Abstract
A 37-year-old woman was referred to our institution for further management of a mass lesion located in the thoracic cavity. The mass had grown by more than 10 cm over the course of a year and was initially considered to be a scar from previous pulmonary tuberculosis at another hospital. The patient had complained of left-sided flank pain for a year and experienced dyspnea for one month. Chest radiography and chest computed tomography revealed an irregular-shaped mass in the left mid to lower pleural cavity. The mass was widely excised through left thoracotomy. Pathologic examination of the biopsy specimen revealed a malignant spindle cell tumor, which consisted of components of osteosarcoma, pleomorphic sarcoma, and leiomyosarcoma. The patient underwent adjuvant chemotherapy and has been doing well without any evidence of recurrence for 14 months.
Keywords: 1. Pleura, 2. Extraskeletal osteosarcoma
CASE REPORT
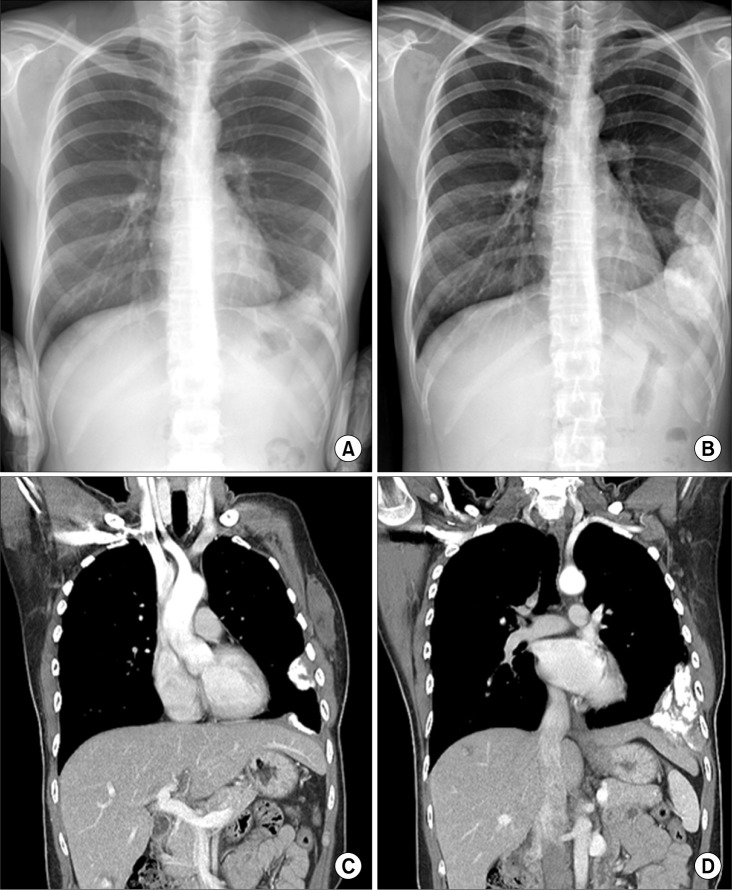
A 37-year-old woman was referred to our institution for further management of a mass lesion located in the thoracic cavity, which was revealed on a chest computed tomography (CT) scan taken at another hospital. She complained of left-sided flank pain that was aggravated with deep inspiration for twelve months and began to experience dyspnea for one month. She had a history of pulmonary tuberculosis with a six-month course of anti-tuberculosis medication 20 years earlier. She did not have a history of smoking or environmental or occupational exposures to toxins. The laboratory tests including tumor markers on admission were normal. The result of acid fast staining of her sputum was also normal. Findings of physical examinations were unremarkable. The initial chest radiograph taken at the other hospital 8 months previously demonstrated an ambiguous consolidation in the left lower lung without a definite mass lesion (Fig. 1A). The patient did not receive treatment for the lesion but has been followed-up for eight months. A chest radiograph taken eight months after the initial visit revealed an irregularly shaped large mass occupying the left lower lung field and compressing the left lower lobe and diaphragm (Fig. 1B). Compared with the initial chest radiograph, the mass had grown markedly. Consequently, chest CT was carried out immediately. Chest CT showed two irregularly shaped soft tissue masses adjacent to the parietal pleura in the left hemithorax, which contained dense calcifications without the invasion of the ribs (Fig. 2).
Fig. 1.
Chest radiograph that was carried out: (A) at another hospital eight months previously and (B) at the time of admission. Chest computed tomography revealed two separated tumors. (C) A 4-cm mass adjacent to inner side of the shaft of the 6th rib and (D) an 8-cm mass located at the costophrenic angle.
