Abstract
Objectives
The atraumatic restorative treatment (ART) was developed as an affordable, patient-friendly dental caries management procedure that does not need extensive operator training or special skills. The aim of this study was to determine factors that influence the decision to use ART using an innovative marketing research technique known as conjoint analysis.
Methods
A conjoint survey was completed by 723 members of the American Academy of Pediatric Dentistry. Three factors (age of the child, level of cooperation, type of insurance) were varied across three levels to create nine patient scenarios. The weights that practitioners placed on these factors in decisions to use ART in treating carious lesions were determined by conjoint analysis. Factors such as lesion location, depth, and extension were fixed in the nine clinical scenarios.
Results
Seven-hundred twenty-three pediatric dentists completed the survey (32 percent). Age of the child was the most important factor in pediatric dentists’ decisions to use ART (46 percent) compared with level of cooperation (41 percent) and type of insurance coverage (11 percent). For the age factor, the age of 2 years had the greatest utility (0.55) compared with age 4 (−0.09) and age 6 (−0.46). For types of insurance coverage, having no insurance (0.124) had the greatest utility compared with having public insurance (−0.119).
Conclusions
Although insurance coverage was the least important among the factors, being without insurance, being very young, and being uncooperative was the scenario where pediatric dentists most favored ART when making trade offs between different factors using the conjoint design.
Keywords: dental atraumatic restorative treatment, decision making, conjoint analysis, pediatric dentistry, access to health care
Introduction
The atraumatic restorative treatment (ART) was developed as an affordable, patient-friendly dental caries management procedure that does not need extensive operator training or special skills (1,2). Although the early applications of ART were in field settings in developing countries, recent research suggests that ART conforms to modern minimal invasive dentistry concepts (3,4) and can be applied in modern clinical settings in developed countries (5). This conclusion was supported by two recent systematic reviews: the first one showed that survival rate for ART restorations were high in single-surface restorations in primary teeth and permanent teeth (6) and the second one showed that when compared with amalgam, ART showed no significant difference in primary teeth (6) and did better than amalgam in permanent teeth (7). Equally important, the ART approach, because of its shorter clinical sessions and reduced cost of treatment (8), could be of a particular benefit to underserved children who have high treatment demands, those with difficult access to dental care and limited financial resources.
In the United States, The American Academy of Pediatric Dentistry (AAPD) considers ART a means of restoring and preventing caries in populations that have little access to traditional dental care (9). However, despite the advantages discussed above, the practice of ART is not believed to be widely used in the United States. Factors related to the use of ART in the United States among pediatric dentists are still unknown. Moreover, studies that have assessed dentists’ use of specific techniques are relatively rare and typically have significant limitations.
The most common method for assessing dental restorative treatment decisions have been surveys that ask direct questions about specific treatments or use simple ranking techniques to gather information about the factors that influence professionals’ decision to use certain dental procedures over others (10). This common methodology only assesses professionals’“stated decisions,”evaluating one factor at a time, and does not assess“derived decisions” or the relative importance of each factor (10). Simple self-reported survey responses are also susceptible to social desirability bias (11), failing to both incorporate any concept of opportunity cost or measure preference strength (10). To avoid those shortfalls, the present study used conjoint design to investigate patient factors that influence pediatric dentists’ decisions whether to use ART with their patients. Conjoint analysis can better model actual decision making because it requires respondents to make trade offs in a holistic context,as opposed to surveys which do not impose a resource constraint such as when respondents can rate all attributes as “extremely important” without having to evaluate trade offs (11-13).
A number of examples of conjoint analysis have been utilized in public health and health care research (14-18). In spite of this, the use of conjoint analysis is still rare in dental research (11-13). One of the applications where conjoint analysis was used in dental research assessed the determinants of dentists’ decisions to provide a particular restorative treatment dental implants. This study found disagreement between what dentists state to be important (self-reported task) and the factors they actually use to judge the suitability of implant treatment (hypothetical scenarios based on a con-joint task) (11). In other words, social desirability which is a concern in self-reported surveys is minimized when conjoint task is used.
