Abstract
Purpose
To compare the retinal sensitivity measurements obtained with two microperimeters, the Micro-Perimeter 1 (MP-1) and the Optos optical coherence tomography (OCT)/scanning laser ophthalmoscope (SLO) in subjects with and without maculopathies.
Methods
Forty-five eyes with no known ocular disease and 47 eyes with maculopathies were examined using both microperimeters. A contrast-adjusted scale was applied to resolve the different stimuli and background luminance existing between the two devices.
Results
There was a strong ceiling effect with the MP-1 in the healthy group, with 90.1% (1136 of 1260) test points clustered at 20 dB. The mean sensitivity for the corresponding points in the OCT/SLO was 25.8 ± 1.9 dB. A floor effect was also observed with the OCT/SLO in the maculopathy group with 9.7% (128 of 1316) points clustered at 9-dB values. The corresponding mean sensitivity in the MP-1 was 1.7 ± 3.9 dB. A regression equation between the two microperimeters was established in the common 10 to19 dB intervals as: OCT/SLO = 15.6 + 0.564 × MP-1 − 0.009 × MP-12 + k (k is an individual point constant; MP-1 coefficient P < 0.001; MP-12 coefficient P = 0.006).
Conclusion
The OCT/SLO and the MP-1 provide two different ranges of contrasts for microperimetry examination. Broadening the dynamic range may minimize the constraint of the ceiling and floor effect. There is a significant mathematical relationship in the common interval of the contrast scale.
Translational Relevance
Applying a unified and broadened dynamic range in different types of microperimeters will help to generate consistent clinical reference for measurements.
Keywords: retinal sensitivity, microperimetry, comparison
Introduction
Visual acuity (VA), the gold standard for assessing visual function in clinical practice, may not fully portray visual function.1,2 Besides VA, several validated psychophysical measurements such as the Amsler grid testing, contract sensitivity,3,4 along with the electrophysiological methods, such as electroretinography (ERG),5 electro-oculography (EOG),6,7 and visual evoked potential (VEP) testing8 have been used additionally to access retinal function. However, these examinations do not provide the correlation between functional defects and retinal morphological changes.
Fundus-related perimetry, also known as microperimetry, has been clinically implemented to achieve a precise correlation between retinal pathologies and functional defects by allowing simultaneous fundus observation and compensation of eye movements during the retinal sensitivity examination.9
Since its invention, microperimetry has been widely applied in analyzing characteristics of various macular disorders, including common pathologies like diabetic retinopathy,10–12 uveitic macular edema,13 age-related macular degeneration (AMD)14,15 and even rare pathologies such as Stargardt's disease,16 and North Carolina macular dystrophy (MCDR1).17 It also has been employed in evaluating various pharmacological therapies and surgical procedures, such as anti–vascular endothelial growth factor treatment for neovascular AMD,18,19 laser photocoagulation therapy for diabetic macular edema,20 pars plana vitrectomy for macular holes,21 among others.
The microperimetry technology has rapidly progressed over the past 30 years. The first microperimeter became available in 1982 and was manufactured by Rodenstock Instruments (Munich, Germany) under the name of scanning laser ophthalmoscope (SLO101). Although it was the first time the fundus observation was provided by a perimeter, it had the inconvenience of semi-automated stimulus presentation and no eye-track system.22 The device had its marketing discontinued 2 decades later. In 2003, Nidek Technologies (Padova, Italy) introduced the Micro Perimeter 1 (MP-1) microperimeter that uses a liquid crystal display (LCD) to project the stimuli, SLO scans for fundus observation, a fundus camera to capture fundus images and automated real-time fundus tracking.23 The device was the first to employ a true eye-track system. Three years later, OPKO/OTI (OPKO Instrumentation, Miami, FL) also introduced its new microperimeter, the Spectral optical coherence tomography (Spectral OCT)/SLO, which offers the advantage of correlating functional deficits not only with SLO infrared images (retinal en face images), but also with bidimensional, cross-sectional OCT retinal images.24 In 2012, the OPKO technology was transferred to OPTOS Inc. and the Spectral OCT/SLO was renamed OPTOS OCT/SLO.
Developed on the basis of the conventional perimetry, the MP-1 has an LCD with set luminance similar to the background luminance used in Octopus perimeters (Haag-Streit AG, Koeniz, Switzerland), 1.27 cd/m2 (4 abs), and the OCT/SLO has as LCD set luminance of 10 cd/m2 (31 abs), similar to Humphrey perimeters (Carl Zeiss Meditec, Jena, Germany).25,26 In both microperimeters, the stimulus intensity varies in 1 dB (0.1 log) steps from 0 to 20 dB, where 0 dB represents the brightest luminance of 127 cd/m2 in the MP-1 and 125 cd/m2 in the OCT/SLO.27,28 With the different working parameters, the outputs of the two devices are not usually the same.
Since microperimetry has been used increasingly in clinical care,29 direct comparison between microperimeters becomes of paramount importance to further understand the psychophysics behind the microperimetry tests and interpretation of the results as well as interchangeable use of different machines. The primary aim of the index study is to evaluate the relationship between the MP-1 and the OCT/SLO microperimeter and provide a better understanding of retinal function through comprehensive information obtained from both devices.
Methods
Participants
In this prospective study, the inclusion criteria for healthy subjects were best-corrected VA greater than or equal to 20/20, refractive errors within ±6.00 diopter (D) sphere and ±1.00 D cylinder and no history of ocular diseases. Participants in maculopathy group should have no more than one diagnosis of retinal disease involving the macula in the study eye. The type of macular disease was not specified as a criterion, so maculopathy may include diabetic macular edema, central serous retinopathy, idiopathic macular hole, AMD, and so on.
The study followed the tenets of the Declaration of Helsinki and was approved by the Johns Hopkins institutional review board/ethics committee. Informed consent was obtained from all subjects.
