Abstract
Purpose
To evaluate minimum 5-year follow-up clinical and radiological results of total knee arthroplasty (TKA) using a posterior cruciate ligament sacrificing (PS), non-substituting Advance Medial Pivot Knee.
Materials and Methods
One hundred and twenty knees in 80 patients who could be followed up for more than 5 years after TKA using the PS Advance Medial Pivot Knee were evaluated retrospectively. The evaluations included the preoperative and postoperative range of motion (ROM), tibiofemoral angle, Knee Society (KS) knee and function scores, and Western Ontario and McMaster Universities Arthritis Index (WOMAC) score. The Kaplan-Meier method was used for survival analysis.
Results
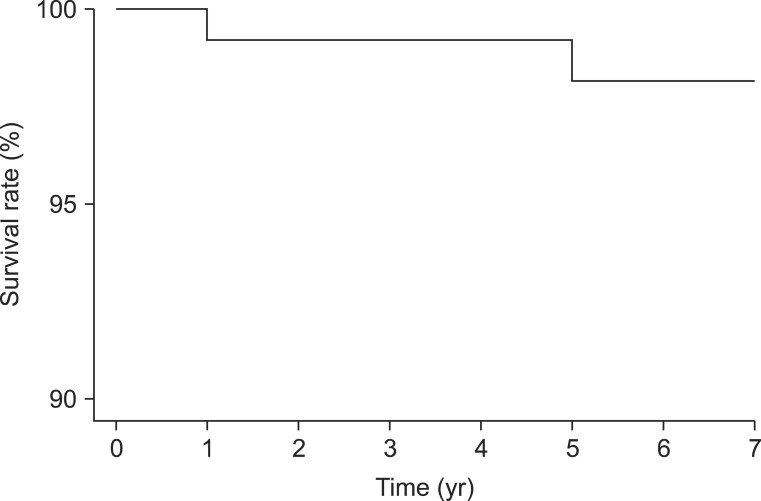
The ROM increased from a preoperative mean flexion contracture of 7.6° and further flexion of 115.1° to a postoperative mean flexion contracture of 1.5° and further flexion of 120.5°. The tibiofemoral angle was changed from 4.6° varus preoperatively to 5.8° valgus postoperatively. The KS knee and function scores as well as WOMAC score significantly improved after surgery (p<0.05). Complications developed in 4 cases (3.3%): 2 cases of periprosthetic patellar fracture (1.7%) and 2 cases of aseptic loosening (1.7%). The seven-year survival rate was 98.1% in the Kaplan-Meier survival analysis.
Conclusions
The minimum 5-year follow-up results of TKA using the PS Medial Pivot Knee were satisfactory.
Keywords: Knee, Arthroplasty, Medial Pivot
Introduction
The Advance Medial Pivot Knee (Wright Medical Technology Inc., Memphis, TN, USA) was designed to reproduce the kinematics of the medial pivot motion in the normal knee1,2,3,4,5). The medial compartment of the prosthesis has ball-in-socket geometry to improve joint congruity for stability and the lateral compartment allows for rolling and gliding during knee flexion as in the intact knee6,7,8,9). Other major benefits of the prosthesis include reduced incidences of condylar lift-off and polyethylene wear due to the improved conformity of the polyethylene insert6,10). However, the influence of such biomechanical characteristics of the Advance Medial Pivot Knee on patient satisfaction and implant survivorship has not been sufficiently investigated in studies. Long-term studies have never been published and short-term or mid-term follow-up studies are rare11,12,13).
In this study, we investigated the clinical and radiological results and complications of total knee arthroplasty (TKA) using the Advance Medial Pivot Knee for a minimum follow-up of 5 years under the hypothesis that the posterior cruciate ligament sacrificing, non-substituting (PS) implant designed to replicate the medial pivot motion in the non-arthritic knee would yield satisfying functional improvement without significant complications.
Materials and Methods
1. Study Population
Of the patients who had undergone TKA using the PS Advance Medial Pivot Knee between October 2004 and December 2006, 80 patients (120 knees) who were available for more than 5-year follow-up were retrospectively reviewed. There were 9 males (15 knees) and 71 females (105 knees). Their mean age at the time of surgery was 66.4 years (range, 42 to 83 years). The mean follow-up period was 64.7 months (range, 60 to 86 months). The preoperative diagnosis was osteoarthritis in 108 knees (90.0%), rheumatoid arthritis in 4 knees (3.3%), and osteonecrosis in 8 knees (6.7%).