Dentists’ treatment decisions usually involve factors related to the dentists themselves, the patients, and community factors in addition to the clinical presentation.Given that ART is cheap, relatively fast and simple, and causes less anxiety in children than the traditional restorative approach (2), it may be of value for children with problematic access to dental care. Thus, the present study focused on dentists’ perception of the importance of patients’ nonclinical factors and investigated the influence of child's age, level of cooperation, and insurance coverage on willingness of pediatric dentists to perform ART restorations using hypothetical patient scenarios and conjoint design. In this study, the hypothesis was that pediatric dentists’ use of ART is higher for younger children, for uncooperative children, and for those without insurance.
Methods
This was a cross-sectional exploratory study using a web-based questionnaire with 21 items. The survey was pretested for content validity, using cognitive analysis by six faculty members from the Department of Preventive and Community Dentistry and the Department of Pediatric Dentistry, at the University of Iowa during the spring of 2010. Pilot testing for face validity was carried out by six pediatric dentistry senior residents who pretested the instrument and shared their feedback with the lead investigator.
A national random sample of 2,237 active members of the AAPD, all of whom were registered as pediatric dentistry specialists, was invited to participate in this survey in May 2011. An invitation e-mail was sent to the entire study sample which included a link to the web survey. Three reminder e-mails were sent to nonresponders after 2, 4, and 6 weeks. The University of Iowa Institutional Review Board approved all aspects of this study.
The questionnaire had three sections: a) nine conjoint questions; b) nine demographic and practice characteristics questions; and c) three follow-up questions: if they considered ART to be definitive or interim treatment and why, as well as a question asking where they learned about ART. ART was defined in the introduction of the survey as“A procedure based on removing carious tooth tissues using hand instruments alone and restoring the cavity with an adhesive restorative material” (2).
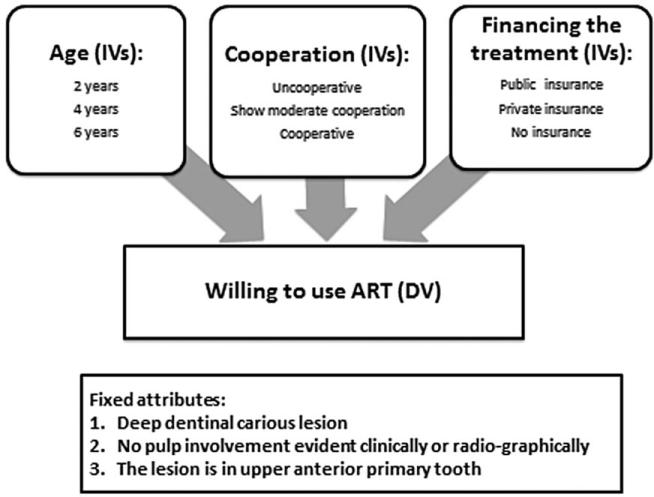
Conjoint analysis elicits preferences of a decision over the range of factors and levels that define the hypothetical scenarios used in the conjoint analysis questions (19). Although all factors that influence pediatric dentists’ decision to use ART should be considered, information and statistical efficiency dictate the use of a limited number of factors to produce the most relevant and efficient parsimonious design (20). Different behavioral and system attributes that were found in the literature that were thought to be important in influencing providers’ restorative treatment decision were included in the scenarios (21-23). These attributes were refined by consultations with experts from pediatric dentistry, dental public health, and health policy; three nonclinical factors were selected: age of the child,cooperation level of the child, and the type of insurance coverage. For each attribute, three levels were identified as shown in Figure 1 which illustrates the conceptual model of this study.
Figure 1.
The conceptual model of our conjoint study including the three factors and their levels.