Methods
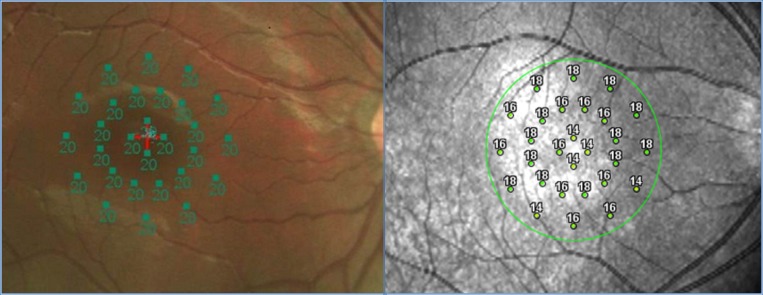
Microperimetry tests were performed in random order on all participants using both MP-1 and OCT/SLO. Important hardware features and software parameters applied in this study is summarized in Table 1. The test pattern was Polar 3 (Fig. 1). The sensitivity values of both microperimeters were compared for each of the 28 corresponding points.
Table 1.
Main testing parameters of the OCT/SLO and the MP-1
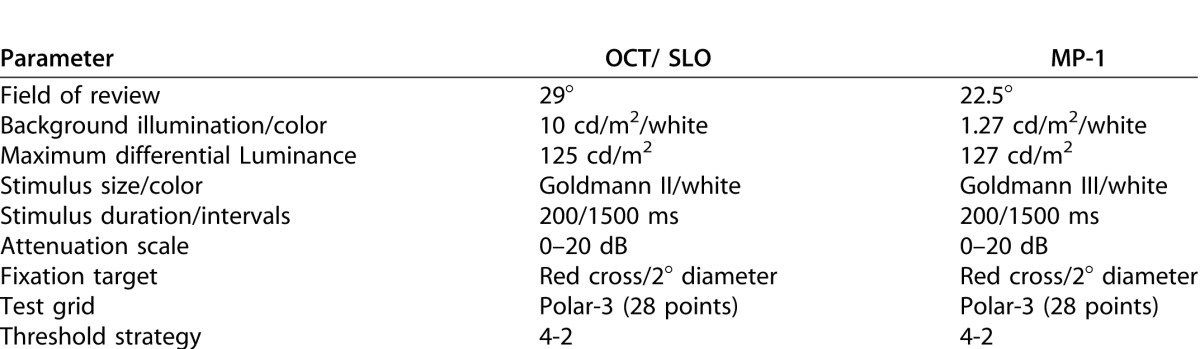
Figure 1.
The Polar 3 pattern consists of a total of 28 points located in three concentric rings centered on the fovea. The inner ring consisted of 4 points; the middle ring and the outer ring consisted of 12 points (2.3°, 6.6°, and 11° in diameter, respectively). Each value of the 28 points represents the light sensitivity for the corresponding retinal area. The sensitivity scale ranged from 0 dB (lowest sensitivity) to 20 dB (highest sensitivity).
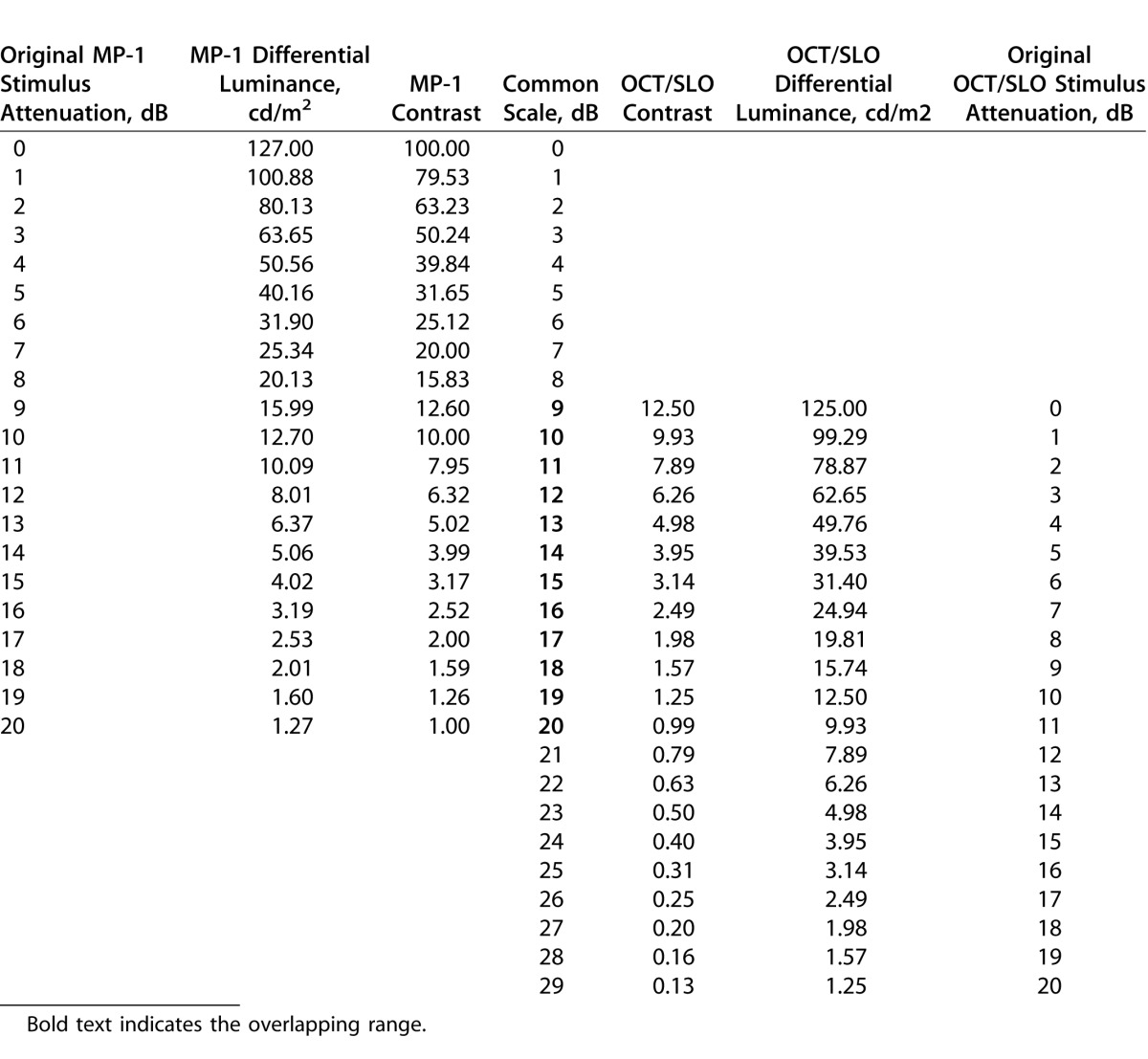
With different background luminance (1.27 cd/m2 for MP-1; 10 cd/m2 for OCT/SLO), the contrast is 1:1 at 20 dB for the MP-1 scale and 11 dB for the OCT/SLO scale. Contrast (Weber contrast) is defined as the ratio of the differential luminance (stimulus minus background luminance) to background luminance. To allow a direct comparison of sensitivity values between the MP-1 and the OCT/SLO, the stimulus attenuation scales were adjusted to an extended common scale that fit the contrast range used in both microperimeters.