The indications for surgery were defined as severe pain or difficulty in performing daily living activities without any improvement with conservative therapy, Kellgren-Lawrence grade 3 or 4 in cases of patients ≥65 years of age, and Kellgren-Lawrence grade 4 in cases of patients with <65 years of age. The number of patients aged ≤60 years was 24, 20 of which had osteoarthritis and the remaining 4 had rheumatoid arthritis.
2. Surgical Techniques and Postoperative Treatment
All the operations were performed by the same surgeon. After a midline skin incision, limited medial parapatellar arthrotomy was performed and traditional sequential medial release was carried out. The anterior and posterior cruciate ligaments were removed in all knees. The distal femoral cut was performed using an intramedullary alignment guide and the proximal tibial cut was done using an extramedullary alignment guide. The femoral component was placed in a 3° externally rotated position with reference to the posterior condylar axis. In order to maintain the medial pivot motion during flexion and extension, care was taken not to cause excessive release of the medial collateral ligament (MCL). However, if an unavoidable excessive ligament release in the case of varus knee results in a ≥3 mm medial gap, the ligament was sutured to the pes anserinus attachment site after implant insertion to maintain proper tension for <2-3 mm medial gap during flexion. The MCL suturing was required in 11 knees in whom the postoperative rehabilitation regimen was identical to that in the other patients. The medial/lateral ligament balance and flexion/extension gap balance were adjusted to confirm the absence of abnormal findings on the valgus/varus stress test, the ability to get full knee extension, and absence of medial/lateral laxity or lift off of a trial component during flexion. The femoral and tibial components were fixed with cement in all patients. Patellar resurfacing was selectively performed: the patella was resurfaced in all knees with rheumatoid arthritis and in all of the remaining knees except for 16 knees with relatively good articular surface. Immediately after surgery, patients were allowed to undertake quadriceps strengthening exercises and active straight leg-raising as instructed prior to surgery. On the first postoperative day, continuous passive motion exercises were initiated. At 3-4 days after surgery, when straight leg-raising could be performed without difficulty, progressive weight bearing was started with an assistance of a walker or a cane.
3. Clinical and Radiological Evaluation
Clinical evaluation was based on the pre- and postoperative range of motion (ROM), Knee Society (KS) knee score and function score, Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score, and postoperative complications. The maximum further flexion without pain was measured in supine position using a goniometer. On the radiological evaluation, the standing anteroposterior view and the 30° flexion lateral view taken at the last follow-up were assessed according to the American Knee Society Roentgenographic Evaluation system. In particular, fluoroscopy was used to determine the appearance of radiolucency around the femoral and tbial components. The femorotibial angle (Ω) change was measured. To assess the implant position, the valgus angle of the femoral component (α) and the varus angle of the tibial component (β) were measured on the anteroposterior view and the flexion angle of the femoral component (γ) and the posterior slope of the tibial component (δ) were measured on the lateral view. The Kaplan-Meier method was used for survival analysis with revision or the need for revision defined as failure.
4. Statistical Analysis
The paired t-test was used to determine the significance of clinical results and changes in the femorotibial angle. Statistical analysis was done using the SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA) with a significance level set at p<0.05.
Results
There was significant improvement in the ROM between the preoperative and last follow-up assessments: the mean flexion contracture decreased from 7.6° to 1.5° and the mean range of further flexion increased from 115.1° (ROM, 107.5°) to 120.5° (ROM, 119°) (p<0.05). The KS knee score and function score, and the WOMAC score for pain and stiffness and function were significantly improved (p<0.05) (Table 1).
Table 1.
Clinical Results

Values are presented as mean (range).
WOMAC: Western Ontario and McMaster Universities Osteoarthritis Index.
The femorotibial angle was improved from a mean of 4.6°±4.5° varus preoperatively to a mean of 5.8°±2.4° valgus postoperatively. The mean α, β, γ and δ angle were 96.2°±2.1°, 89.1°±1.7°, 2.5°±1.5° and 84.4°±2.7°, respectively. Except for 2 cases of aseptic loosening, ≥2 mm radiolucency was not observed in any case when assessed according to the American Knee Society Roentgenographic Evaluation system (Table 2).
Table 2.
