Abstract
Objective:
The current study describes sleeping heart rate patterns in an adolescent cohort of Hispanic and Caucasian children over approximately a 5-year period to determine how sex, ethnicity, and body mass index (BMI) contribute to sleeping heart rate patterns over time.
Methods:
Participants were recruited from a large urban school district in the southwest United States as part of the Tucson Children's Assessment of Sleep Apnea Study (TuCASA). Heart rate data was obtained through electrocardiogram (ECG) recordings during in-home polysomnography, approximately 5 years apart. Second-wave cohort data were analyzed to determine how age, sex, ethnicity, physical activity, and BMI contribute to average sleeping heart rates. The same variables were used to investigate how sleeping heart rate patterns change longitudinally from school-age (6–11 years) to adolescence (10–17 years) during sleep.
Results:
Female adolescents had significantly faster average heart rates during sleep. Sleeping heart rate decreased significantly with increasing age in the adolescent cohort. Although the Hispanic group had a statistically significant higher body mass index than Caucasians, there were no significant differences in heart rate observed between ethnicities or in those who were classified as obese (BMI ≥ 95th percentile for age). Longitudinal analysis between the school-aged and adolescent cohort revealed a significant overall decrease in heart rate across a 5-year period.
Conclusions:
Hispanic and Caucasian adolescents experience a similar decrease in sleeping heart rate with age. Female adolescents had significantly faster heart rates than males, and no significant differences were observed between Caucasians and Hispanics, or obese vs. nonobese adolescents.
Citation:
Hedger-Archbold K, Sorensen ST, Goodwin JL, Quan SF. Average heart rates of Hispanic and Caucasian adolescents during sleep: longitudinal analysis from the TuCASA cohort. J Clin Sleep Med 2014;10(9):991-995.
Keywords: adolescents, heart rate, polysomnography
Sleep parameters in adolescents and school-aged children have been increasingly characterized in recent years1; however, despite being regularly recorded during overnight polysomnography (PSG), limited data on normative heart rate patterns during sleep have been reported. There are currently available data for sleeping heart rates in infants2 and school-aged children,3 as well as heart rates during wakefulness in adolescents,4,5 but there remains a paucity of published information regarding adolescent heart rates during sleep. The current study first aimed to describe average heart rates of healthy adolescents during sleep, and to determine the relationships between age, sex, body mass index (BMI), physical activity, and ethnicity (Caucasian/Hispanic) on nocturnal heart rates. Second, the study aimed to determine the changes in sleeping heart rates experienced in a cohort of healthy children over a 5-year time period, and determine if sex, ethnicity, and BMI during school-age years contributed to variability in sleeping heart rates for adolescents.
METHODS
Participants
The Tucson Children's Assessment of Sleep Apnea study (TuCASA) is a longitudinal cohort that has been previously described.6 In brief, the TuCASA cohort includes generally healthy school-aged children who were recruited from a large urban school district in the Southwest United States. With the cooperation of their respective elementary schools, parents of the students were asked to complete a brief screening questionnaire (N = 2,327) and to provide contact information if they wanted to see if their child was eligible for the study. Those who qualified were then studied using a single overnight unattended in-home polysomnography (PSG) along with completion of a questionnaire regarding their sleep habits. TuCASA initially recruited 503 participants (ages 6–11 years) who had their PSGs recorded between the years of 2000 and 2004 (TuCASA 1).
BRIEF SUMMARY
Current Knowledge/Study Rationale: Little is known about heart rate patterns during sleep for adolescents and how these patterns may change over a 5-year period. We aimed to describe and determine the relationships between age, sex, body mass index (BMI), physical activity and ethnicity on nocturnal heart rate patterns in a cohort of healthy adolescents.
Study Impact: No significant differences were found between obese vs. non-obese, Caucasian vs. Hispanic adolescents in nocturnal heart rates, although female adolescents had significantly faster heart rates than males at all time points. Levels of physical activity and fitness may be an important contributor to the observed sex differences in nocturnal heart rate and should be investigated in future work.