In Table 2, MP-1 and OCT/SLO differential luminance is the stimulus luminance minus background luminance; MP-1 contrast and OCT/SLO contrast is the ratio of differential luminance to background luminance. The common scale is 0 to 29 dB with the MP-1 values ranging from 0 to 20 dB (same as original scale) and the OCT/SLO values ranging from 9 to 29 dB (shifted 9 dB). Thus, the 0 to 8 dB interval uniquely belongs to the MP-1 and the 21 to 29 dB intervals were uniquely used in the OCT/SLO. The two microperimeters share the 9 to 20 dB intervals (gray area in Table 2).
Table 2.
Original stimulus attenuation scales and common scale
Statistical Analysis
Macular light sensitivities from each eye were compared between two microperimeters for all the 28 matching points.
Normal distribution of the sensitivity threshold data was assessed with the Shapiro-Wilk test. Spearman correlations were used to analyze the relationship of sensitivity values obtained with the two microperimeters due to the abnormal distribution of data.
As each point was analyzed individually, a multilevel regression model was applied to establish a mathematical relationship in the sensitive values of the common intervals by groups and locations (three rings of Polar 3) while controlling the correlation among the points from the same eye and form the same subject (three different levels: points, eyes, subjects). Therefore, a random intercept of each point was contained in the regression model.
P values less than 0.05 were considered statistically significant. All analyses were performed using SPSS statistical package (SPSS, 19.0 Inc., Chicago, IL) and STATA (StataCorp LP, College Station, TX).
Results
Forty-five eyes from 24 healthy volunteers (12 females, 12 males) with a mean age of 35.4-years old (range: 21–83 years), and 47 eyes of 30 patients with maculopathy (16 females, 14 males) with a mean age of 58.9-years old (range: 32–80 years) were prospectively included in the study. Three eyes in the healthy group and 13 eyes in diseased group were excluded due to high refractive error (exceeding ±6.00 D sphere and ±1.00 D cylinder) or failed in the microperimetry test due to opacity of refractive media or poor VA.
The VA (mean ± SD) was 0.26 ± 0.25 logMAR. Maculopathies included diabetic maculopathy (24 eyes), AMD (15 eyes), central serous retinopathy (3 eyes), idiopathic macular hole (2 eyes), Stargardt's disease (1 eye), multifocal choroditis with cystoid macular edema (1 eye) and hydroxychloroquine maculopathy (1 eye).
A total of 1260 paired points (28 points per eye from 45 eyes) from the healthy group and 1316 paired points (28 points per eye from 47 eyes) from the maculopathy group were included in the analysis.
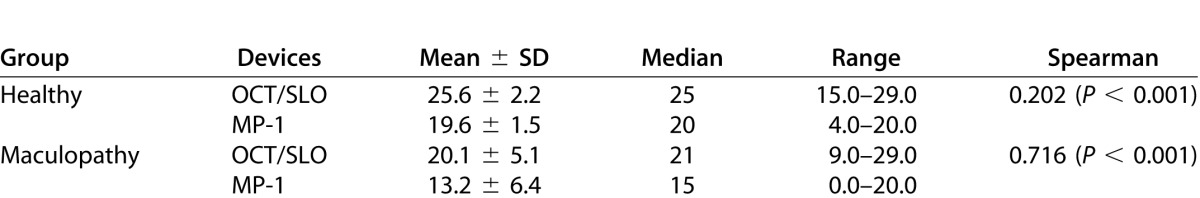
All retinal sensitivities described below are reported with values from the contrast-adjusted scale. The mean sensitivity measured with the OCT/SLO and MP-1 was 25.6 dB and 19.6 dB in heathy subjects and 20.1 dB and 13.2 dB in patients with maculopathies, respectively (Table 3). Both healthy and maculopathy subjects had a higher sensitivity when examined by the OCT/SLO device than the MP-1 device. The Spearman correlation between these two microperimeters was much higher in maculopathy group (r = 0.716) than in healthy group (r = 0.202).
Table 3.
Sensitivity thresholds measured with OCT/SLO and MP-1 in both groups (dB)
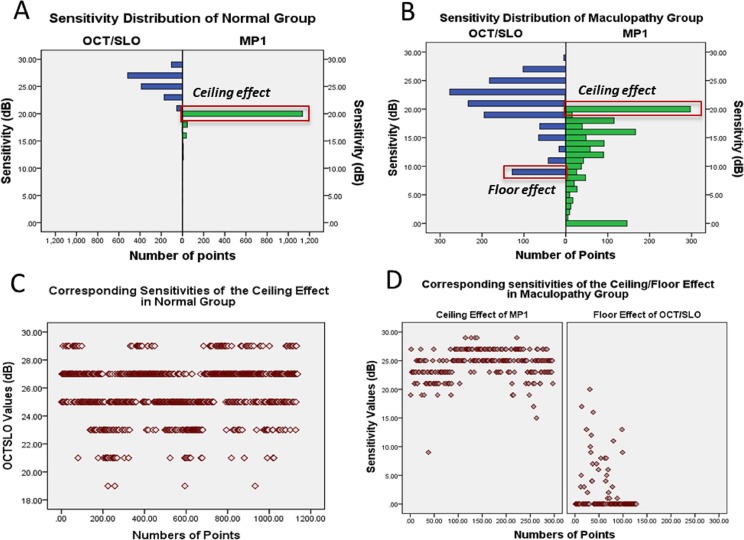
In the healthy group, 90.1% (1136/1260) of the sensitivity points acquired with the MP-1 were clustered at 20 dB (Fig. 2A, ceiling effect of the MP-1 highlighted in red box). The points clustered at 20 dB had a mean sensitivity of 25.8 ± 1.9 dB when measured with the OCT/SLO (Fig. 2C).