Zonal Distribution of Radiolucency at Bone-cement Interfaces

Complications occurred in 4 knees (3.3%): periprosthetic patellar fracture in 2 (1.7%) and aseptic loosening in 2 (1.7%). There was no case of infection. Periprosthetic patellar fractures were caused by aggressive flexion exercises in one and by trauma in the other. Conservative treatment for the former with no displacement and open reduction and internal fixation using tension band wiring for the latter resulted in satisfactory outcomes. Aseptic tibial component loosening was observed at 1 year and 9 months after surgery in one knee, which was revised using structural allograft and stemmed tibial component (Fig. 1). Aseptic loosening in the other case was observed at 5 years and 7 months after surgery, and the plain radiography revealed osteolysis in the femur and aseptic loosening in the tibia. The patient declined revision surgery and has been under observation (Fig. 2). The 7-year survival rate according to the Kaplan-Meier method was 98.1% (95% confidence interval, 0.96 to 1.00) (Fig. 3).
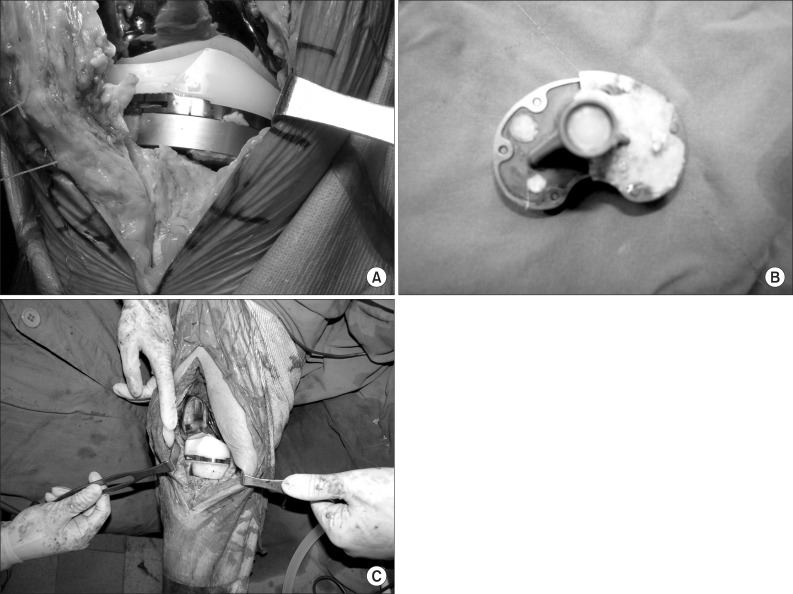
Fig. 1.
(A) Early failure of the tibial component was observed intraoperatively. (B) The tibial component was removed. (C) Revision total knee arthroplasty was performed using a stemmed tibial component and a structural allograft.
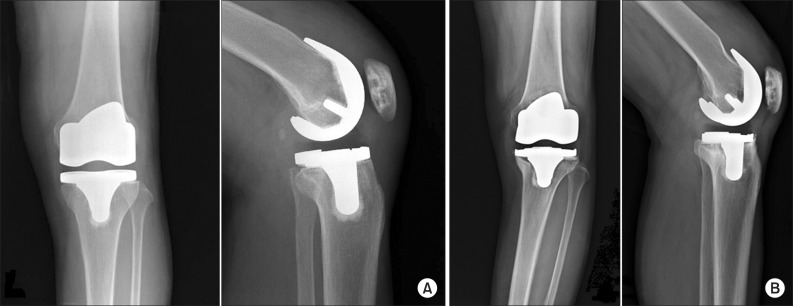
Fig. 2.
(A) Anteroposterior (AP) and lateral radiographs were taken immediately postoperatively. (B) AP and lateral radiographs taken at postoperative 67 months show aseptic loosening of the tibial component and osteolysis of the femoral component.
Fig. 3.
Kaplan-Meier survival curve of the Medial Pivot Knee prosthesis.
Discussion
The clinical and radiological results of TKA using the PS Advance Medial Pivot Knee were satisfactory without significant complications after the minimum 5-year mid-term follow-up. The significance of this study can be found in the fact that the mid-term results of Advance Medial Pivot Knee in TKA have never been addressed in domestic studies and our results were comparable to those described in international mid-term follow-up studies11,12,13).
Fan et al.11) reported minimum 5-year follow-up results of 58 medial pivot TKAs: the mean ROM was improved from 103.5° preoperatively to 115.4° at the last follow-up; non-progressive radiolucent lines were observed in only 2 cases; and there was no case of revision for loosening. In a mean 6.7-year follow-up study by Karachalios et al.12), the mean ROM was improved from 101° preoperatively to 117° at the last follow-up and the 5-year survival rate and 9-year survival rate were 99.1% and 97.5%, respectively. Component loosening occurred in 2 active obese patients (1%). Vecchini et al.13) followed 160 patients (172 knees) for a mean of 7 years after medial pivot TKA: the mean ROM was improved from 97.7° preoperatively to 112.5° at the last follow-up and the survival rate was 98.6%. In our mean 6.1-year follow-up study, the mean ROM was improved from 107.5° preoperatively to 119° at the last follow-up, showing more favorable results than the above-mentioned studies. The 7-year survival rate (98.1%) was comparable to that of Vecchini et al.13).