Approximately 5 years later, researchers attempted to contact the initial 503 participants and were able to obtain valid in-home PSG recordings with 319 children (TuCASA 2). From this group of 319 children, 163 (51.1%) had valid recorded ECG heart rates during PSG. From this group of 163 children with valid ECG data, 22 were found to have some degree of sleep disordered breathing (SDB), and so were excluded from analyses (SDB was defined as the respiratory disturbance index [RDI] ≥ 1 and associated with > 3% oxygen desaturation7). Two additional outlier cases who had hypertension (142/90 and 134/86, respectively) were also excluded from analyses, yielding a sample size for cross-sectional analyses of N = 139 participants from TuCASA 2 (Figure 1).
Figure 1. Flow Diagram of Participant Selection.
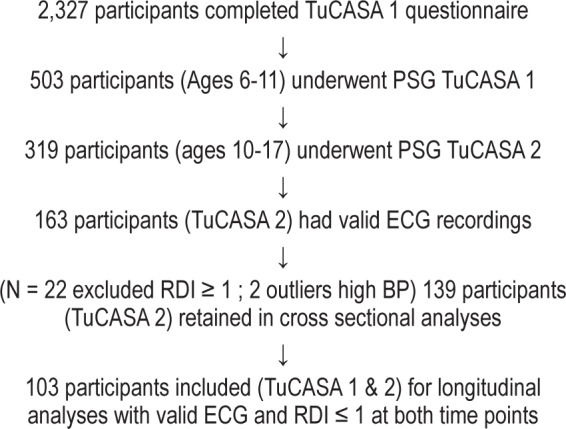
For the purposes of longitudinal analysis, we wanted to determine the change over time from sleeping heart rate from TuCASA 1 to TuCASA 2 PSG. Therefore, to create within subject pairs for analyses, 34 participants with the presence of SDB at TuCASA 1, and 2 participants with insufficient ECG data (< 6 h of HR signal recorded) at TuCASA 1 were excluded. The resulting sample of N = 103 was then used in longitudinal ANOVA analyses.
Average heart rates were calculated from the PSGs and were also characterized by body position (supine and other), REM, and NREM stages.
Polysomnography
On the night of the their baseline and follow-up PSG, a 2-member, mixed-sex team came to the participant's home approximately an hour prior to the child's normal bedtime, as determined by parental report. At this time, informed consent from the parent or guardian, and assent from the child were obtained, as well as anthropometric measures of height, weight, and blood pressure. The single night PSG was recorded on both occasions using a Compumedics PS-2 system (Abbots-ford, Victoria, Australia) with the following channel leads; C3/ A2 and C4/A1 electroencephalogram, right and left electroculogram, bipolar electromyogram, both thoracic and abdominal plethysmography bands, airflow thermistor, nasal pressure cannula, snoring microphone, body position sensor, ambient light sensor, finger pulse oximetry, and ECG. The ECG was recorded using a single bipolar lead sampled at a rate of 64 cycles per second. Sleep staging was scored according to Rechtschaffen and Kales criteria.8 The RDI was defined by the number of apneas and hypopneas per hour of sleep that were also associated with at least 3% oxygen desaturation (RDI > 3%).
Assessment of Physical Activity
As a surrogate for fitness level, the Block Kids Physical Activity Screener was used to assess the children's daily physical activity levels (http://www.nutritionquest.com), which is designed for school-age children aged 8–17 years to complete by themselves. The Screener inquires about frequency and duration of activities in the past week, then computes an estimation of the average amount of total kilocalories (kcals) expended by that child on a daily basis.
Data Analysis
BMI percentiles were determined based on height and weight charts provided online from the Center for Chronic Disease Prevention and Health Promotion.9 Obesity was defined as having a body mass index (BMI) ≥ 95th percentile compared to same aged peers. Mean sleeping heart rates were determined for each stage of sleep and were weighted according to percent time in each sleep stage to obtain an overall average during the entire time spent asleep. Parent reports of sleep behavior the night before and morning after the PSG were used to obtain estimates of the time the adolescent went to bed and the time they awoke in the morning.
Independent sample t-tests were used to determine whether heart rate varied according to sex, ethnicity, physical activity, and BMI during adolescence (TuCASA 2 PSG). Cohen's d was used to measure effect size. t-tests with equal variances not assumed were used to compare Caucasians to Hispanics due to unequal sample sizes. Least square means analysis of variance models were used to control for covariates with age. To determine how heart rate changed from baseline to follow-up for independent variables of gender and ethnicity, a longitudinal analysis was conducted using repeated measures ANOVA. All analyses were conducted using SPSS version 20.0 (IBM, SPSS, Chicago, IL). Data are presented as mean ± SD or percentages as appropriate.