Figure 2.
Distribution pattern of sensitivities and ceiling/floor effect of microperimetry.
In the group of patients with maculopathy, 22.5% (296/1316) of points had sensitivity clustered at 20 dB when measured with the MP-1 (Fig. 2B, ceiling effect of the MP-1 highlighted in red box), the OCT/SLO corresponding mean sensitivity was 24.3 ± 2.5 dB (Fig. 2D). Conversely, 9.7% (128/1316) of the points were clustered at the lowest value of 9 dB in the OCT/SLO contrast-adjusted range (Fig. 2B, floor effect of the OCT/SLO highlighted in red box), the MP-1 corresponding mean sensitivity was 1.7 ± 3.9 dB (Fig. 2D). The majority of these points (76.6%, 98/128) had sensitivities as low as 0 dB of the MP-1.
A mathematical relationship was established by applying multilevel mixed-effects regression model for points in the 10 to 19 dB interval; the two edges of the common interval (9 and 20 dB) were removed due to the ceiling or floor effect. A total of 125 paired points from the healthy group and 864 paired sensitivity points from maculopathy group were included in the model.
The derived multilevel, mixed-effects model equations are as follows:
• Normal subjects:
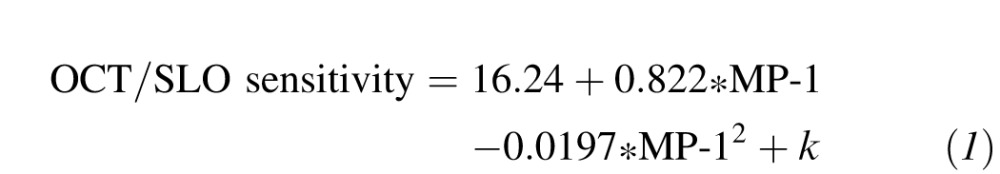 (1)
(1)
|
 |
• Subjects with maculopathy:
 |
 |
The constant k accounts for the random effects of each point. The values of the random effect vary from eye to eye and from subject to subject. Therefore, the magnitude of the effect cannot be given a specified value in the equations.
There were no statistically significant differences between the healthy and maculopathy group in the coefficient of MP-1 and MP-12, with P = 0.86 for MP-1 and P = 0.83 for MP-12.
In the conversion-equation for healthy subjects, the MP-1 coefficients have not reached statistical significance and the most probable explanation is the small number of points (only 1%) within the MP-1 - OCT/SLO common interval. As the slopes in two groups were not statistically significant, a general equation was derived by combining all points from both groups:
 |
 |
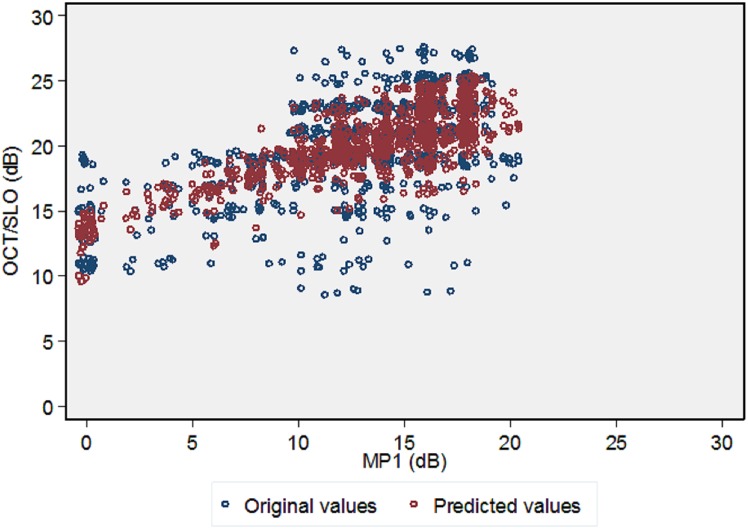
The original OCT/SLO values and the predicted OCT/SLO values from the equation are shown in Figure 3.
Figure 3.
The original and predicted OCT/SLO values by the regression equation.
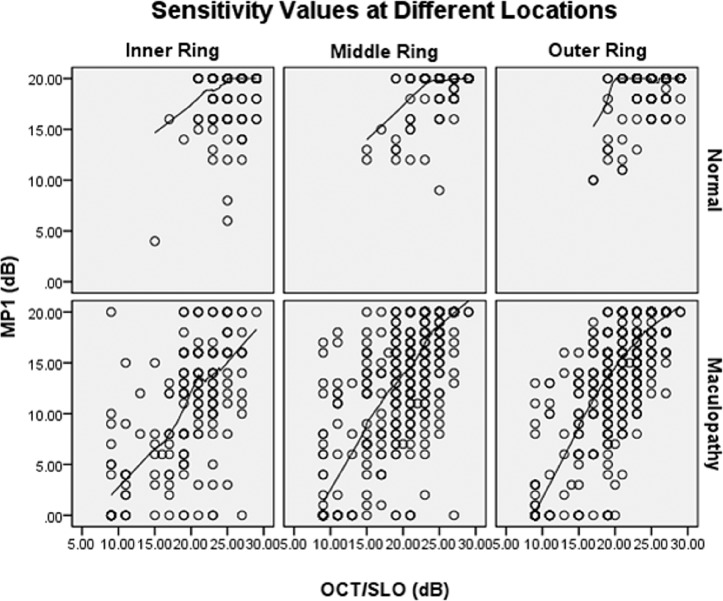
The mixed-effects model also considered the point's distribution into the three concentric rings of the pattern (inner, mid, and outer) but did not reveal differences in the relationship between the OCT/SLO and the MP-1 at this level (P = 0.1672). Figure 4 showed the similar lowess curves at different locations when sensitivity values from the OCT/SLO and the MP-1 was plotted against each other.
Figure 4.