Fig. 2.
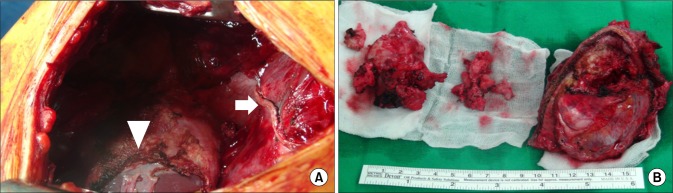
Operative findings and gross findings of the mass. (A) Radical excision of the tumor involved wedge resection of the left lower lobe of the lung (arrow) and partial resection of the diaphragm (arrowhead). (B) After removal, the tumors showed a hard surface and an irregular margin, and the mass contained calcification.
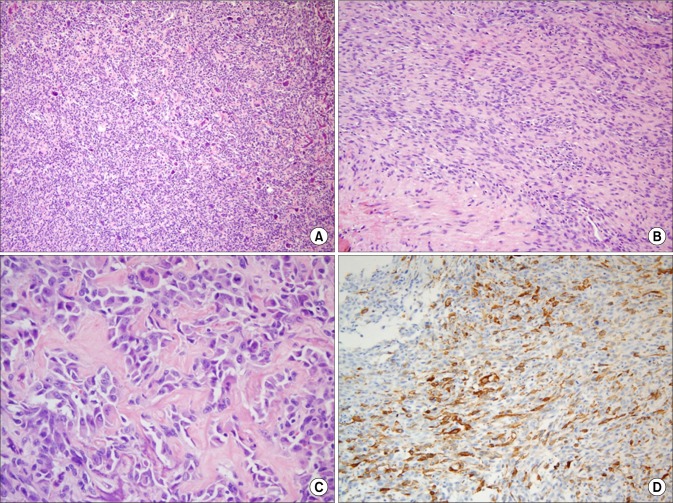
For correct diagnosis and proper treatment, surgical excision of the masses was performed through left thoracotomy via the 7th intercostal space. The intraoperative findings showed two hard and irregularly shaped masses with a hard osteoid surface. These masses were clearly separated. One was 8 cm in size and was located at the costophrenic angle, and the other was 4 cm in size, located adjacent to the inner surface of the shaft of the 6th rib. They had invaded the adjacent structures including the left lower lobe, chest wall, and the diaphragm, but had not invaded the adjacent ribs. These masses were radically excised involving the invaded organs to obtain adequate resection margins (Fig. 3), and the defect of the diaphragm was reconstructed with a 2-mm-thick polytetrafluoroethylene (Gore-Tex WL Gore and Associates Inc., Flagstaff, AZ, USA) patch. Histologically, the tumors consisted of osteosarcoma, pleomorphic sarcoma, and leiomyosarcoma. The microscopic findings (H&E stain) showed the histologic appearance of the mass (Fig. 3), which consisted of smooth muscle differentiation and osteoid production cells. Differences in nuclei size and shape were also observed in the H&E stain. In the immunohistochemistry stain, smooth muscle actin was detected. The microscopic findings of the two masses were the same, and therefore, these were considered seeding. The patient underwent four cycles of adjuvant chemotherapy with the regimen of high-dose methotrexate, cisplatin, and doxorubicin. Currently, she is doing well without any evidence of recurrence for 14 months after surgery.
Fig. 3.
Microscopic findings of the mass. (A) Differences in nuclei size and shape (H&E, ×100). (B) Smooth muscle differentiation (H&E, ×200). (C) Osteoid production cells (H&E, ×400). (D) Smooth muscle actin detection (immunohistochemistry stain, ×200).
DISCUSSION
Extraskeletal osteosarcoma is a rare malignancy that accounts for approximately 1% to 2% of all soft tissue sarcomas and 4% of all osteosarcomas [1]. Extraskeletal osteosarcoma is defined as the malignant tumor originating from the soft tissues without involvement of the bone and composed of malignant cells of an osteoblastic phenotype producing an osseous matrix [2]. It dominantly occurs in middle-aged patients in contrast to osteogenic sarcoma, which commonly occurs in younger patients under the age of 20 years, and the tumor can cause symptoms by its mass effect. Approximately half the cases of this tumor occur in the lower extremity, and the other half frequently occur in the upper extremity, retroperitoneum, and the trunk [3]. Extraskeletal osteosarcoma rarely occurs in the pleural cavity, and a majority of these tumors arise from the diaphragm [2]. Furthermore, the tumor originating from the parietal pleura is extremely rare [4]. This case is the first report on extraskeletal osteosarcoma that originated from the pleura in Korea.
