Abstract
Objective
We examined the association between caregiver health literacy and the likelihood of a non-urgent emergency department (ED) visit in children presenting for fever.
Methods
This cross-sectional study used the Newest Vital Sign to assess the health literacy of caregivers accompanying children with fever to the ED. Visit urgency was determined by resources utilized during the ED visit. Findings were stratified by race and child age. Chi-square and logistic regression analysis controlling for race were conducted to determine the association between low health literacy and ED visit urgency.
Results
299 caregivers completed study materials. 39% of ED visits for fever were non-urgent and 63% of caregivers had low health literacy. Low health literacy was associated with a higher proportion of non-urgent ED visits for fever (44% vs. 31%, OR 1.8, 95% CI 1.1, 2.9). Low health literacy was associated with higher odds of a non-urgent visit in white and Hispanic caregivers, but not black caregivers. In regression analysis, children ≥ 2 years old had higher odds of a non-urgent visit if caregivers had low health literacy (aOR 2.0; 95% CI 1.1, 4.1); this relationship did not hold for children < 2 years (aOR 0.8; 95% CI 0.4, 1.8).
Conclusions
Nearly two-thirds of caregivers with their child in the ED for fever have low health literacy. Caregiver low health literacy is associated with non-urgent ED utilization for fever in children over 2 years of age. Future interventions could target health literacy skills regarding fever in caregivers of children ≥ 2 years.
Keywords: Health literacy, utilization, emergency service, hospital, health services accessibility, nonurgent emergency care use, infant, child, preschool, child
INTRODUCTION
A significant national problem, low health literacy is found in over half of caregivers presenting to the emergency department (ED) with their child.1,2 Adults with low health literacy lack the skills in understanding disease process, care knowledge, and health related decision-making.3 Specific to ED use, adults with low health literacy have poor health system navigation leading to difficulty accessing the health system.3 This may be particularly problematic for parents with low health literacy when their child has an acute illness. In a previous study, we found children of caregivers with low health literacy have higher odds of a non-urgent visit.1 In particular, children without a chronic illness have three times the odds of a non-urgent visit if the caregiver has low health literacy. As suggested by previous research,1,4 times when children require more than usual care, such as an acute illness (e.g. gastroenteritis, viral upper respiratory infection, or fever), in otherwise healthy children prompts non-urgent ED visits by caregivers with low health literacy. However, no previous study has addressed a specific acute disease state, such as fever, to understand how health literacy impacts non-urgent ED use.
A lack of health literacy skills, specifically in the setting of a child with fever, could lead to more non-urgent ED visits given the history of “fever phobia” described in caregivers of children.5 Fever is fear provoking to parents with common misperception of the danger of fever (e.g. death or brain damage) creating the concept of “fever phobia.”5–7 Fever represents a common self-limited illness, but requires caregivers to assess and understand the significance of their child’s temperature and treat the fever correctly through dosing antipyretic medications, both a difficulty for caregivers with low health literacy.3,8–10 Low educational attainment is related to increased ED use for fever, supporting that low health literacy may increase non-urgent visits for fever.7
We examined the relationship between low health literacy and non-urgent ED use in caregivers of children presenting to the ED for fever. We hypothesized that in caregivers with low health literacy, children presenting to the ED for fever would be more likely to be classified as non-urgent.
METHODS
Study Participants
This cross-sectional study assessed caregivers accompanying children 57-days to 12-years-old with a complaint of fever presenting to the pediatric ED. Research assistants (RAs) enrolled patients during two periods, 8 summer weeks (June-July 2011, 80 shifts, 182 participants) and 10 winter weeks (January-March 2012, 32 shifts, 134 participants), to account for seasonal variation of pediatric illness. Subjects were excluded if they previously completed the study, did not speak English or Spanish, if the child was in acute distress (e.g., highest acuity triage level), or if the child had a condition for which fever is always urgent and testing is required (e.g., central line, neutropenic condition, sickle cell disease, or infant < 57 days11). We enrolled participants separately from our previous study.1 IRB approval was obtained.
Trained RAs enrolled consecutive subjects during four hour pre-defined study blocks during daytime, evening, and weekend hours. The RAs attempted to approach all caregivers with children presenting with complaint of fever during the enrollment period. After verbal consent was obtained using a script written at the 5th grade level, the RAs orally administered the Newest Vital Sign12 to assess health literacy and the Children with Special Health Care Needs13 questionnaire to determine child chronic illness status. Caregivers completed a self-administered survey of sociodemographic information.