The Relationship of OCT/SLO and MP1 at Different Locations
Discussion
The decibel is a logarithmic unit that indicates the ratio of a physical quantity (e.g., light intensity) relative to a specified or implied reference level. In perimetry, decibel value represents the attenuation ratio of stimulus intensity from maximum stimulus intensity. With different maximum stimulus intensity settings in perimeters, the same decibel value implies different stimulus intensity (sensitivity thresholds).
The stimuli attenuation scale disparity is the first factor to consider when accounting for the different sensitivity values across various (micro) perimeters. To make sure the certain decibel value equals the same stimulus intensity, the scale was converted in several comparison studies such as Rodenstock SLO101 scale + 5 dB = Octopus scale;30 MP-1 scale + 4 dB = Octopus scale31 and both MP-1 and OCT/SLO have the similar intervals of Humphrey Field Analyzer (HFA) scale (MP-1: 14–34 dB HFA equivalent, OCT/SLO: 13.1–33.6 dB of HFA equivalent).32 From a simple mathematical point of review, the sensitivity values of all (micro) perimeters were comparable, as the stimulus intensities have been calibrated into the same. But these conversions were only based on the stimulus intensity alone. By converting in this way, MP-1 and OCT/SLO have a nearly same scale32 as their maximum difference luminance are very close (127 vs. 125 cd/m2).
However, besides the stimulus intensity, the background luminance also plays an important role in the microperimetry examination. Detection of stimuli on a background is a luminance increment detection task, which depends upon the contrast of the target (stimulus) on the retina.22 Unifying the scale by the stimulus intensity may be sufficient for the comparison of the (micro) perimeters with the same background luminance such as MP-1 versus Octopus (both 1.27 cd/m2) or OCT/SLO versus HFA (both 10 cd/m2).
In (micro) perimeters that have different background luminances, subjects are tested under different contrast even with the same stimulus intensity. For example, in the Rohrschneider study, the conversion of Rodenstock SLO101 and Octopus scales were further adjusted by the contrast into SLO scale + 16 dB = Octopus scale22 as different to the previous conversion SLO scale + 5 dB = Octopus scale.30 As OCT/SLO has approximately an 10-fold brighter background than MP-1, we compared the values on the basis of contrast conversion as well. The conversion of OCT/SLO and MP-1 scales were further adjusted into OCT/SLO scale + 9 dB = MP-1 scale.
The mean OCT/SLO sensitivity values are higher than the MP-1 values in both groups (6 dB higher in the healthy group and 7 dB in maculopathy group). This was also observed in the Rohrscheider study22 that the sensitivity was higher under SLO than under Octopus and thought to be related with the difference of background luminance (light adaptation level). As indicated,22 increasing the light adaption level from the 1.27 cd/m2 (background luminance of SLO and OCT/SLO) to 10 cd/m2 (background luminance of Octopus and MP-1) decrease absolute sensitivity but increase relative light increment thresholds, and it is the latter that we measured.
The Spearman correlation between two devices was low (0.2) in the healthy group, which, to a great extent, is explained by the strong ceiling effect evidenced in the MP-1 outputs. It is in accordance with the previous study that the Spearman correlation between the MP-1 and the OCT/SLO is 0.25 when comparing them with the HFA.32 With less influence of the ceiling/floor effect, Spearman correlation increased to 0.7 in maculopathy group. The higher agreement in diseased group than in the healthy group was also observed by Vineet33 with the Pearson correlation between the MP-1 and the HFA was 0.4 in healthy subjects and 0.8 in glaucoma subjects.
The MP-1 ceiling effect was observed in previous studies in normal datasets.32,34 It is thought to be a limitation of the dynamic range of the MP-1 device. Once the dynamic range was extended by using the OCT/SLO range between 20 to 29 dB, we were able to further differentiate the retinal sensitivity of those points that were pooled in the upper bound of the MP-1 dynamic range. Similarly, the real sensitivity of those points showing a floor effect in the OCT/SLO was revealed by using MP-1 in the maculopathy group. The limited dynamic range makes the sensitivity of the MP-1 for detecting early-stage scotomas lower in comparison with the OCT/SLO. Conversely, the sensitivity of the OCT/SLO for observing changes in deep scotomas area (low retinal sensitivities) is also restricted by its dynamic range.
Ceiling and floor effect are limitations of several psychophysical measures such as VA charts and health-related questionnaire,35,36 but is unnecessary to be a drawback of microperimetry technology. By taking the conventional perimetry as a reference, the OCT/SLO scale corresponds to the 14 to 34 dB interval of the HFA and the MP-1 scale corresponds to the 5 to 25 dB interval of the 0 to 40 dB HFA (based on Weber contrast), there is still enough room to enlarge the dynamic range of both microperimeters.
The estimated regression equation was only applicable in the common intervals, which means if the MP-1 values were within 10 to 19 intervals, the OCT/SLO values can be predicted by the nonlinear equation. The equation was statistically significant and the prediction figure showed good consistence between the original values and predicted values. However, the prediction error of the equation within 1 dB is 36% and within 2 dB is 63%, which is not sufficient for clinical application.
Two main factors account for the low prediction accuracy, despite its being statistically significant. First, the vision regimes may be different. As there is no clear boundary from photopic to mesopic and scotopic luminance, there have been different mesopic luminance regions, such as luminance of 0.001 to 3 cd/m2,37 0.001 to 10 cd/m2,38 0.005 to 5 cd/m2,39 and 0.01 to 10 cd/m2.40 The background luminance of MP-1 evokes mesopic or near-photopic vision, while OCT/SLO mainly evokes photopic vision.32,41 It was also addressed by Seiple and colleagues32 that the low background luminance used in MP-1 falls well into the mesopic arrange. Measuring visual performance at the mesopic luminance range stimulates both rods and cones, is highly complex, and is very difficult to standardize or model.42 Any measurement of mesopic performance will depend not only on the illumination level, but also on the spectral content of the stimuli used to probe performance, their retinal location, their spatial frequency content, and their temporal frequency content.41 These different vision regimes may be a major obstacle to an accurate relationship of the sensitivities between these two microperimeters.