In our study, significant clinical improvement was noted in all patients after TKA using the PS Advance Medial Pivot Knee. Although we used the PS type implant in all knees during TKA, there are some studies providing comparisons with other types of implants. Bae et al.14) reported there was no notable difference in the clinical and radiological results of TKA between the cruciate retaining (CR) type Advance Medial Pivot Knee group (67 cases) and the PS type group (70 cases). Pritchett15) investigated patient preferences in knee prostheses for a mean of 7 years after bilateral TKA: 77% of the 344 patients preferred the medial pivot knee prosthesis to other PS type prostheses. Youm et al.16) showed that the minimum 2-year follow-up results of TKA using the PS type Advance Medial Pivot Knee were comparable to those of TKA using the Nexgen LPS system. On the other hand, Kim et al.17) reported that the satisfaction rate in the CR type Advance Medial Pivot Knee group was significantly low compared to that in the PFC sigma mobile-bearing prosthesis group and the complication rate was remarkably higher in the former group during the mean 2.6-year follow-up. However, we believe their results should be interpreted with caution because it is difficult to associate the complications occurred in their patients (infection, persistent flexion contracture, and constant swelling) with the design features of the implant.
Most PS type implants necessitate an extensive box cutting to enable the cam-post mechanism. However, the PS type Advance Medial Pivot Knee does not require box cutting because the ultracongruent polyethylene insert that has no post provides anteroposterior stability. Accordingly, considering that more bone stock preservation would be of benefit for possible revisions, we preferred to use the Advance Medial Pivot Knee in young patients with a relatively high likelihood of revision, if they met the indications. This is why relatively young patients ≤60 years of age (19 patients, 24 knees) were included in the study. However, we believe long-term follow-up studies should be conducted to assess the influence of bone stock preservation in the box of the femur on future revision surgery.
Of the 2 cases of aseptic loosening, the early loosening of the tibial component in one knee can be attributed to surgical errors: 2° of varus cutting of the proximal tibia. In addition, the use of a 10-mm metal augment without a stem for proximal tibial bone loss may have resulted in increased stress in the medial aspect of the proximal tibia, eventually resulting in subsidence of the medial tibia and tibial component loosening. Regarding the other case in which osteolysis of the femur and aseptic loosening of the tibia were found at 5 years and 7 months after surgery, it is difficult to identify whether the complications were associated with the ultracongruent design of the Advance Medical Pivot knee. Rather, Minoda et al.10) reported that the medial pivot knee prosthesis caused significantly less wear particles than other PS type prostheses. In the other aforementioned mid-term follow-up studies, the incidences of osteolysis and loosening were not significantly high in the knees with medial pivot knee prostheses. Thus, we believe this should be elucidated in further long-term follow-up biomechanical studies.
One of the limitations of this study is that due to the retrospective study design, the level of evidence was relatively low compared to prospective studies. In addition, the number of cases was small and the follow-up was not maintained for the long term. Finally, the study did not examine whether replication of medial pivoting, the biomechanical advantage of the medial pivot knee, was successfully realized after TKA.
