Abstract
Objective
Persistent infection with high-risk (HR) HPV is a necessary risk factor for the development of cervical cancer. Information on HPV infection is limited in Puerto Rico. This study determined the distribution of HPV types and the association of HR-HPV types with cervical pathology in a clinic-based sample of women in PR.
Methods
Data from 92 female participants aged 18 to 34 years and recruited from the University of Puerto Rico-Gynecology Clinic, were analyzed. Cervical cytology was performed. HPV testing was performed using L1 consensus primer PCR with MY09/MY11 primers and typed by dot-blot hybridization. Logistic regression modeling was used to determine the crude and covariate adjusted association between HR-HPV and cervical pathology.
Results
Twenty percent (n=18) of the patients had abnormal cytology, 45.7% (n=42) were HPV positive, and 30.4% (n=28) were HR HPV-positive. Women infected with HR-risk HPV types were 7.9 (95% CI = 2.5–25.5) times likely to have abnormal cytology as compared to women without HR infection when adjusted by age and age at first sexual intercourse.
Conclusions
The burden of HPV infection was high, and, as expected, HR HPVs were strongly associated with dysplasia. A population-based study is needed to estimate HPV prevalence and its association with related malignancies in our population. This will be of great value in determining disease burden and will increase awareness of the HPV vaccination in our population.
Keywords: Cervical cancer, Prevention, Screening, Self-sampling
Introduction
Cervical cancer is the fifth most commonly diagnosed cancer in Puerto Rican women [1]. When compared to that of the United States (US), the age-adjusted incidence rate of cervical cancer (9.1 per 100,000) in Puerto Rico is close to double that of non-Hispanic Whites (NHW) (5.9 per 100,000), although it is lower than what is found in Hispanics (12.9 per 100,000) living on the US mainland [2].
Cervical cancer is almost entirely preventable and curable if detected early [3]. Human papillomavirus (HPV), the most common sexually transmitted infection in the US, is linked etiologically to cervical cancer [4]. Epidemiological and laboratory data have demonstrated that persistent infection with high-risk (HR) HPV types is a necessary risk factor for the development of invasive cervical cancer [5]. Population-based type-specific HPV prevalence data provide baseline data for determining disease burden in a population and is essential for future assessment of the impact of HPV vaccination programs on cervical cytology [5]. Dunne and colleagues reported that the most common HPV types detected in females aged 14 to 59 years from the National Health and Nutrition Examination Survey in the years 2003–2004 were HPV 62 (3.3%), HPV 84 (3.3%), HPV 53 (2.8%), HPV 89 (2.4%), HPV 61(2.4%) and HPV 16 (1.5%). Overall, HPV types 6, 11, 16 and 18 were detected in 3.4% of the study participants, corresponding to 3.1 million females infected with HPV types included in the current quadrivalent HPV vaccine [4], which has been approved by FDA to prevent HPV infection in males and females from 9 to 26 years old.
Information on HPV infection and its relation to HPV-related malignancies is very limited for PR; this information is essential for the further development and improvement of prevention and treatment strategies for cervical dysplasia and cervical cancer in the island, including vaccination programs. Thus, to our knowledge, this pilot study describes for the first time the frequency distribution of HPV types (high and low risk), by cervical pathology status, and assesses the association of HR -HPV types with cervical pathology in a clinic-based sample of women in PR.
Materials and Methods
Our study population consisted of 100 consecutive women who visited the Gynecology Clinic of the University of Puerto Rico (UPR) School of Medicine, who qualified for the study, and who consented to participate. This clinic is a general gynecology clinic at a tertiary institution at which gynecological care is provided to women, including those who are considered high-risk cases, those who are institutionalized, and those of lower incomes.
Complete information on HPV status was assessed for 92 women, and thus, data from these were included in the analysis. Inclusion criteria were that the woman be 18 to 34 years old, that she have an intact uterus, that she be sexually active, and that she be without a history of cervical carcinoma or any recent cervical procedures, such as cone biopsy or LEEP biopsy (loop electrical excisional procedure). An interviewer-administered questionnaire was used to collect data on potential demographic and lifestyle risk factors, including history of STI’s, while information on sexual practices was collected through a self-administered questionnaire using an Audio Computer Assisted Self-Interview (ACASI) system implemented using the Questionnaire Development System (QDS) (Nova Research Co., Washington D.C.). Cervical HPV and cytology samples were collected from each participant. HPV samples were taken first by a study physician, and subsequently self-sampling was performed by the patients following written instructions [6]. Self-collection followed similar procedures to those previously used in other studies [7].