The other factor implies in the psychophysical nature of the microperimetry test. As a psychophysical examination, measurement variability is intrinsic and the variability in diseased subjects may be greater than that in healthy subjects, for example, the VA test in cataract patients or AMD patients,43,44 or the visual field test in glaucoma patients.45,46 It has been reported that the Coefficient of Repeatability (CoR) of the MP-1 is 5.56 dB in patients with maculopathy and 4.2 dB in patients with ABCA 4(ATP-binding cassette, sub-family A, member 4)-Associated Retinopathy when evaluated with the point sensitivity.26,47 A similar result of the OCT/SLO was also observed (Jang HK et al. ARVO 2013; Abstract ID: 3432 - C0153:3433), with the point sensitivity CoR as 4.64 dB in patients with maculopathy. In our study, due to the strong ceiling effect in healthy subjects; the data that used to generate the equation is mainly from maculopathy subjects. With 4- to 5-dB's measurement variability at the point sensitivity level of both MP-1 and OCT/SLO examinations, the rough sensitivity measurement itself also adds the difficulty of the computation into a pure mathematical equation.
The relationship of these two microperimeters was not influenced by different retinal locations. This is in agreement with previous studies in which four eccentric rings occupying 14° of central macular (modified 10-2 pattern) were tested between the HFA and two microperimters and no difference was found.32 The influence of locations could be reviewed when the testing pattern involves a larger macular area as an enlarged difference in the lower part of the visual field was noticed between MP-1 and Octopus in a rectangular test grid covering an area of 27° × 18° of central macula.31
Another important feature of the microperimetry technology is that it provides a comprehensive fixation assessment. The fixation test can be completed either as part of the routine sensitivity test or as an isolated test in both of the devices. Comparing fixation test results from both devices taken during routine sensitivity testing is not reliable due to variable test times, even when the same sensitivity pattern is used. For example, a subject who completes the Polar-3 sensitivity test in 3 minutes on MP-1 may complete the same pattern on OCT/SLO in 5 minutes. This is due to the differences of sensitivity test algorithms or settings.
An isolated fixation test (20 seconds) study has been conducted with both devices and preliminary analysis has indicated that there is high agreement in fixation stability measurements; the results will be reported in a separate manuscript.
In conclusion, OCT/SLO and MP-1 have the same nominal stimulus attenuation scale but provide two different ranges of contrasts for microperimetry examination. Both microperimeters have their limitations of the dynamic range. MP-1 has a ceiling effect at 20 dB but allows finer differentiation for damaged sensitivities. OCT/SLO has a floor effect at 0 dB but allows finer differentiation for near-normal sensitivities. There is a statistically significant relationship in the common interval of scale and such relationship is not influenced by locations. Broadening the stimulus luminance range for both microperimeters may minimize the constraint of the ceiling and floor effect allowing for better assessment of the light sensitivities.
Our study has demonstrated that sensitivity thresholds (expressed in decibel units) should be interpreted under the context of different stimulus attenuation scales and contrasts. Applying a unity background luminance and stimulus attenuation scale in all (micro) perimeters may make the clinical reference more consistent.
Acknowledgments
The authors thank Dr. William H. Seiple, Lighthouse International, for his valuable advice in appropriately interpreting the stimulus attenuation scale of (micro) perimeters and the psychophysics knowledge involved in this project.
Presented in part at the 2012 Association for Research of Vision and Ophthalmology Annual Meeting, May 6–10, 2012, Fort Lauderdale, Florida.
Financial Disclosure(s): The Johns Hopkins University has received research support from OPKO, Inc. and Optos, Inc. The sponsor had no role in the design or conduct of this research. The study was supported by the Hendrik Scholl Research Grant Award at the Wilmer Eye Institute (HL) and Research to Prevent Blindness (QDN). Dr. Nguyen serves on the Scientific Advisory Board for Optos, Inc. and Nidek, Inc.
Disclosure: H. Liu, None; M.G. Bittencourt, None; J. Wang, None; R. Sophie, None; M.A. Ibrahim, None; Y.J. Sepah, None; A. Moradi, None; H.P.N. Scholl, Fovea Pharmaceuticals, Trevena Inc., Guidepoint Global, LLC, Gerson Lehrman Group; and Q.D. Nguyen, Optos, Inc., Nidek, Inc.
References
- 1.Sabates NR, Crane WG, Sabates FN, Schuchard RA, Fletcher DC. Scanning laser ophthalmoscope macular perimetry in the evaluation of submacular surgery. Retina. 1996;16:296–304. doi: 10.1097/00006982-199616040-00004. [DOI] [PubMed] [Google Scholar]
- 2.Grenga P, Lupo S, Domanico D, Vingolo EM. Efficacy of intravitreal triamcinolone acetonide in long standing diabetic macular edema: a microperimetry and optical coherence tomography study. Retina. 2008;28:1270–1275. doi: 10.1097/IAE.0b013e31817d5d1c. [DOI] [PubMed] [Google Scholar]