Measures
Health Literacy
The Newest Vital Sign (NVS) is a validated six-question test administered to assess health literacy and numeracy as a composite score.12 The RA gave the caregiver a nutrition facts label to answer health related questions including performance of calculations. Resulting NVS scores were dichotomized into low (0–4 questions correct) and adequate (5–6 questions correct) health literacy categories using the threshold from a previous study.1
Non-Urgent Visit Classification Based on Resources Used
The urgency of the ED visit was classified based on resources used during the ED visit,14,15 a method used in other studies of ED utilization.16,17 The RAs performed a blinded chart review to determine the resources used during the ED visit. Visits were considered urgent if the child utilized any diagnostic testing (excluded rapid strep and viral antigen swabs), radiologic studies, administration of IV fluids, or provision of any medication (excluding oral antibiotics and over-the-counter medications).14 All other visits were considered non-urgent. Fever was not a criterion for determining visit urgency.
Statistical analyses
We performed chi-square analysis to compare demographic characteristics and health literacy with urgency of the ED visit. We stratified analyses by child age as planned a priori due to a known higher non-urgent ED use in children < 2 years.18 We performed logistic regression, adjusted for race, for the age stratification by including a combined health literacy (low or adequate) and child age (< 2, ≥ 2 years) variable using two regression models to obtain the specific referent group. Additionally, we stratified findings by race to further understand the findings in bivariate analysis. Study data were collected and managed using REDCap electronic data capture tools. SAS software, Version 9.3 (SAS Institute, Inc, Carey NC) was used for all statistical analyses.
A sample size of 283 caregiver/child pairs would detect a minimum difference of 0.15 in non-urgent ED visit proportion between adequate and low health literacy with an α of 0.05 and power of 0.80.
RESULTS
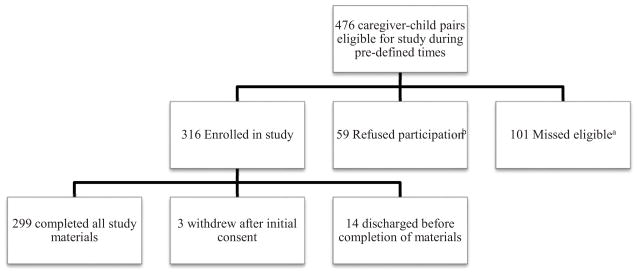
A total of 476 caregiver/child pairs were eligible for enrollment, 316 consented (66%), and 299 completed all study materials (Figure 1). Children had a median age of 2.0 years and 34% had a chronic illness (Table 1). Sixty-three percent of the caregivers had low health literacy (95% CI 58–68%). Low health literacy was associated with lower caregiver educational attainment, minority race/ethnicity, and a higher proportion of publically insured children (p < 0.01 for all variables).
Figure 1.
Patient flow through study
a. Patients were unable to be recruited due to concurrent enrollment of other caregivers. The missed eligible patients were younger (p=0.01) and triaged as a lower acuity (p=0.02).
b. The caregivers that refused participation did not differ from study participants in age (p=0.9) or triage level (p=0.1).
Table 1.
Caregiver and Child Characte
| % (n) | |
|---|---|
| Caregiver | n=299 |
| Age in years (median; range) | (30.0, 18–69) |
| Female gender | 87.2 (258) |
| Foreign born | 16.4 (48) |
| Ethnicity/race | |
| White | 34.6 (101) |
| Black | 42.8 (125) |
| Hispanic | 14.4 (42) |
| Other | 8.2 (24) |
| Education | |
| Less than HS | 14.6 (43) |
| Graduated HS | 27.0 (79) |
| 1–4 years college | 31.4 (92) |
| ≥ College degree | 27.0 (79) |
| Child | |
| Age in years (median; range) | (2.0; 0.2–12) |
| < 2 years | 42.3 (124) |
| ≥ 2 years | 57.7 (169) |
| Insurance | |
| Private | 28.2 (81) |
| Public | 70.4 (202) |
| None | 1.4 (4) |
| Usual source of care | |
| Primary care provider | 94.6 (280) |
| Emergency department | 4.7 (14) |
| None | 0.7 (2) |
| Child has Chronic Illnessa | 34.7 (103) |
Children with Special Health Care Needs Screener for chronic illness.