The published literature and expert opinions helped in assigning the appropriate levels for each factor. For the factor “age of the child,” the expert panel chose the ages 2, 4, and 6, which coincides with three important stages of primary tooth development – eruption, full primary dentition, and exfoliation – and as such, age served as a proxy for tooth development stage. For the factor “child cooperation in the clinical setting,” Frankl's classification was assigned as follows: “uncooperative” for Frankl's class 1, “shows moderate cooperation” for Frankl's class 2, and “cooperative” for Frankl's classes 3 and 4. Frankl's behavioral scale is recommended by the AAPD guidelines (24) to rate children's behavior in clinical settings and was also defined in the introduction of the survey.
The literature found that treatment decisions are usually influenced by prior knowledge of the patients’ source of financing (25). The factor “insurance status of the patient” was used to categorize payments made to dental care providers by a third party (26). The three categories were private insurance, public insurance, or no insurance coverage, with public dental coverage considered to include Medicaid and the Children's Health Insurance Program (27).
Each participant was presented with nine patient scenarios; each scenario represented a specific scenario of a child patient with dental caries seeking restorative treatment for a primary tooth. The clinical presentation of the dental caries in the nine patient scenarios was identical so that all scenarios included the same carious lesion deep into the dentin but with no pulpal involvement evident clinically or radiographically. However, the conjoint factors – age, cooperation, and insurance status – were varied among the nine scenarios. Two surveys were sent out at the same time to two different random samples selected from the AAPD member list using survey administrator software where the entire member list was randomly divided in to two samples with members of each sample receiving only one of the two surveys. The first survey was sent to sample one and investigated the use of ART in upper anterior tooth (present study), and the second sample assessed the use of ART in posterior primary teeth (will be presented in another paper).
For each patient scenario in this study, pediatric dentists rated how likely they were to use ART on a 5-point scale, ranging from 5 = “very likely to use ART” to 1 = “very unlikely to use ART.” A main effect design was used to allow estimations of the relative weights (utilities) for each level of the presented factors on the willingness to use ART score. spss conjoint software (SPSS Inc., Chicago, IL, USA) (28) was used to generate this design and carry out the analysis; Pearson's R, Kendall's tau, and Cramer's V test were used to validate the design. It is important to note that even though a subset of potential patient scenarios were randomly selected and presented to the participant (orthogonal fractional factorial design), the software algorithm is programmed to extrapolate total utility values for all possible patient scenarios for each study participant.
Through a series of linear regressions, spss conjoint used the rating of patient scenarios from each participant to generate utility scores for each attribute level. Utility scores represent participant preferences for that attribute level, with higher utility scores indicating greater preference.
The relative importance of each factor as a whole was also calculated in percentage terms based on the levels’ utilities. In addition, a logit preference probability was estimated for all cases, including the nine cases presented in the survey and the simulation cases, which were cases for patients’ scenarios that were not rated by the respondents.
Three hundred cases was considered as the minimum sample size based on previous studies using conjoint analysis; this number assumed a margin of error of 3 percent around utility values estimates and a confidence interval of 95 percent (29,30).
Response bias was checked by comparing the original sample with the entire AAPD e-mail list and by comparing the demographic data for respondents who were included in the analysis with both the original sample and the entire e-mail list.
Results
Seven hundred and twenty-three pediatric dentists completed the online survey between May and June 2011 with a response rate of 32 percent. This response rate is within the range (25-50 percent) of recent published response rates for national pediatric dentists’ surveys in the United States (31-33). For descriptive findings and ART follow-up questions, responses from the entire original sample of 723 were used. The study sample was predominantly males (58 percent), and the mean age for the sample was 48 years. Among the 723 respondents, 82 percent considered ART to be an interim treatment for the presented scenarios, and 18 percent considered ART to be a definitive treatment. Pediatric dentists cited several factors that influenced their decision regarding the therapeutic goals of ART (definitive or interim), including “caries risk of the patient (61 percent),” “depth of lesion (60 percent),” and “number of surfaces involved, single or multiple (56 percent).”
Our sample reported having learned about ART as a restorative procedure mainly from advanced pediatric training (59 percent), the scientific literature (47 percent), and AAPD policies and guidelines (46 percent). However, for the 3.5 percent of our respondents, our survey was the first time they had encountered ART.