- 3.Wong R, Khan J, Adewoyin T, Sivaprasad S, Arden GB, Chong V. The ChromaTest, a digital color contrast sensitivity analyzer, for diabetic maculopathy: a pilot study. BMC Ophthalmol. 2008;8:15. doi: 10.1186/1471-2415-8-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arend O, Remky A, Evans D, Stuber R, Harris A. Contrast sensitivity loss is coupled with capillary dropout in patients with diabetes. Invest Ophthalmol Vis Sci. 1997;38:1819–1824. [PubMed] [Google Scholar]
- 5.Young B, Eggenberger E, Kaufman D. Current electrophysiology in ophthalmology: a review. Curr Opin Ophthalmol. 2012;23:497–505. doi: 10.1097/ICU.0b013e328359045e. [DOI] [PubMed] [Google Scholar]
- 6.Reilly RB, Lee TC. Electrograms (ECG, EEG, EMG, EOG) Technol Health Care. 2010;18:443–458. doi: 10.3233/THC-2010-0604. [DOI] [PubMed] [Google Scholar]
- 7.Moiceanu C, Radocea R, Serghiescu I, Carstocea B. Electroretinography in monitoring glaucoma patients [in Romanian] Oftalmologia. 2010;54:13–17. [PubMed] [Google Scholar]
- 8.Van Mierlo C, Spileers W, Legius E, Casteels I, Cassiman C. Role of visual evoked potentials in the assessment and management of optic pathway gliomas in children. Doc Ophthalmol. 2013;127:177–190. doi: 10.1007/s10633-013-9399-5. [DOI] [PubMed] [Google Scholar]
- 9.Weingessel B, Sacu S, Vecsei-Marlovits PV, Weingessel A, Richter-Mueksch S, Schmidt-Erfurth U. Interexaminer and intraexaminer reliability of the microperimeter MP-1. Eye (Lond) 2009;23:1052–1058. doi: 10.1038/eye.2008.237. [DOI] [PubMed] [Google Scholar]
- 10.Okada K, Yamamoto S, Mizunoya S, Hoshino A, Arai M, Takatsuna Y. Correlation of retinal sensitivity measured with fundus-related microperimetry to visual acuity and retinal thickness in eyes with diabetic macular edema. Eye. 2006;20:805–809. doi: 10.1038/sj.eye.6702014. [DOI] [PubMed] [Google Scholar]
- 11.Vujosevic S, Midena E, Pilotto E, Radin PP, Chiesa L, Cavarzeran F. Diabetic macular edema: correlation between microperimetry and optical coherence tomography findings. Invest Ophthalmol Vis Sci. 2006;47:3044–3051. doi: 10.1167/iovs.05-1141. [DOI] [PubMed] [Google Scholar]
- 12.Hatef E, Colantuoni E, Wang J, et al. The relationship between macular sensitivity and retinal thickness in eyes with diabetic macular edema. Am J Ophthalmol. 2011;152:400–405. doi: 10.1016/j.ajo.2011.02.024. e402. [DOI] [PubMed] [Google Scholar]
- 13.Sepah YJ, Hatef E, Colantuoni E, et al. Macular sensitivity and fixation patterns in normal eyes and eyes with uveitis with and without macular edema. J Ophthalmic Inflamm Infect. 2012;2:65–73. doi: 10.1007/s12348-011-0052-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hartmann KI, Bartsch DU, Cheng L, et al. Scanning laser ophthalmoscope imaging stabilized microperimetry in dry age-related macular degeneration. Retina. 2011;31:1323–1331. doi: 10.1097/IAE.0b013e31820a6850. [DOI] [PubMed] [Google Scholar]
- 15.Landa G, Su E, Garcia PM, Seiple WH, Rosen RB. Inner segment-outer segment junctional layer integrity and corresponding retinal sensitivity in dry and wet forms of age-related macular degeneration. Retina. 2011;31:364–370. doi: 10.1097/IAE.0b013e3181e91132. [DOI] [PubMed] [Google Scholar]
- 16.Berisha F, Feke GT, Aliyeva S, Hirai K, Pfeiffer N, Hirose T. Evaluation of macular abnormalities in Stargardt's disease using optical coherence tomography and scanning laser ophthalmoscope microperimetry. Graefes Arch Clin Exp Ophthalmol. 2009;247:303–309. doi: 10.1007/s00417-008-0963-8. [DOI] [PubMed] [Google Scholar]
- 17.Szlyk JP, Paliga J, Seiple W, Rabb MF. Comprehensive functional vision assessment of patients with North Carolina macular dystrophy (MCDR1) Retina. 2005;25:489–497. doi: 10.1097/00006982-200506000-00015. [DOI] [PubMed] [Google Scholar]
- 18.Parravano M, Parisi V, Ziccardi L, et al. Single-session photodynamic therapy combined with intravitreal ranibizumab for neovascular age-related macular degeneration: a comprehensive functional retinal assessment. Doc Ophthalmol. 2013;127:217–225. doi: 10.1007/s10633-013-9404-z. [DOI] [PubMed] [Google Scholar]
- 19.Cho HJ, Kim CG, Yoo SJ, et al. Retinal functional changes measured by microperimetry in neovascular age-related macular degeneration treated with ranibizumab. Am J Ophthalmol. 2013;155:118–126. doi: 10.1016/j.ajo.2012.07.009. e111. [DOI] [PubMed] [Google Scholar]
- 20.Rohrschneider K, Bultmann S, Gluck R, Kruse FE, Fendrich T, Volcker HE. Scanning laser ophthalmoscope fundus perimetry before and after laser photocoagulation for clinically significant diabetic macular edema. Am J Ophthalmol. 2000;129:27–32. doi: 10.1016/s0002-9394(99)00270-6. [DOI] [PubMed] [Google Scholar]
- 21.Sun Z, Gan D, Jiang C, et al. Effect of preoperative retinal sensitivity and fixation on long-term prognosis for idiopathic macular holes. Graefes Arch Clin Exp Ophthalmol. 2012;250:1587–1596. doi: 10.1007/s00417-012-1997-5. [DOI] [PubMed] [Google Scholar]
- 22.Rohrschneider K, Fendrich T, Becker M, Krastel H, Kruse FE, Volcker HE. Static fundus perimetry using the scanning laser ophthalmoscope with an automated threshold strategy. Graefes Arch Clin Exp Ophthalmol. 1995;233:743–749. doi: 10.1007/BF00184084. [DOI] [PubMed] [Google Scholar]
- 23.Midena E, Vujosevic S, Cavarzeran F. Normal values for fundus perimetry with the microperimeter MP1. Ophthalmology. 2010;117:1571–1576. doi: 10.1016/j.ophtha.2009.12.044. 1576 e1571. [DOI] [PubMed] [Google Scholar]