Non-Urgent ED Visits
Analysis of resources utilized showed that 39% of the ED visits for fever were non-urgent. Low health literacy was associated with a higher proportion of non-urgent ED visits (44% vs. 31%; OR 1.8; 95% CI 1.1, 2.9). Caregiver black race and public insurance were also related to non-urgent ED use in unadjusted analyses (Table 2).
Table 2.
Caregiver/Child Characteristics and Relationship With Non-urgent ED Visit
| Variable | Percent Non-urgent ED visit | Odds Ratio of Non-Urgent ED Visit (95% Confidence Interval) |
|---|---|---|
| Caregiver | ||
| Health Literacy | ||
| Adequate | 30.9 | 1.0 |
| Low | 43.9 | 1.8 (1.1, 2.9) |
| Ethnicity/race | ||
| White | 28.7 | 1.0 |
| Black | 48.0 | 2.3 (1.3, 4.0) |
| Hispanic | 33.3 | 1.2 (0.6, 2.7) |
| Other | 45.8 | 2.1 (0.8, 5.2) |
| Child | ||
| Child insurancea | ||
| Private | 29.6 | 1.0 |
| Public | 43.1 | 1.8 (1.03, 3.1) |
| Chronic illnessb | ||
| Yes | 29.6 | 1.0 |
| No | 43.1 | 1.6 (0.9, 2.6) |
| Child age | ||
| < 2 years of age | 38.9 | 1.0 |
| ≥ 2 years of age | 41.1 | 1.04 (0.9, 1.3) |
“No insurance” group excluded from this analysis for low count.
Children with Special Health Care Needs Screener for chronic illness.
Effect of Low Health Literacy on Non-Urgent ED Visits Varies by Child Age
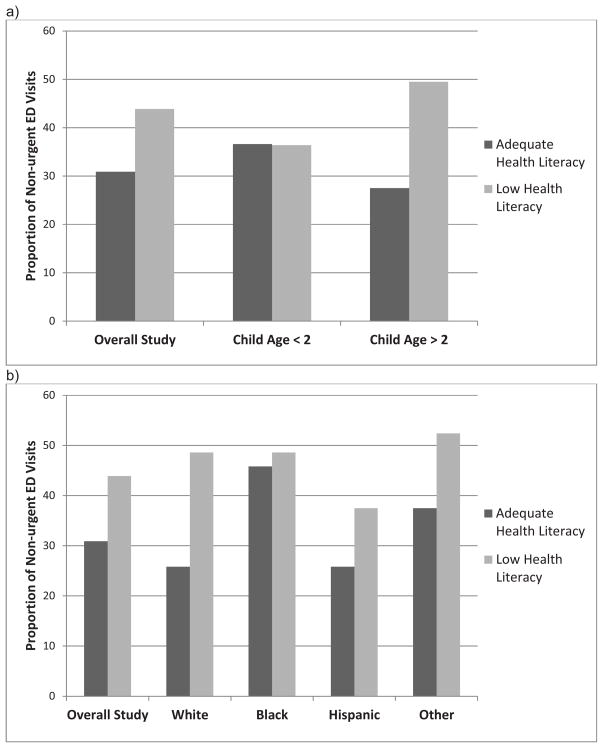
The proportion of non-urgent ED visits in children of caregivers with low health literacy differed by age (Figure 2a). Caregiver low health literacy was associated with a higher proportion of non-urgent ED visits in children ≥ 2 years (OR 2.2; 95% CI 1.2, 3.8) but not in children < 2 years (OR 1.0; 95% CI 0.4, 2.2).
Figure 2.
Health Literacy and Proportion of Non-Urgent ED Visits for Fever Stratified by (a) Child Age and (b) Caregiver Race/Ethnicity
Effect of Low Health Literacy on Non-Urgent ED Visits Varies by Race/Ethnicity
We found a higher proportion of non-urgent ED visits associated with low health literacy in specific racial/ethnic groups (Figure 2b). The proportion of non-urgent ED visits was higher in caregivers with low health literacy of white race (OR 1.7, 95% CI 0.8, 3.9), Hispanic ethnicity (OR 1.8, 95% CI 0.4, 7.7), or “other” race (OR 1.8, 95% 0.3, 9.7), though not statistically significant. Among black caregivers, health literacy was not related to increased odds of a non-urgent ED visit (OR 1.1; 95% CI 0.5, 2.7) with no difference considering private (OR 1.2; 95% CI 0.2, 9.0) or public insurance (OR 1.2; 95% CI 0.4, 3.0).