HPV testing of samples was performed using L1 consensus primer PCR with MY09/MY11 primers at the University of California - San Francisco. Positive PCR products were typed by dot-blot hybridization using 39 individual type-specific probes, including oncogenic HPV types (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, and 68) and non-oncogenic types (6/11, 26/69, 30, 32/42, 34, 53, 54, 57/2/27, 61, 62, 67, 68, 70, 71, 72, 73, 81, 82, 83, 84, 85, 86/87, 90/106, 97, 102/108, as well as 2 separate mixtures, mix1 contains 7/13/40/43/44/55/74/91, and mix2 contains 3/10/28/29/77/78/94 plus all those HPV types that hybridized only with the consensus probe) defined according to IARC [5] and were based on the results of both the physician- and the self-collected samples. Variables studied included cervical cytology and HPV infection status. Cervical cytology results were determined to be either normal or abnormal; abnormal cytology included atypical squamous cells of undetermined significance (ASCUS), atypical squamous cells-cannot exclude high grade squamous intraepithelial lesion(ASC-H), low grade squamous intraepithelial lesion (LSIL), low grade squamous intraepithelial lesion (HSIL) and cancer. HPV infection was divided into HR (oncogenic) and low-risk (LR) (non-oncogenic) categories. Descriptive statistics were performed to summarize the demographic and clinical characteristics of the study group. The chi-square statistic was used to assess factors associated with cervical pathology. Logistic regression models were used to assess the crude and covariate-adjusted association between HR-HPV status and cervical cytology. Interaction terms in the model were evaluated with the likelihood ratio test.
Results
The median age in our sample was 26.4 years (percentiles 25 and 75: 23–30), with a mean age at first sexual intercourse of 18.1 ± 3.0 years (Table 1). The mean number of sexual partners in the last year and lifetime was 1.0 (percentiles 25 and 75:1–2) and 4 (percentiles 25 and 75: 2–6) partners respectively. Only one woman (1.1%) aged 18 to 26 years (recommended vaccination ages) had been vaccinated with the HPV vaccine. Meanwhile, 20% of the women had an abnormal Pap test result (6.5% ASCUS, 9.8% LSIL, and 3.3% HSIL).
Table 1.
Characteristics of study participants by cytology status (n = 92)*
| Characteristics | Cytology Status n (%) | Chi-square (p-value) | |
|---|---|---|---|
| Normal (n=74) | Abnormal (n=18) | ||
| Age (years) | 0.661 | ||
| 18–25 | 33 (44.6%) | 7 (38.9%) | |
| 26–34 | 41 (55.4%) | 11 (61.1%) | |
| Education (years) | 0.963 | ||
| <12 | 12 (16.2%) | 3 (16.7%) | |
| ≥12 | 62 (83.8%) | 15 (83.3%) | |
| Marital status | 0.618 | ||
| Single | 44 (60.3%) | 12 (66.7%) | |
| Married/cohabitating | 29 (39.7%) | 6 (33.3%) | |
| Age at first sexual intercourse (years) | 0.127 | ||
| <18 | 39 (52.7%) | 6 (33.3%) | |
| ≥18 | 35 (47.3%) | 12 (66.7%) | |
| Number of sexual partners (last 12 months) | 0.679 | ||
| 0–1 | 53 (71.6%) | 12 (66.7%) | |
| ≥2 | 21 (28.4%) | 6 (33.3%) | |
| Non-barrier contraceptive use | 0.837 | ||
| Yes | 35 (47.3%) | 9 (50.0%) | |
| No | 39 (52.7%) | 9 (50.0%) | |
| Ever smoking** | 0.526 | ||
| Yes | 16 (84%) | 3 (16%) | |
| No | 34 (76%) | 11 (24%) | |
| History of STI’s*** | 0.545 | ||
| Yes | 20 (27.0%) | 3 (16.7%) | |
| No | 54 (73.0%) | 15 (83.3%) | |
| HR HPV-DNA | |||
| Negative | 58 (78.4%) | 6 (33.3%) | 0.002 |
| Positive | 16 (21.6%) | 12 (66.7%) | |
n<100 due to missing data;
n = 64 due to missing data on smoking status;
self-reported history of the following STIs: HIV/AIDS, Gonorrhea, Syphilis, Genital warts, Genital Herpes, Chlamydia, Thrichomonas, and HPV; no participant reported having HIV/AIDS.
