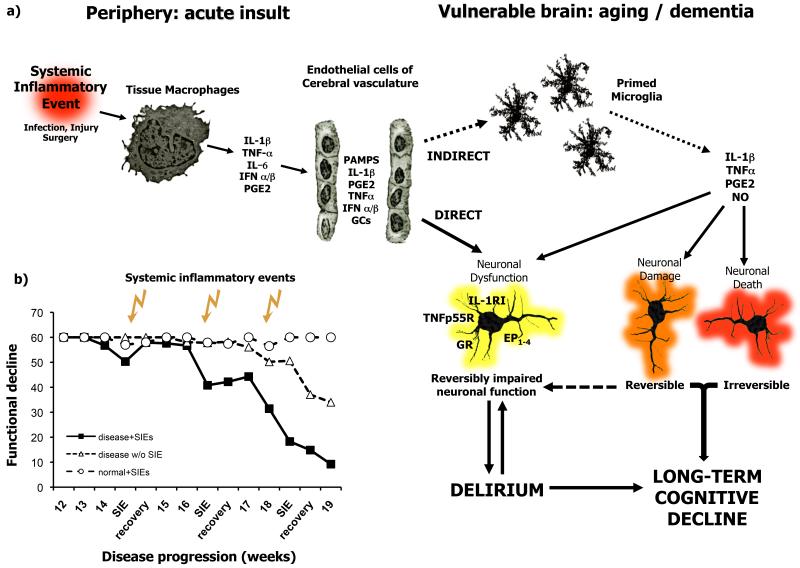
Figure 2. Systemic inflammatory events may trigger delirium and contribute to pathological burden.
a) Systemic inflammatory events trigger the release of inflammatory mediators by tissue macrophages and brain vascular endothelial cells. These mediators may impact on neuronal function directly, or via the activation of microglial cells that have become primed by neurodegenerative disease or aging. Inflammatory mediators may cause reversible disruption of neuronal function, perhaps resulting in delirium. These mediators may also induce acute neuronal synaptic or dendritic damage that may be reversible and contribute to delirium or may be irreversible and contribute to long-term cognitive decline. These inflammatory mediators can also bring about neuronal death acutely and these changes are obviously irreversible and contribute to the accumulating damage and neuropathological burden. Thus acute and long-term cognitive effects are likely to occur by both overlapping and distinct mechanisms. b) Successive systemic inflammatory insults induce acute dysfunction, which is progressively less reversible each time, but also contribute to the progression of permanent disability (adapted from Field et al., 2010 (ref 23)). Abbreviations: IL-1β: interleukin 1β; IL-1RI: interleukin 1 receptor type I; TNF-α: tumour necrosis factor α; TNFp55: TNF p55 receptor; IL-6: interleukin 6; GCs: glucocorticoids; GR: glucocorticoid receptor; NO: nitric oxide; PGE2: prostaglandin E2, EP1-4: prostaglandin receptors 1-4; PAMPs: pathogen associated molecular patterns; IFNα/β, interferons a and b; SIEs: systemic inflammatory events.