Abstract
Entamoeba histolytica is a major cause of diarrhea in the developing countries and it can present with a wide range of gastrointestinal symptoms depending on the phase of the infection. We describe a case of 65-year-old male patient presented with abdominal pain and vomiting. On the clinical and radiological examination provisional diagnosis of colonic carcinoma was suspected. After resection of perforated caecal growth, histopathological sections showed numerous trophozoites of E. histolytica in a background of abundant necrosis. This case revealed differentiation between amoeboma and carcinoma is critical.
KEY WORDS: Amoeboma, colonic carcinoma, Entamoeba histolytica
INTRODUCTION
The term amebiasis is used clinically to denote all conditions which are produced in the human host by infection with Entamoeba histolytica. In general, the clinical spectrum of colorectal amebiasis ranges from asymptomatic carrier to severe fulminant necrotizing colitis with bleeding and perforation.[1] Amoeboma of the large bowel is a rare condition which is difficult to differentiate from colorectal carcinoma. It occurs in 1.5% of all cases with invasive amebiasis.[2] It is characterized by formation of tumor like masses of granulation tissue. Diagnosis rests upon the demonstration of trophozoites of E. histolytica in sections of tissues obtained by biopsy.
CASE REPORT
The present case report is about a 65-year-old diabetic male patient who presented to emergency department of our hospital with abdominal pain and vomiting. Pain was also associated with constipation and abdominal distension. He had past history of chronic abdominal pain, diarrhea and weight loss for last 2 months but no bleeding per rectum.
On general examination, patient was pale and cachectic. According to physical examination, patient's pulse was 102/min and blood pressure was 90/60 mmHg. Body temperature was recorded and it was 37°C. Abdominal examination revealed tenderness all over abdomen and mass in right ileac fossa. Local rectal examination was unremarkable.
Laboratory investigation showed anemia (hemoglobin = 8 g/dl) and high total leucocytes count (18,000/cumm). Report of liver function test was unremarkable, but there was serum electrolyte imbalance and blood sugar level was 240 mg/dl. Urgent chest radiograph and abdominal ultrasonography were suggested. Chest radiograph showed air under diaphragm. According to abdominal ultrasonography report, there was thickening of caecum and ascending colon and intraperitoneal air fluid collection.
Emergency laparotomy was planned with provisional diagnosis of perforative peritonitis in an obstructing right-sided colonic carcinoma. Intravenous antibiotic and injection human insulin were started. Two units blood transfusion was given pre-operatively. Laparotomy revealed a single perforation at caecum with inflamed surrounding area of the colon. There was a minimal peritoneal contamination. Resection of perforated caecal growth along with proximal ileostomy and distal mucous fistula was done under general anesthesia.
Resected intestine was 34 cm in length. A large ulcerative growth was identified in caecum measuring 10 cm in diameter. Rest of the wall was shaggy with one perforation proximal to the growth. Seven lymph nodes were identified. Trophozoites of E. histolytica were seen on histological examination [Figure 1]. Trophozoites were periodic acid-Schiff (PAS) positive [Figure 2]. On microscopic examination, abundant necrosis and transmural florid inflammatory changes were noted. Sections from seven lymph nodes showed reactive hyperplasia.
Figure 1.
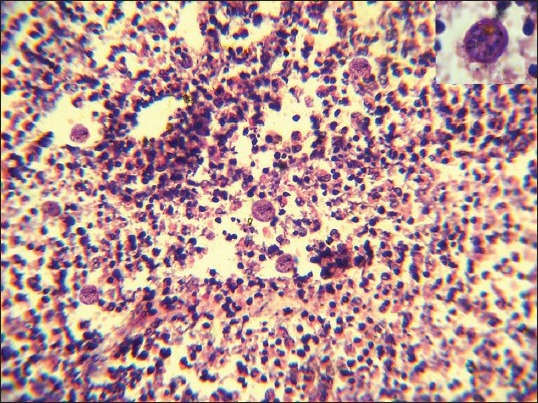
H and E stained histological section of amoeboma in the colonic wall demonstrating Entamoeba histolytica parasites in the inflammatory infiltrate (H and E, ×400). Inset showing degenerated E. histolytica containing ingested red blood cells (H and E, ×1000)
Figure 2.