Conjoint analyses, in assessing trade offs among factors, do not utilize data where subjects have no variation in their responses – in this case, those who would always use ART or never would use ART for all of the scenarios.In addition,con- joint analysis requires that respondents complete each scenario. Thus, data from respondents where there were no variation in how they addressed each scenario (n = 169) and for those who skipped one or more scenarios were excluded from the analyses, resulting in a final sample used in conjoint analysis of 523.
The conjoint model fit was assessed using correlation statistics that provide measures of the correlation between the observed and estimated preferences (34). For these assessments, Pearson's R was 0.97, (P < 0.000), and Kendall's tau was 0.83, (P < 0.001), both of which indicate a good fit. The conjoint design was also validated using Cramer's V test, which demonstrated only weak correlations among the three design factors (either 0 or <0.3). This is consistent with the main effects fractional factorial design selected for the study.
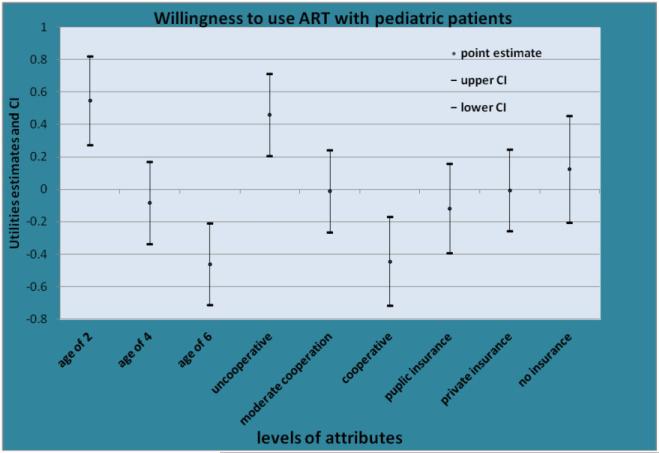
Figure 2 shows the results of the conjoint analysis demonstrating the propensity of pediatric dentists in this sample to use ART with their patients for a particular clinical presentation.Conjoint analysis in this study demonstrated that for the factor“age,”ART was preferred for patients who were“2 years old.” For the factor “cooperation,” the preferred level “unco-operative child” had a significantly higher utility or preference than the level “cooperative child.” Under the factor “insurance coverage,” the most preferred level was “without insurance”; however, this result was not significantly different than the level “public insurance” or the level “private insurance.” Confidence intervals of those utility values are presented in Figure 2.
Figure 2.
The mean utilities for each factor and their associated confidence intervals (CI).
In terms of relative importance of factors, the analysis demonstrated that the most important factor prompting pediatric dentists to use ART with their patients in this analysis was “age” (40 percent), followed by the factor “cooperation” (37 percent), with the factor “insurance coverage” (23 percent) being least important.
In addition to the previous two pieces of information, the total utility for different combinations of the levels was calculated not only for the nine patients’ scenarios presented to respondents but also for all possible 27 combinations of the factors’ levels. Among the 27 scenarios in this study, the highest total utility was for scenario #3 (a 2-year-old patient who is uncooperative and has no insurance),which had a logit probability of 9.8 percent. In contrast, the least preferred patient scenario to use ART with was #25 (a six-year-old patient who is cooperative and has public insurance) with a logit value of 1.1 percent. In other words, if the 27 patients’ scenarios were real, and the factors selected represent all the factors that may influence such a decision, most pediatric dentists thought that they would be most likely willing to treat patients using ART in scenario #3 nine times more often than for patients in scenario #25. Table 1 shows selected patients’ scenarios,their total utility values,and their logit values.
Table 1.