RESULTS
Adolescent Sleeping Heart Rates (TuCASA 2)
Table 1 reports the demographic and sleep variables for the 3 groups of participants. Sleeping heart rates stratified by age and gender are shown in Table 2. Results from the independent sample t-tests within the adolescent group (N = 139) demonstrated that females (N = 69) had significantly faster heart rates (68.2 ± 9.2) than males (63.1 ± 8.5); t137 = −3.36; p = 0.001, d = 0.58 (Table 3). Additionally, Hispanic adolescents (N = 54) had a significantly higher BMI percentile (73.2 ± 24.9) than Caucasians (58.3 ± 30.7); t137 = −2.984; p = 0.002; d = 0.53) (Table 4). While the difference in physical activity levels between males and females was not statistically significant (729.9 ± 729.9 vs. 527.8 ± 442.7; t106.5 = 1.95; p = 0.056, respectively) a trend in difference was noted. There were no significant differences in age or BMI between males and females, and no significant differences in age, physical activity, or average sleeping heart rates between Caucasian and Hispanic adolescents.
Table 1.
Demographic and sleep variables across groups
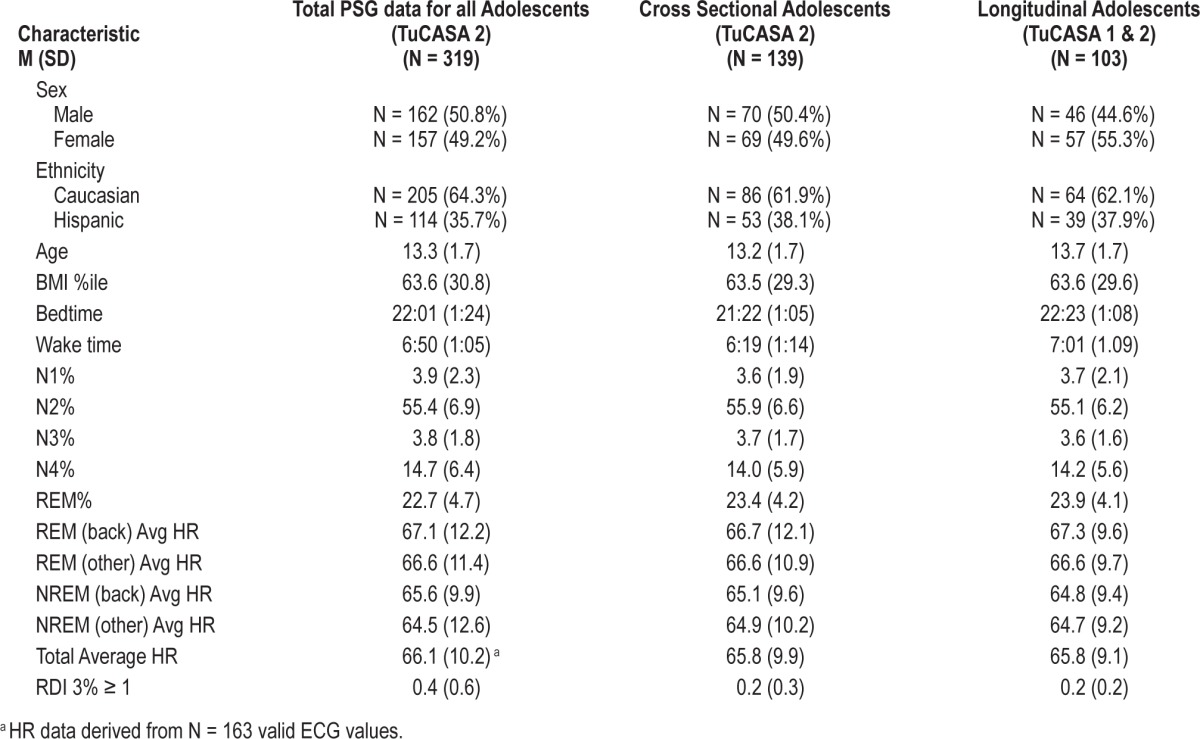
Table 2.