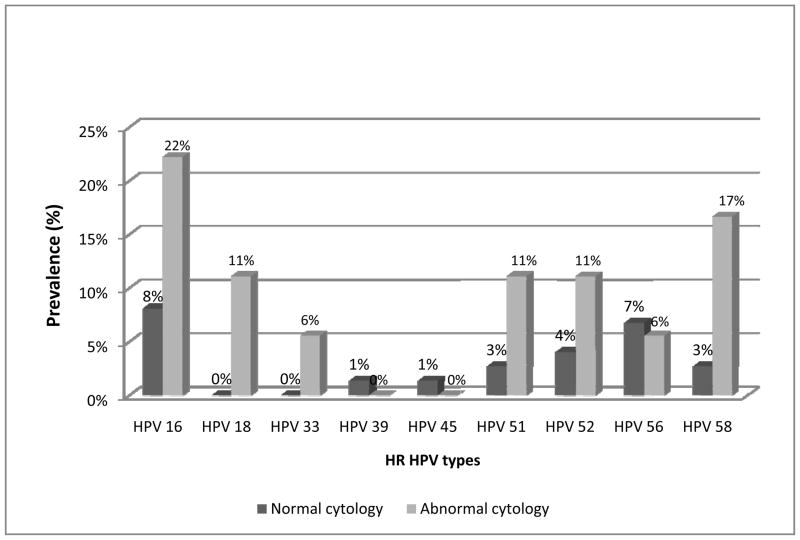
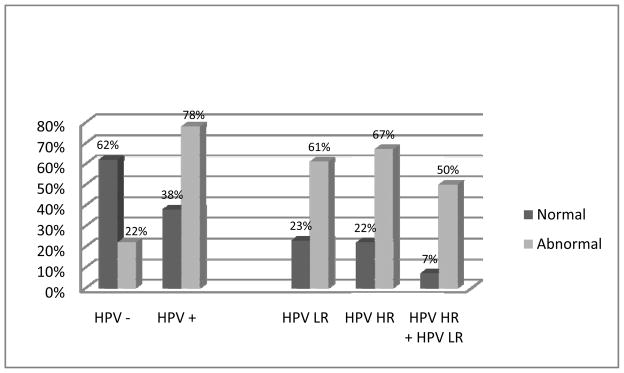
Regarding HPV results, −54.4% of women were HPV-negative and 45.7% were HPV-positive, with 30.4% (n=28) being positive for HR types only, 15.2% (n=14) positive for both LR and HR HPV types, and 30.4% (n=28) positive for LR HPV types only (Figure 1). The prevalence of HPV infection was higher in patients with abnormal cervical cytology results than among those with normal cervical cytology results (Figure 2). Of the patients with abnormal cytology, 33.3% (6/18) were negative for HR HPV and 66.7% (12/18) were positive for HR HPV types (p=0.002). Among those with HSIL (n=3), two were infected with HPV 16 and one with HPV 52. Of the patients with one or more HR types and an abnormal Pap smear, 11.1% (n=2/18) were positive for just one type, 44.4% (n=8/18) were positive for 2 types, and 11.1% (n=2/18) were positive for four (data not shown). Overall, the most prevalent HR HPV types were 16 (n=10, 10.9%), 52 (n=5, 5.4%), 53 (n=5, 5.4%), 56 (n=6, 6.5%) and 58 (n=5, 5.4%; only 2.2% of women (n=2) were infected with HPV 18. In patients with abnormal cytology, the most prevalent HR HPV types were 16 (22.2%), 18 (11.1%), 51 (11.1%), 52 (11.1%), and 58 (16.7%); in those with normal pathology, the prevalence of these HPV types was lower (Figure 3).
Figure 1.
Overall HPV infection results (n=92)
(HPV LR = low-risk human papillomavirus, HPV HR = high-risk human papillomavirus)
Figure 2.
HPV infection in cervical samples, by cervical cytology results.
Figure 3.
Prevalence of HR HPV types in cervical samples, by cervical cytology results.
In bivariate analysis, the only factor statistically associated (p<0.05) with abnormal cytology results was infection with HR-HPV types (p=0.003). No significant associations with abnormal cervical cytology results were observed for the following variables: age, marital status, education, age at first sexual intercourse, smoking status, history of STIs, number of sexual partners in the last year, or use of non-barrier contraceptives (p>0.05) (Table 1). In logistic regression models, after adjusting for age and age at first sexual intercourse, the odds of having an abnormal cytology in patients positive for HR HPV types was 7.9 (95% CI = 2.5–25.5) times the odds of having an abnormal cytology in HR-HPV-negative patients (p=0.002) (Table 2). No significant (p>0.05) interaction terms were observed in this model.