Child Age, Race, Health Literacy, and Non-urgent ED Visits
Given that the effect of health literacy varies by age and racial groups, we conducted a multivariate analysis. In a model adjusted for race, low health literacy was significantly related to a non-urgent visit in children ≥ 2 years (aOR 2.0; 95% CI 1.1, 4.1) but not in children < 2 years of age (aOR 0.8; 95% CI 0.4, 1.8). The differences found by age are not due to increased testing in children < 2 years. The urgency of the ED visit was the same whether the child was < 2 (38.9% non-urgent) or ≥ 2 years (41.1% non-urgent) (p=0.69).
DISCUSSION
Fever presents a unique set of challenges to caregivers with limited health literacy skills. Having a child with fever requires caregivers to assess a numeric value and recognize and adequately treat symptoms. Adults with low health literacy have poor understanding of illness8,19,20 and are known to dose antipyretic medications incorrectly, 9,10 leading to poor treatment of fever at home. Lack of health system navigational skills and hesitance to seek information about illness, could lead to higher ED use.3,21 Caregivers may seek non-urgent ED care mistakenly believing their child needs urgent treatment,22–24 representing a poor understanding of illness. We previously found that caregivers with low health literacy are likely to have health literacy skills challenged during an acute illness leading to care seeking in the ED.1 This study adds the understanding that low health literacy is associated with more non-urgent ED visits for fever in children ≥ 2 years of age.
The relationship between health literacy and non-urgent ED use appears to be affected by child age. As a child ages and the caregiver with adequate health literacy gains more experience, knowledge, or feels more comfortable with fever, the limitation of low health literacy is demonstrated in the higher number of non-urgent ED visits. Conversely, caregivers of younger children seek care equally whether possessing low or adequate health literacy. One of the likely contributors to this age difference is “Fever phobia.” Fever phobia exists across all ranges of socioeconomic status and educational levels, and potentially, may have outweighed the effect of low health literacy on non-urgent ED use in the younger patients.5 Given that a chief complaint of fever is found in 20% of ED patients, ED providers need to be cognizant of fever phobia in all caregivers, and educate all parents using strategies to maximize understanding for all literacy levels. Caregivers of children ≥ 2 years old may respond well to health literacy-related interventions regarding fever. However, if targeting caregivers of children < 2 years, interventions may require alternative strategies.
As in our previous study, this study suggests that low health literacy is related to non-urgent visits among white and Hispanic caregivers. This is statistically limited given the small subgroups. The use of the ED for non-urgent conditions for fever does not vary by health literacy in caregivers of black race. This may be partially explained by past findings of increased fever phobia among caregivers of black race25 or other cultural differences that are not well studied. In order for educational interventions for fever to be effective in black caregivers, we may need to further understand the cultural beliefs about fever and give culturally sensitive education materials.
Limitations
Selection bias may have occurred if caregivers with low health literacy refused participation due to the consent process. This possibility was mitigated through a shortened, low literacy consent procedure using verbal consent. Due to concurrent enrollment, we missed 20% of eligible patients, likely because these patients were lower acuity and discharged from the ED quickly. We did not collect information about fever phobia or reasons for seeking care and therefore our conclusions about fever phobia are based on previous literature. We also did not collect information on referral from a primary care doctor, which would have influenced care-seeking by these families, however, this would likely not have changed our results given healthcare navigation varies by health literacy. Finally, we did not enroll children in whom fever would always be an urgent visit (febrile neonates, etc) as these children should seek care regardless of literacy level.
Conclusions
Nearly two-thirds of the caregivers presenting to the ED with a child for fever have low health literacy. Low caregiver health literacy is associated with non-urgent ED use for fever in children ≥ 2 years of age. Clinical providers need to be cognizant of the communication challenge when educating caregivers of all health literacy levels. Providers should employ easy to understand language to describe the child’s illness and treatment plans for fever. To be most effective, future interventions targeting health literacy skills regarding fever care could target caregivers of children > age 2.
What’s new.
Over two-thirds of caregivers with their child in the ED for fever have low health literacy which is related to higher odds of a non-urgent visit in children ≥ 2 years. We found that health literacy is an important factor in care-seeking behavior for mild acute illnesses such as fever.