Conclusions
The clinical and radiological results of TKA using the PS Advance Medial Pivot Knee designed to reproduce normal knee kinematics were satisfactory after the minimum 5-year mid-term follow-up. And the incidence of tibial component loosening after using this ultracongruent implant was not remarkable.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Banks SA, Hodge WA. Accurate measurement of three-dimensional knee replacement kinematics using single-plane fluoroscopy. IEEE Trans Biomed Eng. 1996;43:638–649. doi: 10.1109/10.495283. [DOI] [PubMed] [Google Scholar]
- 2.Blaha JD, Mancinelli CA, Simons WH, Kish VL, Thyagarajan G. Kinematics of the human knee using an open chain cadaver model. Clin Orthop Relat Res. 2003;(410):25–34. doi: 10.1097/01.blo.0000063564.90853.ed. [DOI] [PubMed] [Google Scholar]
- 3.Hoff WA, Komistek RD, Dennis DA, Gabriel SM, Walker SA. Three-dimensional determination of femoral-tibial contact positions under in vivo conditions using fluoroscopy. Clin Biomech (Bristol, Avon) 1998;13:455–472. doi: 10.1016/s0268-0033(98)00009-6. [DOI] [PubMed] [Google Scholar]
- 4.Iwaki H, Pinskerova V, Freeman MA. Tibiofemoral movement 1: the shapes and relative movements of the femur and tibia in the unloaded cadaver knee. J Bone Joint Surg Br. 2000;82:1189–1195. doi: 10.1302/0301-620x.82b8.10717. [DOI] [PubMed] [Google Scholar]
- 5.Mahfouz MR, Hoff WA, Komistek RD, Dennis DA. A robust method for registration of three-dimensional knee implant models to two-dimensional fluoroscopy images. IEEE Trans Med Imaging. 2003;22:1561–1574. doi: 10.1109/TMI.2003.820027. [DOI] [PubMed] [Google Scholar]
- 6.Schmidt R, Komistek RD, Blaha JD, Penenberg BL, Maloney WJ. Fluoroscopic analyses of cruciate-retaining and medial pivot knee implants. Clin Orthop Relat Res. 2003;(410):139–147. doi: 10.1097/01.blo.0000063565.90853.a4. [DOI] [PubMed] [Google Scholar]
- 7.Blaha JD. A medial pivot geometry. Orthopedics. 2002;25:963–964. doi: 10.3928/0147-7447-20020901-32. [DOI] [PubMed] [Google Scholar]
- 8.Miyazaki Y, Nakamura T, Kogame K, Saito M, Yamamoto K, Suguro T. Analysis of the kinematics of total knee prostheses with a medial pivot design. J Arthroplasty. 2011;26:1038–1044. doi: 10.1016/j.arth.2010.08.015. [DOI] [PubMed] [Google Scholar]
- 9.Omori G, Onda N, Shimura M, Hayashi T, Sato T, Koga Y. The effect of geometry of the tibial polyethylene insert on the tibiofemoral contact kinematics in Advance Medial Pivot total knee arthroplasty. J Orthop Sci. 2009;14:754–760. doi: 10.1007/s00776-009-1402-3. [DOI] [PubMed] [Google Scholar]
- 10.Minoda Y, Kobayashi A, Iwaki H, Miyaguchi M, Kadoya Y, Ohashi H, Yamano Y, Takaoka K. Polyethylene wear particles in synovial fluid after total knee arthroplasty. Clin Orthop Relat Res. 2003;(410):165–172. doi: 10.1097/01.blo.0000063122.39522.c2. [DOI] [PubMed] [Google Scholar]
- 11.Fan CY, Hsieh JT, Hsieh MS, Shih YC, Lee CH. Primitive results after medial-pivot knee arthroplasties: a minimum 5-year follow-up study. J Arthroplasty. 2010;25:492–496. doi: 10.1016/j.arth.2009.05.008. [DOI] [PubMed] [Google Scholar]
- 12.Karachalios T, Roidis N, Giotikas D, Bargiotas K, Varitimidis S, Malizos KN. A mid-term clinical outcome study of the Advance Medial Pivot knee arthroplasty. Knee. 2009;16:484–488. doi: 10.1016/j.knee.2009.03.002. [DOI] [PubMed] [Google Scholar]
- 13.Vecchini E, Christodoulidis A, Magnan B, Ricci M, Regis D, Bartolozzi P. Clinical and radiologic outcomes of total knee arthroplasty using the Advance Medial Pivot prosthesis. A mean 7 years follow-up. Knee. 2012;19:851–855. doi: 10.1016/j.knee.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 14.Bae DK, Song SJ, Cho SD. Clinical outcome of total knee arthroplasty with medial pivot prosthesis a comparative study between the cruciate retaining and sacrificing. J Arthroplasty. 2011;26:693–698. doi: 10.1016/j.arth.2010.04.022. [DOI] [PubMed] [Google Scholar]
- 15.Pritchett JW. Patient preferences in knee prostheses. J Bone Joint Surg Br. 2004;86:979–982. doi: 10.1302/0301-620x.86b7.14991. [DOI] [PubMed] [Google Scholar]
- 16.Youm YS, Cho SD, Jeong JY, Jeon HM, Shin SM. A comparison of the short-term results between the PCL sacrificing Medial Pivot Knee and Nexgen LPS total knee arthroplasty. J Korean Knee Soc. 2010;22:175–182. [Google Scholar]
- 17.Kim YH, Yoon SH, Kim JS. Early outcome of TKA with a medial pivot fixed-bearing prosthesis is worse than with a PFC mobile-bearing prosthesis. Clin Orthop Relat Res. 2009;467:493–503. doi: 10.1007/s11999-008-0221-8. [DOI] [PMC free article] [PubMed] [Google Scholar]