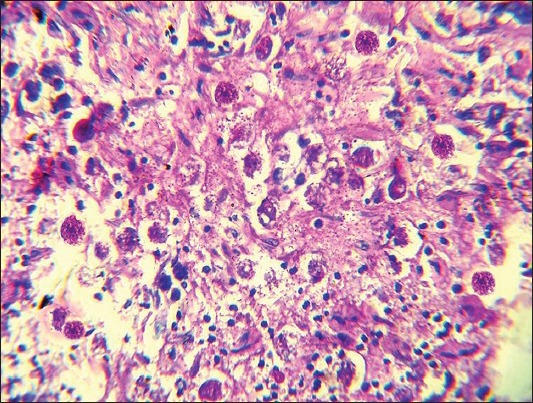
Periodic acid-Schiff (PAS) stain showing trophozoites of Entamoeba histolytica (×400, PAS)
CONCLUSIONS
E. histolytica is a major cause of dysentery in developing countries. An estimated 20% of world population harbor E. histolytica, but only a small number of patients develop invasive amoebiasis.[3] Infection occurs through ingestion of mature quadrinucleate cyst along with contaminated food and water. Most common site of localized infection is caecum and ascending colon followed by sigmoid-rectal region. Typical appearance of amoebic ulcer is flask shaped ulcer.
However lesions vary from small ulcer involving only mucosa to formation of tumor like mass (amoeboma). Gunn and Howard first described the term amoebic granulomas which was renamed as amoeboma by Ochsner and Debakey.[4,5] Amoeboma is characterized by localized florid inflammatory response with formation of pseudotumor by granulation tissue within the bowel wall. A study by Radke showed 26% patients with amoeboma presented with intermittent or complete bowel obstruction.[6] Differential diagnosis includes Crohn's disease and appendiceal abscesses in younger individuals and colon cancer and diverticulitis in the elderly.[7] Hence, in elderly individual amoeboma can be misdiagnosed as colonic carcinoma due to its rare incidence and unusual presentation. The studies by Ng et al.[8] Sinharay et al.[9] and Farnandes et al.[10] also found cases of amoebic colitis that caused diagnostic uncertainty by mimicking a colonic carcinoma.
Liver is the most common extra-colonic site where E. histolytica can produce lesions. Hepatic amoebiasis along with amoeboma can mimic metastatic liver nodule.
Microscopic examination of intestinal biopsy specimen is essential to differentiate between amoeboma and malignancy. In general, trophozoites are round or oval in shape having abundant vacuolated cytoplasm and perfectly round nuclei. On routine stain, trophozoites can be misdiagnosed as macrophages. Special stains are useful in this instance. On PAS staining trophozoites appear bright pink in color. Heidenhain's iron hematoxylin stain demonstrates erythrophagocytosis.
The management is a combination of both surgical resection and intravenous metronidazole.
This case attempts to highlight that amoebic colitis can mimic colonic carcinoma, particularly in an endemic area.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Ooi BS, Seow-Choen F. Endoscopic view of rectal amebiasis mimicking a carcinoma. Tech Coloproctol. 2003;7:51–3. doi: 10.1007/s101510300008. [DOI] [PubMed] [Google Scholar]
- 2.Misra SP, Misra V, Dwivedi M. Ileocecal masses in patients with amebic liver abscess: Etiology and management. World J Gastroenterol. 2006;12:1933–6. doi: 10.3748/wjg.v12.i12.1933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cardoso JM, Kimura K, Stoopen M, Cervantes LF, Flizondo L, Churchill R, et al. Radiology of invasive amebiasis of the colon. AJR Am J Roentgenol. 1977;128:935–41. doi: 10.2214/ajr.128.6.935. [DOI] [PubMed] [Google Scholar]
- 4.Gunn H, Howard NJ. Amoebic granulomas of the large bowel. JAMA. 1931;97:166–70. [Google Scholar]
- 5.Ochsner A, DeBakey M. Surgical amoebiasis. Int Clin. 1942;1:68–99. [Google Scholar]
- 6.Radke RA. Ameboma of the intestine: An analysis of the disease as presented in 78 collected and 41 previously unreported cases. Ann Intern Med. 1955;43:1048–66. doi: 10.7326/0003-4819-43-5-1048. [DOI] [PubMed] [Google Scholar]
- 7.Majeed SK, Ghazanfar A, Ashraf J. Caecal amoeboma simulating malignant neoplasia, ileocaecal tuberculosis and Crohn's disease. J Coll Physicians Surg Pak. 2003;13:116–7. [PubMed] [Google Scholar]
- 8.Ng DC, Kwok SY, Cheng Y, Chung CC, Li MK. Colonic amoebic abscess mimicking carcinoma of the colon. Hong Kong Med J. 2006;12:71–3. [PubMed] [Google Scholar]
- 9.Sinharay R, Atkin GK, Mohamid W, Reay-Jones N. Caecal amoebic colitis mimicking a colorectal cancer. J Surg Case Rep 2011. 2011:1. doi: 10.1093/jscr/2011.11.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fernandes H, D’Souza CR, Swethadri GK, Naik CN. Ameboma of the colon with amebic liver abscess mimicking metastatic colon cancer. Indian J Pathol Microbiol. 2009;52:228–30. doi: 10.4103/0377-4929.48927. [DOI] [PubMed] [Google Scholar]