Healthy cross-sectional adolescent cohorts sleeping heart rate according to age and gender (N = 139).
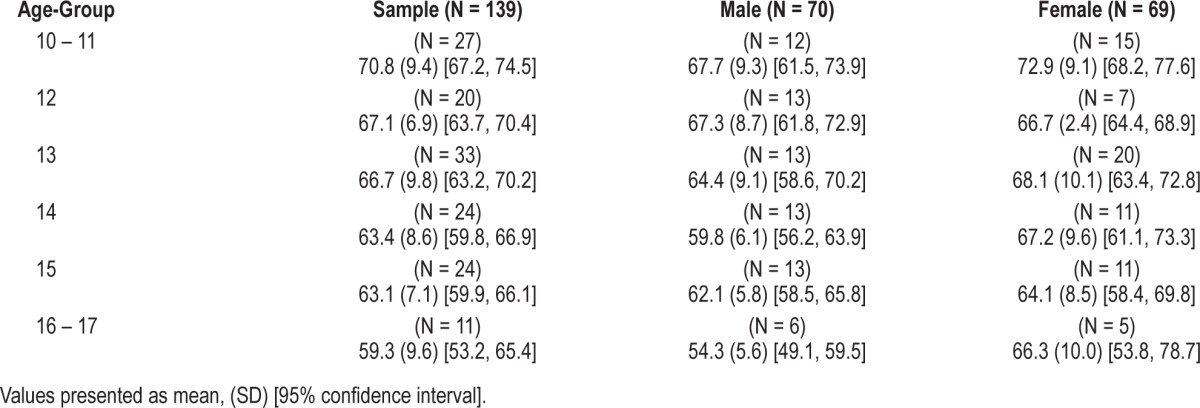
Table 3.
Age, BMI, and heart rate stratified by gender (N = 139)
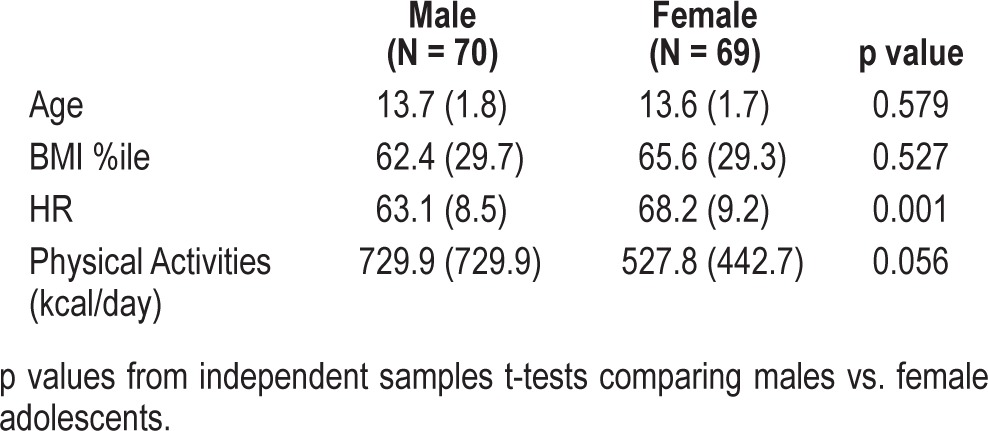
Table 4.
