ABSTRACT
Few smokers receive evidence-based tobacco treatment during healthcare visits. Electronic health records (EHRs) present an opportunity to efficiently identify and refer smokers to state tobacco quitlines. The purpose of this case study is to develop and evaluate a secure, closed-loop EHR referral system linking patients visiting healthcare clinics with a state tobacco quitline. A regional health system, EHR vendor, tobacco cessation telephone quitline vendor, and university research center collaborated to modify a health system’s EHR to create an eReferral system. Modifications included the following: clinic workflow adjustments, EHR prompts, and return of treatment delivery information from the quitline to the patient’s EHR. A markedly higher percentage of adult tobacco users were referred to the quitline using eReferral than using the previous paper fax referral (14 vs. 0.3 %). The eReferral system increased the referral of tobacco users to quitline treatment. This case study suggests the feasibility and effectiveness of a secure, closed-loop EHR-based eReferral system.
Keywords: Electronic health record, Tobacco cessation, Telephonic tobacco quitline, Workflow, Healthcare system
INTRODUCTION
The healthcare setting presents an unequaled opportunity to treat patients who use tobacco. About 70 % of smokers visit a primary care clinician each year [1, 2], and the majority of them would like to quit [3]. In addition, multiple, effective, evidence-based tobacco dependence treatments could be provided in the healthcare setting. However, despite the intersection of a population in need, an appropriate venue, and effective evidence-based interventions [1], too few tobacco users leave their primary care visits with evidence-based treatment [4].
The healthcare regulatory-policy environment now supports an increasing role for electronic health records (EHRs) in the treatment of tobacco use. For instance, the 2009 Health Information Technology for Economic and Clinical Health (HITECH) Act calls for the provision of incentives to physicians and hospitals that adopt and demonstrate meaningful use of EHR systems [5, 6] including documentation of smoking status. Partly as a result of HITECH, 72 % of physicians [7] and 44 % of hospitals [8] in 2012 reported that they used electronic health records. In addition, the 2010 Affordable Care Act mandates coverage of evidence-based tobacco-use treatment [9, 10], which can be efficiently accomplished via the EHR [11].
The EHR has already demonstrated its potential to enhance the treatment of chronic diseases such as obesity, diabetes, and congestive heart failure [12]. Research also shows that EHR modifications can enhance adherence to guideline recommendations [13–16], improve quality of care [17, 18], and yield cost savings [5]. Additionally, research shows that EHR modifications can increase the medical staff’s assessment and treatment of tobacco use and may do so with little interruption of the workflow of busy clinicians [11, 19, 20]. Finally, the EHR may reduce the costs and burden of delivering tobacco dependence interventions by efficiently referring smokers to available external treatment resources such as state tobacco quitlines [21, 22].
Unfortunately, one limitation of many EHR systems is a limited capacity for closed-loop communication between the patient’s healthcare system and outside entities such as quitlines. Quitlines typically are independent, evidence-based tobacco cessation treatment services that provide counseling (and sometimes medication) to tobacco users [1] and are available in all 50 states (800-QUIT-NOW). With growing use of both EHRs and quitlines nationally, demand has increased to create a fully electronic tobacco quitline referral mechanism (“eReferral”) that can be incorporated into the EHR. In particular, there is interest in creating a mechanism that allows for both an eReferral from the clinic to the quitline and electronic feedback from the quitline to the patient’s EHR that closes the referral “loop” by summarizing the outcome of the referral in a manner that is compliant with the Health Insurance Portability and Accountability Act (HIPAA).
This paper describes a partnership among one of the nation’s largest EHR vendors (Epic Systems Corporation or “Epic”), a large Wisconsin healthcare system that uses the Epic EHR (Dean Health Systems or “Dean”), the nation’s largest telephone tobacco quitline vendor (Alere Wellbeing, Inc. or “Alere” that provides quitline services to the State of Wisconsin as the Wisconsin Tobacco Quit Line or “WTQL”), and a university-based tobacco dependence research center (the University of Wisconsin Center for Tobacco Research and Intervention or “UW-CTRI”). The goal of this work was to build and implement an EHR-based mechanism to electronically refer adult Dean patients who want to quit tobacco use to the WTQL for cessation services.
The EHR referral mechanism was intended to meet the following criteria: (a) fit seamlessly into existing clinic workflow supported by a reasonable level of staff training, (b) deliver daily HIPAA-compliant referrals from the health system clinics to the quitline vendor, and (c) electronically transmit service outcomes of the quitline referral in a timely and HIPAA-compliant way back to the individual patient’s EHR.