Examples of Patient Scenarios, the Total Utility, and Logit Values of Selected Patients’ Scenarios
| ID # of patient scenario | Patient's scenario as presented for pediatric dentists | Total utility | Logit value (%) |
|---|---|---|---|
| #1 | A 2-year-old patient who is uncooperative and has public insurance | 3.8 | 7.6 |
| #2 | A 2-year-old patient who is uncooperative and has private insurance | 3.9 | 8.6 |
| #3 | A 2-year-old patient who is uncooperative and has no insurance | 4.1 | 9.8 |
| #9 | A 2-year-old patient who is cooperative and has no insurance | 3.159 | 4.0 |
| #10 | A 4-year-old patient who is uncooperative and has public insurance | 3.189 | 4.1 |
| #12 | A 4-year-old patient who is uncooperative and has no insurance | 3.4 | 5.2 |
| #19 | A 6-year-old patient who is uncooperative and has public insurance | 2.8 | 2.8 |
| #25 | A 6-year-old patient who is cooperative and has public insurance | 1.9 | 1.1 |
| #27 | A 6-year-old patient who is cooperative and has no insurance | 2.2 | 1.4 |
Response bias was evaluated in different steps to ensure that the sample was representative of the AAPD members. The 523 eligible cases that were used in the conjoint analysis were compared with the original sample of 723 respondents and the AAPD member list by age and gender using t-test and chi-squared, and no significant statistical differences were detected.
Discussion
The literature describes substantial variation in dentists’ assessments of clinical, community, and behavioral factors that influence their decisions to provide a particular restorative treatment for their patients (21-23). The methods used to examine and report the factors influencing practitioners’ decisions to select a restorative treatment option are often complicated by constraints of the conditions under which dentists were asked to make their assessments and, thus, limit inference to other settings (10,11,35,36). In contrast, conjoint analysis allows investigators to model choices under many different scenarios, under different constraints, and across any population. As such, conjoint analysis offers a flexible mechanism for not only evaluating a current situation, but also new, future, or potential (hypothetical) situations.
This study controlled for the clinical factors that may drive most initial treatment decisions among pediatric dentists. This allowed investigation of dentists’ perception of other patient factors that may influence the decision to use ART. Such factors play an important role in marketing the use of ART as an affordable, atraumatic, and patient-friendly procedure for whom traditional dental care is not feasible (2,3). In addition, the clinical presentation that was used in this study was a good candidate for ART restoration; using ART in such a cavity has been shown to have high survival rate (4) and conforms to the American Dental Association (ADA) specification for quality restorations (3).
As predicted by the study hypothesis, the results demonstrated that pediatric dentists are more likely to use ART with young and uncooperative children. This is consistent with other studies that listed age as an important factor in practitioners’ decisions to provide restorative treatment in general (21-23) and with the AAPD guidelines that recommend the use of ART with very young children and uncooperative children, for whom the traditional restorative treatment would be difficult (9).
In contrast with other reports (21-23), where insurance coverage was usually selected by a small percentage (usually <10 percent) of respondents as a factor in restorative treatment decision making, the conjoint analysis found that its importance value was 23 percent, which suggests that although insurance was less important than the other two factors, relative to the other factors’ value, it was still of substantial importance. That is, in conjoint analysis, the meaning of the importance value is relative and not absolute, so that in this case, the importance value of “insurance status” was nearly 60 percent of the importance value of “child cooperation.” Interestingly, in the present study, when respondents were asked about the importance of different factors in their decision to use ART as definitive or interim treatment using a “check all that apply” format, “insurance status” was cited only about 10 percent as often as “cooperation.” Thus, con-joint results suggested a stronger impact of insurance than the direct ratings. However, conjoint results failed to demonstrate a statistical difference between the three levels of the factor “insurance” and suggested that pediatric dentists were equally willing to use ART with children with no insurance compared with children with private insurance or on public assistance. This may suggest that social pressure still plays a role when responding to the conjoint scenarios in this study. It would be instructive to conduct a future study where the insurance factor is embedded in a more complex design and larger number of factors to validate the results of this study.
