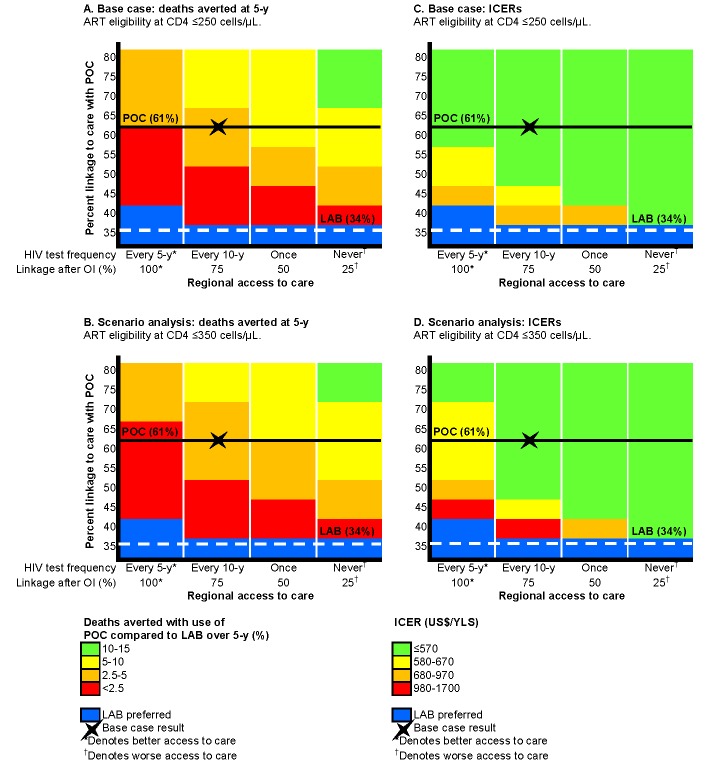
Figure 4. Multi-way sensitivity analysis on regional access to care and linkage to care with POC-CD4 compared to LAB-CD4.
Projected decrease in 5-y mortality and ICERs with use of POC-CD4 compared to LAB-CD4 in four settings that represent a range of access to care (decreasing access to care from left to right) and with different probabilities of linkage with POC-CD4 (increasing up the vertical axis). The base case is indicated by the X in each figure; the horizontal lines represent the base case overall linkage rates (POC-CD4, solid black; LAB-CD4, dashed white). Decreased mortality at 5 y with POC-CD4 is projected in settings that use current Mozambique guidelines for ART eligibility (CD4 count ≤250/µl) (A) or earlier ART eligibility (CD4 count ≤350/µl) (B). More deaths could be averted (noted by changes in color towards green) in settings with fewer opportunities to access care or by improving POC-CD4 linkage rates compared to LAB-CD4. Blue denotes the few situations in which LAB-CD4 results in better clinical outcomes than POC-CD4 at 5 y. (C) displays the ICERs of POC-CD4 compared with LAB-CD4 given current Mozambique guidelines (ART eligibility at CD4 count ≤250/µl); (D) displays ICERs in settings with earlier ART eligibility (CD4 count ≤350/µl). POC-CD4 is at the very cost-effective threshold (i.e., US$450–US$860/YLS in [C] and US$460–US$1,030/YLS in [D]) compared to LAB-CD4 except when linkage with POC-CD4 is <5% better than LAB-CD4 in settings with repeat HIV testing every 5 y.