: 10.1053/j.semperi.2011.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hutcheon JA, Lisonkova S, Magee LA, et al. Optimal Timing of Delivery in Pregnancies with Pre-existing Hypertension. BJOG. 2011;118:49–54. doi: 10.1111/j.1471-0528.2010.02754.x. [DOI] [PubMed] [Google Scholar]
- 5.Engle WA. Morbidity and Mortality in Late Preterm and Early Term Newborns: A Continuum. Clin perinatol. 2011;38:493–516. doi: 10.1016/j.clp.2011.06.009. [DOI] [PubMed] [Google Scholar]
- 6.Spong C, Mercer B, D’Alton M, Kilpatrick S, Blackwell S, Saade George. Timing of Indicated Late-Preterm and Early-Term Birth. Obstetrics and Gynecology. 2011;118:323–333. doi: 10.1097/AOG.0b013e3182255999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reddy UM, Bettegowda VR, Dias T, et al. Term Pregnancy: A Period of Heterogeneous Risk for Infant Mortality. Ostet Gynecol. 2011;117:1279–1287. doi: 10.1097/AOG.0b013e3182179e28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hibbard JU, Wilkins I, Sun L, et al. Consortium on Safe Labor, Respiratory Morbidity in Late Preterm Births. JAMA. 2010;304:419–425. doi: 10.1001/jama.2010.1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hourani M, Ziede F, Rajab M. Timing of Planned Caesarean Section and the Morbidities of the Newborn. North Am J Med Sci. 2011;3:465–468. doi: 10.4297/najms.2011.3465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.De Luca R, Boulvain M, Irion O, Berner M, Pfister RE. Incidence of Early Neonatal Mortality and Morbidity After Late-Preterm and Term Cesarean Delivery. Pediatrics. 2009;123:e1064. doi: 10.1542/peds.2008-2407. [DOI] [PubMed] [Google Scholar]
- 11.Moster D, Wilcox AJ, Vollset SE, et al. Cerebral Palsey among Term and Postterm Births. J Am Med Assoc. 2010;304:976–982. doi: 10.1001/jama.2010.1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boyle E, Pulsen G, Field D, et al. Effects of Gestational Age at Birth on Health Outcomes at 3 and 5 years of age: Population Based Cohort Study. BMJ. 2012;344:c869. doi: 10.1136/bmj.e896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fleischman AR, Oinuma M, Clark SL. Rethinking the Definition of “Term Pregnancy”. Obstet Gynecol. 2010;116:136–139. doi: 10.1097/AOG.0b013e3181e24f28. [DOI] [PubMed] [Google Scholar]
- 14.Nonmedically Indicated Early-Term Deliveries. Committee Opinion No. 561. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2013;121:911–915. doi: 10.1097/01.AOG.0000428649.57622.a7. [DOI] [PubMed] [Google Scholar]
- 15.Martin JA, Hamilton BE, et al. National Vital Stat Rep. 2010;61:1–100. [PubMed] [Google Scholar]
- 16.Wilmink FA, Hukkelhoven CW, Lunshof S, et al. Neonatal Outcome Following Elective Cearean Section Beyond 37 Weeks of Gestation: a 7 year retrospective analysis of a national registry. Am J Obstet Gynecol. 2010;202:250, e1–e8. doi: 10.1016/j.ajog.2010.01.052. [DOI] [PubMed] [Google Scholar]
- 17.Tita AT, Landon MB, Spong CY, et al. Eunice Kennedy Schriver NICHD Maternal-Fetal-Medicine Units Network. Timing of Elective Repeat Cesarean Delivery at Term and Neonatal Outcomes. N Engl J Med. 2009;260:111–120. doi: 10.1056/NEJMoa0803267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang J, Troendle J, Reddy UM, Laughon SK, Branch DW, Burkman R, et al. Contemporary Cesarean Delivery Practice in the United States. Am J Obstet Gynecol. 2010 Aug 11; doi: 10.1016/j.ajog.2010.06.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Many A, Helpman L, Vilnai Y, Kupfermic M, Lessing J, Dollberg S. Neonatal Respiratory Morbidity after Elective Cesarean Section. J Matern Fetal Neonatal Med. 2006;19(2):75–78. doi: 10.1080/14767050500333868. [DOI] [PubMed] [Google Scholar]
- 20.Heimstad R, Romundstad PR, Eik-Nes SH, Salvesen KA. Outcomes of Pregnancy Beyond 37 Weeks of Gestation. Obstet & Gynecol. 2006;108(3):500–508. doi: 10.1097/01.AOG.0000227783.65800.0f. [DOI] [PubMed] [Google Scholar]
- 21.Zhang X, Kramer MS. Variations in Mortality and Morbidity by Gestational Age Among Infants Born at Term. J Pediatr. 2009;154(3):358–362. doi: 10.1016/j.jpeds.2008.09.013. [DOI] [PubMed] [Google Scholar]
- 22.Mandujano A, Waters TP, Myers SA. The Risk of Fetal Death: Current Concepts of Best Gestational Age for Delivery. Am J Obstet Gynecol. 2012;207:207e1–207e8. doi: 10.1016/j.ajog.2012.12.005. [DOI] [PubMed] [Google Scholar]
- 23.Holland MG, Refuerzo JS, Ramin SM, Saade GR, Blackwell SC. Late Preterm Birth: How Often is it Avoidable? Am J Obstet Gynecol. 2009;201:404e1–404e4. doi: 10.1016/j.ajog.2009.06.066. [DOI] [PubMed] [Google Scholar]