The majority of the study sample considered ART as an interim treatment, which is consistent with our earlier work on the use of ART in pediatric dentistry training institutions, in which 57 percent of pediatric dentistry residency programs (37) and 83 percent of predoctoral pediatric dentistry programs chairs considered ART to be an interim treatment in primary teeth (38). This may be different from how ART is viewed globally as a definitive treatment (1-3), particularly in certain populations that do not have access to more traditional restorative treatment.
Although there was no response bias detected in the sample using mainly demographic data, the possibility of selection bias cannot be excluded. It seems likely that pediatric dentists who are practicing ART or are interested in this procedure may have been more likely to have answered the survey. This in turn, however, suggests the actual rate of use to be lower than estimated. Furthermore, study results are limited to the factors and levels selected to be included in the hypothetical scenarios. Deciding on the number of factors and levels to be included in the conjoint design is one of the major challenges to produce a feasible design that achieves statistical efficiency but at the same time does not overwhelm the respondent. This required the options included in the patients’ scenarios to be realistic and important contextual factors to be included in the model (34).
The present study suggests the feasibility of using techniques borrowed from marketing research such as conjoint analysis to assess dentists’ restorative treatment decisions. However, future research is needed to validate this conclusion. This may be achieved by asking questions on a variety of restorative modalities and assessing the relative importance practitioners place on different factors in a variety of patient situations.
Although insurance coverage was the least important among the factors, being without insurance, being very young,and being uncooperative was the scenario where pediatric dentists most favored ART when making trade offs between different factors using the conjoint design.
Acknowledgment
This project was funded by NIH/NIDC R T32 grant DEO 14678-06.
References
- 1.Frencken JE, Coelho S. The correct use of the ART approach. J Appl Oral Sci. 2010;18(1):1–4. doi: 10.1590/S1678-77572010000100002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Frencken JE, Pilot T, Songpaisan Y, Phantumvanit P. Atraumatic restorative treatment (ART): rationale, technique, and development. J Public Health Dent. 1996;56:135–40, 161-3. doi: 10.1111/j.1752-7325.1996.tb02423.x. [DOI] [PubMed] [Google Scholar]
- 3.Frencken JE. The ART approach using glass-ionomer in relation to global oral health care. Dent Mater. 2010;26(1):1–6. doi: 10.1016/j.dental.2009.08.013. [DOI] [PubMed] [Google Scholar]
- 4.Van't Hof MA, Frencken JE, van Palenstein Helderman WH, Holmgren CJ. The Atrumatic Restorative treatment (ART) approach for managing dental caries: a meta-analysis. Int Dent J. 2006;56:345–51. doi: 10.1111/j.1875-595x.2006.tb00339.x. [DOI] [PubMed] [Google Scholar]
- 5.Carvalho TS, Ribeiro TR, Bönecker M, Pinheiro ECM, Colares V. The atraumatic restorative treatment approach: an “atraumatic” alternative. Med Oral Patol Oral Cir Bucal. 2009;14:668–73. [PubMed] [Google Scholar]
- 6.de Amorim RG, Leal SC, Frencken JE. Survival of atraumatic restorative treatment (ART) sealants and restorations: a meta-analysis. Clin Oral Investig. 2012;16(2):429–41. doi: 10.1007/s00784-011-0513-3. doi: 10.1007/s00784-011-0513-3; [Epub 2011 Jan 28] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mickenautsch S, Yengopal V, Banerjee A. Atraumatic restorative treatment versus amalgam restoration longevity: a systematic review. Clin Oral Investig. 2010;14(3):233–40. doi: 10.1007/s00784-009-0335-8. doi: 10.1007/s00784-009-0335-8; [Epub 2009 Aug 18] [DOI] [PubMed] [Google Scholar]