Table 2.
Logistic regression models of the association of HR-HPV infection and cervical cytology
| Characteristics | Crude POR (95% CI) | Adjusted POR** (95% CI) |
|---|---|---|
| HR-HPV-DNA | ||
| Negative* | 1.0 | 1.0 |
| Positive | 7.25 (2.4 – 22.3) p=0.001 |
7.9 (2.5 – 25.5) P=0.001 |
no HPV or only LR HPV
Adjusted for age and age at first sexual intercourse
Discussion
To our knowledge this is the first study to describe the frequency of HPV infection and its relation to cervical cytology in a clinic-based sample of women in PR. As expected, a strong association of HR-HPV types with abnormal cervical cytology was found. Our study population was a high-risk population, as 20% of patients surveyed had an abnormal cytology result. This percentage is higher than what would be expected in the general US population (5%) [8], although just slightly higher than that reported in a similar clinic-based population of 9,657 women aged 14 to 65 years receiving routine cervical screening in the US [9]. The high number of women with abnormal cytology in this study reflects the fact that this is a clinic-based study, and estimates of disease burden are expected to be higher than those in the general population. Furthermore, despite its being a general gynecology clinic, it also is a tertiary care center, one to which low socioeconomic status women—who could be at higher risk for sexually transmitted infections—are frequently referred [10]. Nonetheless, despite the potential for selection bias in our study, patients with cervical infection with HR-HPV types had higher the odds of having an abnormal cytology than did those without HR-HPV infection, after adjusting for age and age at first sexual intercourse, which is consistent with other studies worldwide [11]. In addition, this result is consistent with the well-established association between HPV and cervical dysplasia [5,12].
Disparities in cervical cancer incidence and mortality rates exist among women Hispanic and women of African ancestry, as well as in developing Latin American countries and the Caribbean. Ortiz and colleagues reported that the higher incidence of cervical cancer observed among US Hispanics, non-Hispanic Blacks, and Puerto Ricans, compared to that of non-Hispanic Whites, could reflect either a potential higher prevalence of HPV infection in these populations or lower screening rates in these groups [2]. No population-based data on the prevalence of HPV exist for PR that might explain the burden of cervical cancer among women in this population. In our sample of 92 Puerto Rican women, 43.5% were positive for HPV infection, which is consistent with our hypothesis that women in PR have a high prevalence of HPV infection. Dunne et al. [4] reported an overall HPV prevalence of 26.8% among a representative sample of females aged 14 to 59 years in the US. Nonetheless, this has to be confirmed in population-based studies, as a higher prevalence of infection is expected in clinic-based samples [5]. Despite the high disease burden, only 1.1% of the participants aged 26 years or younger had a history of HPV vaccine administration at the time of the study, which suggests a low uptake of the vaccine in this group, and this only two years after the approval of the first HPV vaccine in the US. As a result of this observation, all the patients in our study who were candidates for the vaccine were referred to the vaccination clinic so that they might receive information about the HPV vaccine and, when interested, receive the vaccine itself.
Among the study’s limitations is the fact that subjects recruited for this study were women who underwent evaluation at a single clinical referral center; thus, it is possible that our results are not be generalizable to the female population in PR. In addition, our small sample size limited the power of our study to assess the association between demographic and lifestyle factors (such as cigarette use, which is a known co-factor for a positive Pap test) and cytology status. Given the cross-sectional nature of our study, we cannot differentiate between incident and persistent HPV infections. Thus, even though many of the HPV infections detected among study participants will regress, some women might have incident infections, which have not yet progressed to premalignant lesions, underestimating the observed odds of the association between HPV infections and cervical malignancies.
In conclusion, our study showed that the burden of HPV infection was high in this clinic-based sample of women in PR, with a high prevalence of HPV types not included in currently available HPV vaccines. Also, as expected, HR HPVs were strongly associated with dysplasia and HPV 16 was the most common type among women with HSIL. A population-based study is needed to estimate HPV prevalence in PR and to assess, as well, its association with related malignancies. This will be of great value in the determination of disease burden and will increase awareness of HPV vaccination in our population.