Age, BMI, and heart rate stratified by ethnicity
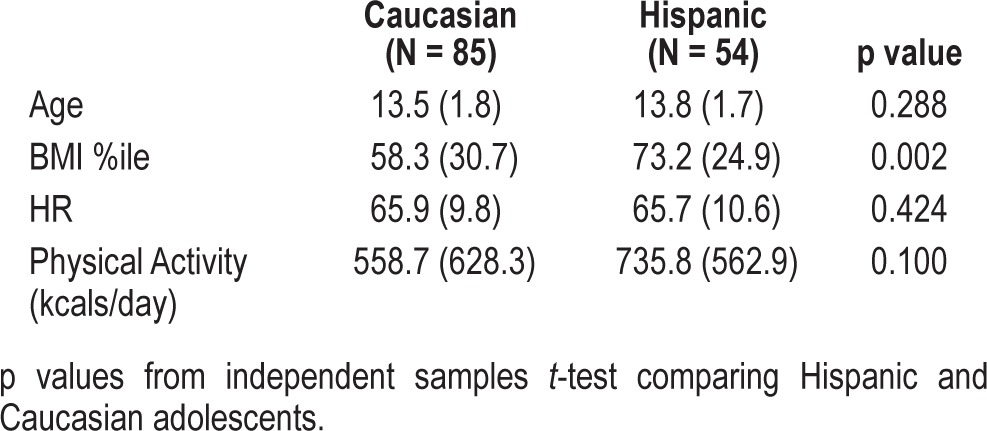
Since no significant differences in average heart rates were observed between the Caucasian and Hispanic groups, both groups were combined in the least square means analysis of variance models. Results from these analysis revealed that overall sample heart rates decreased with age (F = 12.905, p < 0.001) and female adolescents had significantly faster heart rates than males through the adolescent years when controlling for age (F = 14.738, p < 0.001). There were no significant differences observed in average heart rates in adolescents who were classified as obese (N = 26) vs. nonobese (N = 115). A small but significant difference was observed within individuals comparing average heart rates during REM (66.7 ± 9.6) to NREM (65.1 ± 9.3); t136 = 4.447; p < 0.001; d = 0.36. However, when physical activity was entered into the model along with gender, age, and BMI percentile, the difference between male and female nocturnal heart rate was attenuated (66.6 ± 14.4 vs. 63.9 ± 14.3, p = 0.12, respectively), and failed to achieve statistical significance.
Change in Heart Rates 5 Years Later (TuCASA 1 & 2)
Longitudinal analysis of heart rates was conducted on N = 103 participants with an average duration of 4.5 (0.8) (min 2.7, max 7.3) years between PSG studies. Average change in body mass index was an increase of 3.1%. There were no significant relationships found between change in BMI and change in overall heart rate, REM heart rate, or NREM heart rate (p > 0.05). Similarly, no significant relationships were observed between duration of time between time points on any heart rate measure. As a result, neither was entered as a covariate in analysis.
Results from the ANOVA investigating changes in overall heart rate over time revealed a significant decrease between baseline (76.8) and follow-up (65.8) of 11 BPM in overall heart rate (F1, 99 = 92.60, p < 0.001, η2 = 0.48). There were no significant main effects or interactions for gender (p = 0.73) and/or ethnicity (p = 0.07) on change in overall average heart rates. Significant decreases between time points were also observed for average heart rates during REM between baseline (79.1) and follow-up (66.9); F1, 98 = 54.12, p < 0.001, η2 = 0.36. Similar to overall heart rates, there were no main effects or interaction with gender (p = 0.99) and/or ethnicity (p = 0.13). Lastly, changes in average heart rates during NREM sleep also significantly decreased from baseline (74.7) to follow-up (64.8); F1, 99 = 105.6; p < 0.001; η2 = 0.52. Consistent with overall and REM heart rates, there was no main effect observed on gender (p = 0.68); however, a significant main effect was observed on ethnicity (F1, 99 = 4.45, p = 0.04, η2 = 0.04), with Hispanic youth demonstrating an accelerated decrease in NREM heart rate from school-aged years (76.8) to adolescence (64.2) compared to Caucasian youth (73.4 to 65.1).
DISCUSSION
Consistent with sleeping heart rates in school-aged children, Hispanic and Caucasian adolescents ages 10 to 17 years old had sleeping rates that decreased significantly as age increased. Females in this cohort had consistently faster average heart rates than males. On average, healthy female heart rates were approximately 5 beats per minute faster than males, and heart rate decreased with each advancing year during adolescence. There was also a significant difference between average recorded heart rates between sleep stages, with ECG recordings during REM yielding higher rates than NREM. Furthermore, level of fitness appeared to explain some of the differences in heart rate between genders.
Although reports of normative values for heart rate during sleep are rare in the literature, the findings in the current study appear to be consistent with a recently described cohort by Scholle and colleagues investigating healthy German youth of Caucasian ancestry.10 The researchers investigated children and adolescents between the ages of 1 and 18 years old who had no health problems and were free from cardiorespiratory morbidity using a single in-lab nocturnal PSG. Findings from the study highlighted a significant decrease in heart rate during both wakefulness and sleep at each of the age groups studied, and found females to have significantly faster heart rates during sleep. Corroborating findings from our current study, the investigators also found that heart rates during REM were significantly faster than NREM. Our results extend these previous findings by documenting them in a home environment, demonstrating their occurrence in a longitudinal cohort containing Hispanics, and exploring the role of fitness as an explanatory variable.