Acknowledgments
Funding Source: This publication was partially supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Number 8UL1TR000055. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
The authors would like to acknowledge Que Xiong, Itohan Otasowie, and Mark Nimmer for their effort in data collection. This publication was partially supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Number 8UL1TR000055 with effort including study design, analysis and interpretation of the data.
Abbreviations
- ED
Emergency department
- CSHCN
Children With Special Health Care Needs
- NVS
Newest Vital Sign
- OR
Odds Ratio
- AOR
Adjusted Odds Ratio
Footnotes
Conflicts of Interest: No author has conflicts of interest and there are no corporate sponsors of this research.
Contributor’s Statement:
Andrea K. Morrison: Dr. Morrison conceptualized and designed the study, submitted the IRB, designed the data collection instruments, trained research assistants, coordinated and supervised data collection, participated in acquisition of the data, carried out the initial data analysis and interpretation, drafted the initial manuscript, and approved the final manuscript as submitted.
Ruben Chanmugathas: Mr. Chanmugathas participated in acquisition of the data, participated in initial drafting of the manuscript, critically reviewed the manuscript, and approved the final manuscript as submitted.
Marilyn M. Schapira: Dr. Schapira participated in study conceptualization and design, critically reviewed the manuscript, and approved the final manuscript as submitted.
Marc H. Gorelick: Dr. Gorelick participated in study conceptualization and design, critically reviewed the manuscript, and approved the final manuscript as submitted.
Raymond G. Hoffmann: Dr. Hoffmann participated in study conceptualization and design, aided with data analysis by providing statistical expertise, critically reviewed the manuscript, and approved the final manuscript as submitted.
David C. Brousseau: Dr. Brousseau participated in study conceptualization and design, aided with data analysis, critically reviewed the manuscript, and approved the final manuscript as submitted.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Morrison AK, Schapira MM, Gorelick MH, Hoffmann RG, Brousseau DC. Low caregiver health literacy is associated with higher pediatric emergency department use and non-urgent visits. Acad Pediatr. 2014;14(3):309–14. doi: 10.1016/j.acap.2014.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Morrison AK, Myrvik MP, Brousseau DC, Hoffmann RG, Stanley RM. The relationship between parent health literacy and pediatric emergency department utilization: A systematic review. Acad Pediatr. 2013;13(5):421–429. doi: 10.1016/j.acap.2013.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nielsen-Bohlman LT, Panzer AM, Kindig DA, editors. Health literacy: A prescription to end confusion. 1. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- 4.Sanders LM, Shaw JS, Guez G, Baur C, Rudd R. Health literacy and child health promotion: Implications for research, clinical care, and public policy. Pediatrics. 2009;124 (Suppl 3):S306–14. doi: 10.1542/peds.2009-1162G. [DOI] [PubMed] [Google Scholar]
- 5.Schmitt BD. Fever phobia: Misconceptions of parents about fevers. Am J Dis Child. 1980;134:176–181. [PubMed] [Google Scholar]
- 6.Baker MD, Monroe KW, King WD, Sorrentino A, Glaeser PW. Effectiveness of fever education in a pediatric emergency department. Pediatr Emerg Care. 2009;25(9):565–568. doi: 10.1097/PEC.0b013e3181b4f64e. [DOI] [PubMed] [Google Scholar]
- 7.Poirier MP, Collins EP, McGuire E. Fever phobia: A survey of caregivers of children seen in a pediatric emergency department. Clinical Pediatrics. 2010;49(6):530–534. doi: 10.1177/0009922809355312. [DOI] [PubMed] [Google Scholar]