Acknowledgments
Financial support: This work was sponsored by grant U54RR026139-01A1 of the National Center for Research Resources and U54 MD 007587-03 of the National Institute on Minority Health and Health Disparities from the National Institutes of Health; by grant number G12RR003051 (RCMI Program, University of Puerto Rico Medical Sciences Campus) from the National Center for Research Resources (NCRR), components of the National Institutes of Health (NIH); and by U54CA96297 and U54CA96300 from the UPR/MDACC Partnership for Excellence in Cancer Research, National Cancer Institute. The contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Cancer Institute.
This study was approved by the IRB of the UPR-MSC (Protocol A1810108) and sponsored by grant U54RR026139-01A1 of the National Center for Research Resources and U54MD 007587-03 of the National Institute on Minority Health and Health Disparities from the National Institutes of Health; by grant number G12RR003051 (RCMI Program, University of Puerto Rico Medical Sciences Campus) from the National Center for Research Resources (NCRR), components of the National Institutes of Health (NIH); and by U54CA96297 and U54CA96300 from the UPR/MDACC Partnership for Excellence in Cancer Research, National Cancer Institute.
Footnotes
The authors have no conflict of interest to disclose
References
- 1.Torres-Cintrón M, Ortiz AP, Pérez-Irizarry J, et al. Incidence and Mortality of the Leading Cancer Types in Puerto Rico: 1987–2004. P R Health Sci J. 2010;29:317–329. [PubMed] [Google Scholar]
- 2.Ortiz AP, Soto-Salgado M, Calo WA, et al. Incidence and mortality rates of selected infection-related cancers in Puerto Rico and in the United States. Infect Agent Cancer. 2010;5:10. doi: 10.1186/1750-9378-5-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.DiSaia P, Creasman W. Clinical Gynecologic Oncology. 7. St. Louis MO: Mosby Elsevier; 2007. pp. 2–3. [Google Scholar]
- 4.Dunne EF, Unger ER, Sternberg M, et al. Prevalence of HPV infection among females in the United States. JAMA. 2007;297:813–819. doi: 10.1001/jama.297.8.813. [DOI] [PubMed] [Google Scholar]
- 5.IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Human papillomavirus. 100B. Lyon, France: International Agency for Research on Cancer; 2011. [Accessed February 6, 2013]. Available at: http://monographs.iarc.fr/ENG/Monographs/vol100B/index.php. [Google Scholar]
- 6.Ortiz AP, Alejandro N, Pérez CM, Otero Y, Soto-Salgado M, Palefsky J, Tortolero-Luna G, Romaguera J. Acceptability of cervical and anal HPV self-sampling in a sample of Hispanic women in Puerto Rico. P R Health Sci J. 2012;31(4):205–12. [PMC free article] [PubMed] [Google Scholar]
- 7.Gravitt PE, Lacey JV, Jr, Brinton LA, et al. Evaluation of Self-Collected Cervicovaginal Cell Samples for Human Papillomavirus Testing by Polymerase Chain Reaction. Cancer Epidemiol Biomarkers Prev. 2001;10:95–100. [PubMed] [Google Scholar]
- 8.Results from the National Breast and Cervical Cancer Early detection program October 31, 1991-September 30, 1993. MMWR. 1994;43:530–544. [PubMed] [Google Scholar]
- 9.Datta SD, Koutsky LA, Ratelle S, et al. Human Papillomavirus Infection and Cervical Cytology in Women Screened for Cervical Cancer in the United States, 2003–2005. Ann Intern Med. 2008;148:493–500. doi: 10.7326/0003-4819-148-7-200804010-00004. [DOI] [PubMed] [Google Scholar]
- 10.U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health. Agenda for Research on Women’s Health for the 21st Century: A Report of the Task Force on the NIH Women’s Health Research Agenda for the 21st Century. Vol. 2. Bethesda, MD: 1999. NIH Publication No. 99–4386. [Google Scholar]
- 11.Sargent A, Bailey A, Almonte M, et al. Prevalence of type-specific HPV infection by age and grade of cervical cytology: data from the ARTISTIC trial. Br J Cancer. 2008;20; 98:1704–1709. doi: 10.1038/sj.bjc.6604324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tota JE, Chevarie-Davis M, Richardson LA, Devries M, Franco EL. Epidemiology and burden of HPV infection and related diseases: implications for prevention strategies. Prev Med. 2011;53 (Suppl 1):S12–21. doi: 10.1016/j.ypmed.2011.08.017. [DOI] [PubMed] [Google Scholar]