Radiologically, extraskeletal osteosarcoma often appears as a mass with soft-tissue opacity and a diverse degree of mineralization on the chest radiograph. In approximately 50% of the patients with this tumor, calcification or osteoid formation is found. On the CT scan, the tumor is found to be separate from the adjacent osseous structures and has a pseudocapsule. Moreover, CT is the best method for the detection of matrix mineralization [3]. However, differential diagnosis of extraskeletal osteosarcoma by a CT scan is generally difficult even though the CT scan can provide precise images, because calcification in the pleural cavity can be produced by other etiologies including benign and malignant diseases [4]. The benign causes include trauma, infection, bleeding, calcifying fibrous pseudotumor, and calcified plaque by asbestos exposure, while the malignant causes include metastasis from osteogenic osteosarcoma, malignant pleural mesothelioma, parosteal osteosarcoma of the rib, and osseous Paget’s disease of the bone [2,4]. Therefore, comprehensive consideration including symptoms, occupational history, and medical history is required for correct diagnosis.
In general, the most common site of metastasis by osteogenic osteosarcoma is the lung (up to 88% of osteoid osteosarcoma) [3]. Therefore, the possibility of pulmonary metastasis should be considered first for patients who present with pleural osteosarcoma. In our case, however, primary osteogenic osteosarcoma occurring in the other organs was not found.
The tumor has been known for a high-grade malignancy with poor prognosis (5-year survival rate: 37%), and it commonly metastasizes to the distant organs [5]. Radical resection of the tumor has been considered the appropriate initial treatment because the tumor is not particularly chemosensitive or radiosensitive [3]. There are no specific guidelines for chemotherapy for extraskeletal osteosarcomas. Therefore, the role of chemotherapy in the treatment of the tumor is still being debated. Regarding the efficacy of chemotherapy, a retrospective clinical analysis reported the clinical outcomes of the patients receiving adjuvant chemotherapy for extraskeletal osteosarcoma that occurred mainly at the lower extremities [6]. The cited study reported favorable prognosis of adjuvant chemotherapy for extraskeletal osteosarcoma. In our study, the patient is doing well with adjuvant chemotherapy.
In conclusion, this is an extremely rare case of extraskeletal osteosarcoma that originated from the parietal pleura. Although the mass was initially considered to be a scar of previous pulmonary tuberculosis, as in this case, the possibility of primary malignant tumor should be considered in patients who present with pleural calcification. If the mass is assessed to be resectable, surgical resection of the tumor can be the standard option for correct diagnosis as well as proper treatment.
Footnotes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Song HK, Leibold TM, Gal AA, Miller JI., Jr Extraskeletal osteosarcoma of the diaphragm presenting as a chest mass. Ann Thorac Surg. 2002;74:565–7. doi: 10.1016/s0003-4975(02)03556-7. [DOI] [PubMed] [Google Scholar]
- 2.Matono R, Maruyama R, Ide S, et al. Extraskeletal osteosarcoma of the pleura: a case report. Gen Thorac Cardiovasc Surg. 2008;56:180–2. doi: 10.1007/s11748-007-0216-5. [DOI] [PubMed] [Google Scholar]
- 3.Mc Auley G, Jagannathan J, O’Regan K, et al. Extraskeletal osteosarcoma: spectrum of imaging findings. AJR Am J Roentgenol. 2012;198:W31–7. doi: 10.2214/AJR.11.6927. [DOI] [PubMed] [Google Scholar]
- 4.Shiota H, Yasukawa T, Hirai A, Chiyo M, Yusa T, Hiroshima K. Extraskeletal osteosarcoma of the pleura:report of a case. Ann Thorac Cardiovasc Surg. 2013;19:297–301. doi: 10.5761/atcs.cr.12.01964. [DOI] [PubMed] [Google Scholar]
- 5.Lee JS, Fetsch JF, Wasdhal DA, Lee BP, Pritchard DJ, Nascimento AG. A review of 40 patients with extraskeletal osteosarcoma. Cancer. 1995;76:2253–9. doi: 10.1002/1097-0142(19951201)76:11<2253::aid-cncr2820761112>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 6.Goldstein-Jackson SY, Gosheger G, Delling G, et al. Extraskeletal osteosarcoma has a favourable prognosis when treated like conventional osteosarcoma. J Cancer Res Clin Oncol. 2005;131:520–6. doi: 10.1007/s00432-005-0687-7. [DOI] [PubMed] [Google Scholar]