Compared to waking heart rates, sleeping heart rates observed in Hispanic and Caucasian adolescents in the present study appear to be approximately 15% to 20 % slower than published normative heart rates during wakefulness.4 Similar to our previous study when this cohort was younger, there were no significant differences found between sleeping heart rates in Hispanics and Caucasians; however, it should be noted that this is a finding that does not apply to all ethnic groups, as there is evidence that African American children may have faster heart rates during sleep.3
In contrast to findings in the adult and pediatric literature, obese participants in our study did not have comparably faster heart rates.11 One explanation for this may be due to our sample having a relatively high average BMI compared to equal aged peers. Average BMI observed in our sample was at the 66th percentile, suggesting that even though otherwise healthy, the adolescents in our study were heavier than same-aged peers, and may have had elevated heart rates compared to a more representative sample. Additionally, numerous participants approached and exceeded the 85th percentile classifying them as over-weight9; thus the 95th percentile for classifying obese subjects in our sample may not discriminate differences when applying this clinical cutoff to the groups' average sleeping heart rates.
Resting daytime pulse rate is generally accepted as a marker of underlying physical fitness in children.12 In our study we assessed physical activity using a validated self-administered questionnaire as a surrogate for fitness in our cohort. We found a nonsignificant trend for higher physical activity levels in males than females (p = 0.056) and when included in our multivariate models explained much of the difference in sleeping heart rates between genders. Resting daytime heart rate in adolescents has been shown to be inversely correlated with fitness levels.13 Our results extend these previous observations to heart rate during sleep. They also suggest that some of the differences in sleeping heart rate between genders in adolescents may be explained by fitness levels rather than inherent differences between males and females. However, further studies will be needed to confirm these observations.
Although our study utilized a generally healthy cohort of children and adolescents to minimize the impact comorbid symptoms and cardiorespiratory problems would have on ECG recordings, the study has some limitations. First, the extent heart rate parameters during sleep differ between unattended in-home and in-lab PSGs remains unknown. Scholle and colleagues found that there was a first-night effect on sleeping heart rates in comparison to the second night in lab recordings with second-night recordings having slower heart rates by approximately 1 to 2 beats per minute.10
Secondly, in the current study our sample initially consisted of 319 participants who underwent PSGs, yet only 163 (51.1%) of our participants had valid recorded heart rates during the in-home PSG, suggesting the possibility that the ECG lead may be more easily dropped during in-home PSGs than in-lab recordings. Thirdly, fitness level in this study was ascertained by questionnaire. Thus, there may be greater variability than if a cardiopulmonary exercise test had been performed. However, we believe that any error would be non-differential, and thus unlikely to alter our findings.
Lastly, although bedtime and wake time were available to investigate sleep routine, there was no known information regarding alternative bed time behaviors such as playing video games14 or consuming caffeinated beverages,15 which may have an impact on sleeping heart rates.
The current study presents data from a generally healthy prospective cohort of Hispanic and Caucasian children and adolescents that allowed for exclusion of children and adolescents who have evidence of sleep disordered breathing. In adult patients with sleep apnea, there is evidence that they may have lower heart rate variability and higher heart rates in comparison with controls matched for age, gender, and BMI,16 and an increase in sympathetic drive may be present in those with OSA even during wakefulness.17 Future research should further investigate potential racial differences, physical activity or fitness levels, and the impact BMI and sleep apnea have on heart parameters during sleep.