- 8.Lokker N, Sanders L, Perrin EM, et al. Parental misinterpretations of over-the-counter pediatric cough and cold medication labels. Pediatrics. 2009;123(6):1464–1471. doi: 10.1542/peds.2008-0854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yin HS, Dreyer BP, Foltin G, van Schaick L, Mendelsohn AL. Association of low caregiver health literacy with reported use of nonstandardized dosing instruments and lack of knowledge of weight-based dosing. Ambul Pediatr. 2007;7(4):292–298. doi: 10.1016/j.ambp.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 10.Yin HS, Mendelsohn AL, Wolf MS, et al. Parents’ medication administration errors: Role of dosing instruments and health literacy. Arch Pediatr Adolesc Med. 2010;164(2):181–186. doi: 10.1001/archpediatrics.2009.269. [DOI] [PubMed] [Google Scholar]
- 11.Baker MD, Bell LM, Avner JR. Outpatient management without antibiotics of fever in selected infants. N Engl J Med. 1993;329(20):1437–1441. doi: 10.1056/NEJM199311113292001. [DOI] [PubMed] [Google Scholar]
- 12.Weiss B, Mays M, Martz W, et al. Quick assessment of literacy in primary care: The newest vital sign. Annals of family medicine. 2005;3(6):514. doi: 10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bethell CD, Read D, Stein REK, Blumberg SJ, Wells N, Newacheck PW. Identifying children with special health care needs: Development and evaluation of a short screening instrument. Ambulatory Pediatrics. 2002;2(1):38–48. doi: 10.1367/1539-4409(2002)002<0038:icwshc>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 14.DeAngelis C, Fosarelli P, Duggan AK. Use of the emergency department by children enrolled in a primary care clinic. Pediatr Emerg Care. 1985;1(2):61–65. [PubMed] [Google Scholar]
- 15.Mistry RD, Brousseau DC, Alessandrini EA. Urgency classification methods for emergency department visits: Do they measure up? Pediatr Emerg Care. 2008;24(12):870–874. doi: 10.1097/PEC.0b013e31818fa79d. [DOI] [PubMed] [Google Scholar]
- 16.Mistry RD, Cho CS, Bilker WB, Brousseau DC, Alessandrini EA. Categorizing urgency of infant emergency department visits: Agreement between criteria. Acad Emerg Med. 2006;13(12):1304–1311. doi: 10.1197/j.aem.2006.07.028. [DOI] [PubMed] [Google Scholar]
- 17.Sarver JH, Cydulka RK, Baker DW. Usual source of care and nonurgent emergency department use. Acad Emerg Med. 2002;9(9):916–923. doi: 10.1111/j.1553-2712.2002.tb02193.x. [DOI] [PubMed] [Google Scholar]
- 18.Brousseau DC, Hoffmann RG, Nattinger AB, Flores G, Zhang Y, Gorelick M. Quality of primary care and subsequent pediatric emergency department utilization. Pediatrics. 2007;119(6):1131–1138. doi: 10.1542/peds.2006-3518. [DOI] [PubMed] [Google Scholar]
- 19.DeWalt DA, Hink A. Health literacy and child health outcomes: A systematic review of the literature. Pediatrics. 2009;124 (Suppl 3):S265–74. doi: 10.1542/peds.2009-1162B. [DOI] [PubMed] [Google Scholar]
- 20.Yin HS, Mendelsohn AL, Nagin P, van Schaick L, Cerra ME, Dreyer BP. Use of active ingredient information for low socioeconomic status parents’ decision-making regarding cough and cold medications: Role of health literacy. Acad Pediatr. 2013;13(3):229–235. doi: 10.1016/j.acap.2013.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Trifiletti LB, Shields WC, McDonald EM, Walker AR, Gielen AC. Development of injury prevention materials for people with low literacy skills. Patient Educ Couns. 2006;64(1–3):119–127. doi: 10.1016/j.pec.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 22.Berry A, Brousseau D, Brotanek JM, Tomany-Korman S, Flores G. Why do parents bring children to the emergency department for nonurgent conditions? A qualitative study. Ambul Pediatr. 2008;8(6):360–367. doi: 10.1016/j.ambp.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 23.Fieldston ES, Alpern ER, Nadel FM, Shea JA, Alessandrini EA. A qualitative assessment of reasons for nonurgent visits to the emergency department. Pediatr Emer Care. 2012;28:220–25. doi: 10.1097/PEC.0b013e318248b431. [DOI] [PubMed] [Google Scholar]
- 24.Kubicek K, Liu D, Beaudin C, et al. A profile of nonurgent emergency department use in an urban pediatric hospital. Pediatr Emer Care. 2012;28(10):977–984. doi: 10.1097/PEC.0b013e31826c9aab. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rupe A, Ahlers-Schmidt CR, Wittler R. A comparison of perceptions of fever and fever phobia by ethnicity. Clin Pediatr. 2010;49(2):172–176. doi: 10.1177/0009922809336208. [DOI] [PubMed] [Google Scholar]