- 24.Anastasakis A, McAnany JJ, Fishman GA, Seiple WH. Clinical value, normative retinal sensitivity values, and intrasession repeatability using a combined spectral domain optical coherence tomography/scanning laser ophthalmoscope microperimeter. Eye (Lond) 2011;25:245–251. doi: 10.1038/eye.2010.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Midena E, Radin PP, Pilotto E, Ghirlando A, Convento E, Varano M. Fixation pattern and macular sensitivity in eyes with subfoveal choroidal neovascularization secondary to age-related macular degeneration. A microperimetry study. Semin Ophthalmol. 2004;19:55–61. doi: 10.1080/08820530490882896. [DOI] [PubMed] [Google Scholar]
- 26.Chen FK, Patel PJ, Xing W, et al. Test-retest variability of microperimetry using the Nidek MP1 in patients with macular disease. Invest Ophthalmol Vis Sci. 2009;50:3464–3472. doi: 10.1167/iovs.08-2926. [DOI] [PubMed] [Google Scholar]
- 27.Landa G, Rosen RB, Garcia PM, Seiple WH. Combined three-dimensional spectral OCT/SLO topography and Microperimetry: steps toward achieving functional spectral OCT/SLO. Ophthalmic Res. 2010;43:92–98. doi: 10.1159/000247593. [DOI] [PubMed] [Google Scholar]
- 28.Sabates FN, Vincent RD, Koulen P, Sabates NR, Gallimore G. Normative data set identifying properties of the macula across age groups: integration of visual function and retinal structure with microperimetry and spectral-domain optical coherence tomography. Retina. 2011;31:1294–1302. doi: 10.1097/IAE.0b013e3182019be2. [DOI] [PubMed] [Google Scholar]
- 29.Rohrschneider K, Bultmann S, Springer C. Use of fundus perimetry (microperimetry) to quantify macular sensitivity. Progr Retinal Eye Res. 2008;27:536–548. doi: 10.1016/j.preteyeres.2008.07.003. [DOI] [PubMed] [Google Scholar]
- 30.Andersen MV. Scanning Laser Ophthalmoscope microperimetry compared with Octopus perimetry in normal subjects. Acta Ophthalmol Scand. 1996;74:135–139. doi: 10.1111/j.1600-0420.1996.tb00057.x. [DOI] [PubMed] [Google Scholar]
- 31.Springer C, Bultmann S, Volcker HE, Rohrschneider K. Fundus perimetry with the Micro Perimeter 1 in normal individuals: comparison with conventional threshold perimetry. Ophthalmology. 2005;112:848–854. doi: 10.1016/j.ophtha.2004.11.051. [DOI] [PubMed] [Google Scholar]
- 32.Seiple W, Rosen RB, Castro-Lima V, Garcia PM. The physics and psychophysics of microperimetry. Optom Vis Sci. 2012;89:1182–1191. doi: 10.1097/OPX.0b013e3182640c83. [DOI] [PubMed] [Google Scholar]
- 33.Ratra V, Ratra D, Gupta M, Vaitheeswaran K. Comparison between Humphrey Field Analyzer and Micro Perimeter 1 in normal and glaucoma subjects. Oman J Ophthalmol. 2012;5:97–102. doi: 10.4103/0974-620X.99372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Midena E, Radin PP, Convento E, Cavarzeran F. Macular automatic fundus perimetry threshold versus standard perimetry threshold. Eur J Ophthalmol. 2007;17:63–68. doi: 10.1177/112067210701700109. [DOI] [PubMed] [Google Scholar]
- 35.Beck RW, Maguire MG, Bressler NM, Glassman AR, Lindblad AS, Ferris FL. Visual acuity as an outcome measure in clinical trials of retinal diseases. Ophthalmology. 2007;114:1804–1809. doi: 10.1016/j.ophtha.2007.06.047. [DOI] [PubMed] [Google Scholar]
- 36.Massof RW. Application of stochastic measurement models to visual function rating scale questionnaires. Ophthalmic Epidemiol. 2005;12:103–124. doi: 10.1080/09286580590932789. [DOI] [PubMed] [Google Scholar]
- 37.Illuminating Engineering Society of North America. IESNA Lighting Handbook. 9th ed. New York: Illuminating Engineering;; 2000. [Google Scholar]
- 38.CIE TC 1-58 “Visual Performance in the Mesopic Range.”. Available at: http://www.lightinglab.fi/CIETC1-58/index.html. Accessed January 2014. [Google Scholar]
- 39.MOVE: Mesopic Optimization of Visual Efficiency. 2005 Available at: http://www.lightinglab.fi/research/international/MOVE/index.html. Accessed January 2014. [Google Scholar]
- 40.Halonen L, Puolakka M. CIE and Mesopic Photometry. CIE Tutorial and Expert Symposium on Measurement Uncertainties in Photometry and Radiometry for Industry; Vienna, Austria: 2014. September 11–12. [Google Scholar]
- 41.Stockman A, Sharpe LT. Into the twilight zone: the complexities of mesopic vision and luminous efficiency. Ophthalmic Physiol Opt. 2006;26:225–239. doi: 10.1111/j.1475-1313.2006.00325.x. [DOI] [PubMed] [Google Scholar]
- 42.Andrews DP, Hammond P. Mesopic increment threshold spectral sensitivity of single optic tract fibres in the cat: cone-rod interaction. J Physiol. 1970;209:65–81. doi: 10.1113/jphysiol.1970.sp009156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Patel PJ, Chen FK, Rubin GS, Tufail A. Intersession repeatability of visual acuity scores in age-related macular degeneration. Invest Ophthalmol Vis Sci. 2008;49:4347–4352. doi: 10.1167/iovs.08-1935. [DOI] [PubMed] [Google Scholar]
- 44.Elliott DB, Sheridan M. The use of accurate visual acuity measurements in clinical anti-cataract formulation trials. Ophthalmic Physiol Opt. 1988;8:397–401. doi: 10.1111/j.1475-1313.1988.tb01176.x. [DOI] [PubMed] [Google Scholar]
- 45.Holmin C, Krakau CE. Variability of glaucomatous visual field defects in computerized perimetry. Albrecht Von Graefes Arch Klin Exp Ophthalmol. 1979;210:235–250. [PubMed] [Google Scholar]
- 46.Heijl A, Lindgren A, Lindgren G. Test-retest variability in glaucomatous visual fields. Am J Ophthalmol. 1989;108:130–135. doi: 10.1016/0002-9394(89)90006-8. [DOI] [PubMed] [Google Scholar]
- 47.Cideciyan AV, Swider M, Aleman TS, et al. Macular function in macular degenerations: repeatability of microperimetry as a potential outcome measure for ABCA4-associated retinopathy trials. Invest Ophthalmol Vis Sci. 2012;53:841–852. doi: 10.1167/iovs.11-8415. [DOI] [PMC free article] [PubMed] [Google Scholar]