DISCLOSURE STATEMENT
This was not an industry supported study. TuCASA was supported by HL62373. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Grigg-Damberger M, Gozal D, Marcus CL, et al. The visual scoring of sleep and arousal in infants and children. J Clin Sleep Med. 2007;3:201–40. [PubMed] [Google Scholar]
- 2.Witcombe NB, Yiallourou SR, Walker AM, Horne RS. Blood pressure and heart rate patterns during sleep are altered in preterm-born infants: implications for sudden infant death syndrome. Pediatrics. 2008;122:e1242–8. doi: 10.1542/peds.2008-1400. [DOI] [PubMed] [Google Scholar]
- 3.Archbold KH, Johnson NL, Goodwin JL, Rosen CL, Quan SF. Normative heart rate parameters during sleep for children aged 6 to 11 years. J Clin Sleep Med. 2010;6:47–50. [PMC free article] [PubMed] [Google Scholar]
- 4.Salameh A, Gebauer RA, Grollmuss O, et al. Normal limits for heart rate as established using 24-hour ambulatory electrocardiography in children and adolescents. Cardiol Young. 2008;18:467–72. doi: 10.1017/S1047951108002539. [DOI] [PubMed] [Google Scholar]
- 5.Rijnbeek PR, Witsenburg M, Schrama E, Hess J, Kors JA. New normal limits for the pediatric electrocardiogram. Eur Heart J. 2001;22:702–11. doi: 10.1053/euhj.2000.2399. [DOI] [PubMed] [Google Scholar]
- 6.Goodwin JL, Babar SI, Kaemingk KL, et al. Symptoms related to sleep disordered breathing in white and Hispanic children: the Tucson Children's Assessment of Sleep Apnea Study. Chest. 2003;124:196–203. doi: 10.1378/chest.124.1.196. [DOI] [PubMed] [Google Scholar]
- 7.Witmans MB, Keens TG, Davidson Ward SL, Marcus CL. Obstructive hypopneas in children and adolescents: normal values. Am J Respir Crit Care Med. 2003;168:1540. doi: 10.1164/ajrccm.168.12.954. [DOI] [PubMed] [Google Scholar]
- 8.Rechtschaffen A, Kales A. Los Angeles: 1968. A Manual of Standardized Terminology: Techniques and Scoring Systems for Sleep Stages of Human Subjects. [DOI] [PubMed] [Google Scholar]
- 9.National Center for Health Statistics, CDC Growth Charts: United States. 2000. Available from: http://www.cdc.gov/GrowthCharts/
- 10.Scholle S, Wiater A, Scholle HC. Normative values of polysomnographic parameters in childhood and adolescence; Cardiorespiratory parameters. Sleep Med. 2011;12:988–96. doi: 10.1016/j.sleep.2011.05.006. [DOI] [PubMed] [Google Scholar]
- 11.Krishnan B, Jeffery A, Metcalf B, et al. Gender differences in the relationship between heart rate control and adiposity in young children: a cross-sectional study (EarlyBird 33) Pediatr Diabetes. 2009;10:127–34. doi: 10.1111/j.1399-5448.2008.00455.x. [DOI] [PubMed] [Google Scholar]
- 12.Peters H, Whincup PH, Cook DG, Law C, Li L. Trends in resting pulse rates in 9-11 year-old children in the UK 1980-2008. Arch Dis Child. 2014;99:10–14. doi: 10.1136/archdischild-2013-304699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tell GS, Vellar OD. Physical fitness, physical activity, and cardiovascular disease risk factors in adolescents: The Oslo Youth Study. Prev Med. 1988;17:12–24. doi: 10.1016/0091-7435(88)90068-0. [DOI] [PubMed] [Google Scholar]
- 14.Ivarsson M, Anderson M, Akerstedt T, Lindblad F. Playing a violent television game affects heart rate variability. Acta Paediatr. 2009;98:166–72. doi: 10.1111/j.1651-2227.2008.01096.x. [DOI] [PubMed] [Google Scholar]
- 15.Bonnet M, Tancer M, Uhde T, Yeragani VK. Effects of caffeine on heart rate and QT variability during sleep. Depress Anxiety. 2005;22:150–5. doi: 10.1002/da.20127. [DOI] [PubMed] [Google Scholar]
- 16.Narkiewicz K, Monatno N, Cogliati C, et al. Altered cardiovascular variability in obstructive sleep apnea. Circulation. 1998;98:1071–7. doi: 10.1161/01.cir.98.11.1071. [DOI] [PubMed] [Google Scholar]
- 17.Narkiewicz K, Van de Borne PJ, Cooley RL, Dyken ME, Somers VK. Sympathetic activity in obese subjects with and without obstructive sleep apnea. Circulation. 1998;98:772–6. doi: 10.1161/01.cir.98.8.772. [DOI] [PubMed] [Google Scholar]