- 8.Estupinan-Day S, Milner T, Tellez M. Final report. Pan American Health Organization; Washington, DC: 2006. Oral health of low-income children: procedures for atraumatic restorative treatment. [Google Scholar]
- 9.American Academy of Pediatric dentistry. Policy on Interim therapeutic treatment. 2009 [Google Scholar]
- 10.Ryan M, Scott D, Reeves C, Bate A, van Teijlingen E, Russell E, Napper M, Robb C. A review of quantitative techniques for eliciting public views. Health Technol Assess. 2001;5(5):1–186. doi: 10.3310/hta5050. [DOI] [PubMed] [Google Scholar]
- 11.Koele P, Hoogstraten J. Determinants of dentists’ decisions to initiate dental implant treatment: a judgment analysis. J Prosthet Dent. 1999;81(4):476–80. doi: 10.1016/s0022-3913(99)80017-1. [DOI] [PubMed] [Google Scholar]
- 12.Chakraborty G, Gaeth GJ, Cunningham M. Understanding consumers’ preferences for dental service. J Health Care Mark. 1993;13(3):48–58. [PubMed] [Google Scholar]
- 13.Cunnigham M, Gaeth G, Juang C, Chakraborty G. Using choice-based conjoint to determine the relative importance of dental benefit plan attributes. J Dent Educ. 1999;63(5):391–9. [PubMed] [Google Scholar]
- 14.Vick S, Scott A. Agency in health care. examining patients’ preferences for attributes of the doctor–patient relationship. J Health Econ. 1998;17(5):587–605. doi: 10.1016/s0167-6296(97)00035-0. [DOI] [PubMed] [Google Scholar]
- 15.Ryan M, Hughes J. Using conjoint analysis to assess women's preferences for miscarriage management. Health Econ. 1997;6(3):261–73. doi: 10.1002/(sici)1099-1050(199705)6:3<261::aid-hec262>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 16.Ryan M. A role for conjoint analysis in technology assessment in health care? Int J Technol Assess Health Care. 1999;15(3):443–57. [PubMed] [Google Scholar]
- 17.Van der Pol M, Cairns J. Establishing preferences for blood transfusion support: an application of conjoint analysis. J Health Services Res Manage. 1998;3:70–6. doi: 10.1177/135581969800300203. [DOI] [PubMed] [Google Scholar]
- 18.Derek S, Brown F, Johnson R, Poulos C, Messonnier M. Mothers’ preferences and willingness to pay for vaccinating daughters against human papillomavirus. Vaccine. 2010;28(7):1702–8. doi: 10.1016/j.vaccine.2009.12.024. [DOI] [PubMed] [Google Scholar]
- 19.Bridges J, Hauber AB, Marshall D, Lloyd A, Prosser L, Regier D, Johnson F, Mauskopf J. Conjoint analysis applications in health – a checklist: a report of the ispor good research practices for conjoint analysis task force. Value Health. 2011;14(4):403–13. doi: 10.1016/j.jval.2010.11.013. [DOI] [PubMed] [Google Scholar]
- 20.Cunningham C, Deal K, Rimas H, Chen Y, Buchanan D, Sdao-Jarvie K. Providing information to parents of children with mental health problems: a discrete choice analysis of professional preferences. J Abnorm Child Psychol. 2009;37(8):1089–102. doi: 10.1007/s10802-009-9338-9. [DOI] [PubMed] [Google Scholar]
- 21.Bader J, Shugars D. What do we know about how dentists make caries-related treatment decisions? Community Dent Oral Epidemiol. 1997;25(1):97–103. doi: 10.1111/j.1600-0528.1997.tb00905.x. [DOI] [PubMed] [Google Scholar]
- 22.Bader J, Shugars D. Understanding dentists’ restorative treatment decisions. J Public Health Dent. 1992;52(2):102–10. doi: 10.1111/j.1752-7325.1992.tb02251.x. [DOI] [PubMed] [Google Scholar]
- 23.Brennan DS, Spencer AJ. The role of dentist, practice and patient factors in the provision of dental services. Community Dent Oral Epidemiol. 2005;33:181–95. doi: 10.1111/j.1600-0528.2005.00207.x. [DOI] [PubMed] [Google Scholar]
- 24.Originating Committee, Clinical Affairs Committee – Behavior Management Subcommittee Guideline on Behavior Guidance for the Pediatric Dental Patient. REFERENCE MANUAL V 35/nO. 6 13/14. Adopted 1990, Revised 2011. Available from: http://www.aapd.org/media/Policies_Guidelines/G_BehavGuide.pdf.
- 25.Doméjean-Orliaguet S, Léger S, Auclair C, Gerbaud S, Tubert-Jeannin L. Caries management decision: influence of dentist and patient factors in the provision of dental services. J Dent. 2009;37(11):827–34. doi: 10.1016/j.jdent.2009.06.012. [DOI] [PubMed] [Google Scholar]
- 26.Manski RJ, Brown E. Statistical Brief 221. Agency for Health Care Research and Quality; Rockville. MD: Sep, 2008. Dental coverage of children and young adults under age 21, United States, 1996 and 2006. 2008. Available from: http://meps.ahrq.gov/data_files/publications/st221/stat221.pdf. [Google Scholar]
- 27.Manski RJ, Brown E. Dental use, expenses, private dental coverage, and changes, 1996 and 2004. Agency for Healthcare Research and Quality; Rockville: 2007. MEPS Chartbook No.17. Available from: http://www.meps.ahrq.gov/mepsweb/data_files/publications/cb17/cb17.pdf. [Google Scholar]
- 28.SPSS Inc. PASW Statistics for Windows,Version 18.0. SPSS Inc.; Chicago: 2009. [Google Scholar]
- 29.Ryan M, Bate A, Eastmond CJ, Ludbrook A. Use of discreet choice experiments to elicit preferences. Qual Health Care. 2001;10(Suppl. 1):i55–60. doi: 10.1136/qhc.0100055... [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Orme B. Getting started with conjoint analysis: strategies for product design and pricing research. 2nd ed. Research Publishers LLC; Madison: 2010. [Google Scholar]
- 31.Weil TN, Inglehart MR. Pediatric dentists’ behavior management of children with autism spectrum disorders. J Dent Educ. 2010;74(12):1294–307. [PubMed] [Google Scholar]
- 32.Tellez M, Gray SL, Gray S, Lim S, Ismail AI. Sealants and dental caries, Dentists’ perspectives on evidence-based recommendations. J Am Dent Assoc. 2011;142(9):1033–40. doi: 10.14219/jada.archive.2011.0324. [DOI] [PubMed] [Google Scholar]
- 33.Oueis HS, Ralstrom E, Miriyala V, Molinari GE, Casamassimo P. Alternatives for hand over mouth exercise after its elimination from the clinical guidelines of the American Academy of Pediatric Dentistry. Pediatr Dent. 2010;32(3):223–8. [PubMed] [Google Scholar]
- 34.Orme BK. Getting started with conjoint analysis: strategies for product design and pricing research. Research Publishers, LLC; Madison: 2006. [Google Scholar]
- 35.Louviere JJ, Henley DH, Woodworth G, Meyer RJ, Levin IP, Stoner JW, Curry D, Anderson DA. Laboratory simulation versus revealed preference methods for estimating travel demand models: an empirical comparison. Trans Res Rec. 1981;79:42–51. [Google Scholar]
- 36.Ryan M, Shelley Farrar S. Using conjoint analysis to elicit preferences for health care. BMJ. 2000;320(7248):1530–3. doi: 10.1136/bmj.320.7248.1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kateeb E, Warren J, Momany E, Kanellis M, Damiano P, Weber-Gasparoni K, Ansley T. Atraumatic restorative treatment (ART) in pediatric dentistry residency programs: a survey of program directors. Pediatr Dent. 2013;35(7):500–5. [PubMed] [Google Scholar]
- 38.Kateeb ET, Warren JJ, Damiano P, Momany E, Kanellis M, Weber-Gasparoni K, Ansley T. Teaching atraumatic restorative treatment (ART) in U.S. dental schools: a survey of pre-doctoral pediatric dentistry program directors. J Dent Educ. 2013;77(10):1306–14. [PubMed] [Google Scholar]