METHODS
Selection of clinics
Two Dean clinics in Madison, WI were selected that (1) had a paper Fax-to-Quit WTQL referral system in place for at least 1 year prior to the implementation of the new EHR-based eReferral system and (2) were using Epic EHR software. Of the two clinics selected, one was a primary care clinic (viz., a family medicine clinic with seven physicians) while the other was a specialty clinic (viz., pulmonary medicine with six physicians).
The paper fax (Fax-to-Quit) quitline referral system
A paper Fax-to-Quit program for the WTQL was developed in 2003 by the UW-CTRI as a mechanism to provide evidence-based care to clinic patients. This system was developed in response to health system requests to more efficiently link their patients to the WTQL. Once a healthcare system requested Fax-to-Quit, UW-CTRI Outreach staff traveled to the clinic or hospital to train staff on using the program and provide necessary materials (e.g., clinic-specific Fax-to-Quit referral forms). Utilizing Fax-to-Quit was relatively simple but required a number of manual steps. First, staff had to query patients regarding their tobacco-use status. Staff then described the WTQL services to the identified tobacco users and asked if the patients were interested in receiving such services. If the patient agreed and provided written permission, staff manually completed a paper Fax-to-Quit form that included contact information and best times for the WTQL to call the patient. The form was then manually faxed to the WTQL which attempted to contact the patient within 48 hours and deliver the WTQL treatment services. Depending on the clinic, different staff members assumed responsibility for these different tasks. Finally, the WTQL faxed back to the referring provider (not to the patient’s chart) a form describing the outcome of the referral, including whether their patient was reached, if she/he agreed to receive services, and which services were provided. Clinics were encouraged to enter quitline treatment information into the patient’s EHR (via scanning or manually), but few clinics reported doing so. Since 2003, approximately 1,000 healthcare sites in Wisconsin have implemented a Fax-to-Quit program, with 556 active at the time of this study. While many clinics have requested Fax-to-Quit, utilization has been very modest. During 2012, these sites referred a total of 1,884 patients to the WTQL, averaging 3.4 referrals per clinic per year (WTQL data).
The eReferral quitline referral system
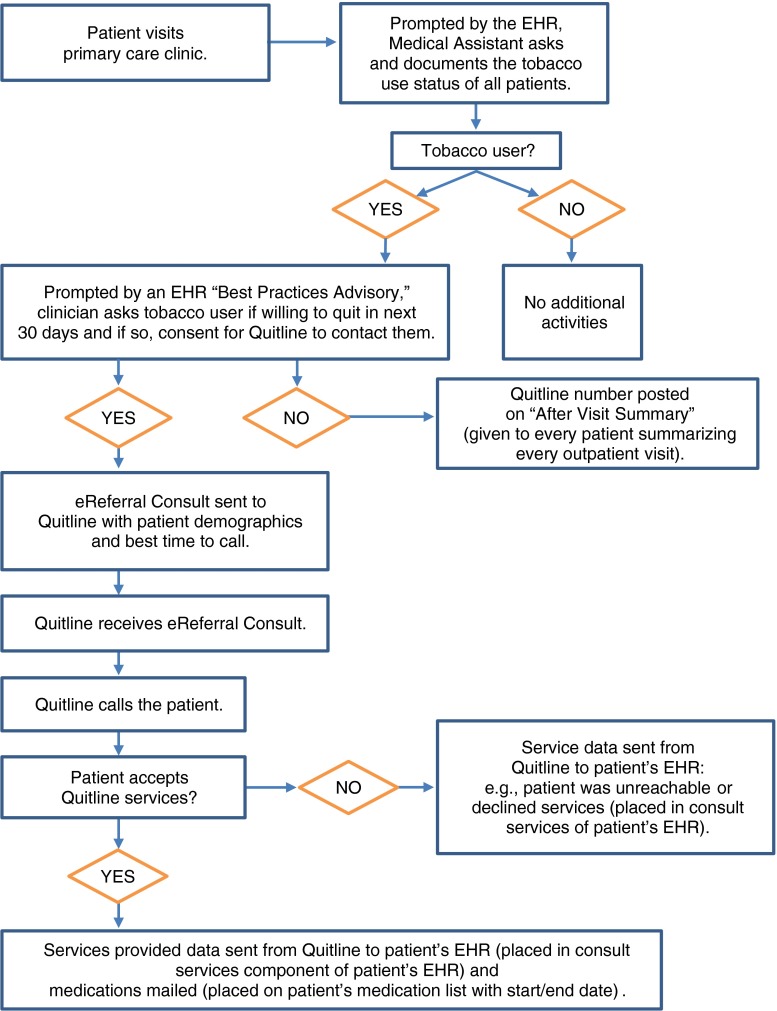
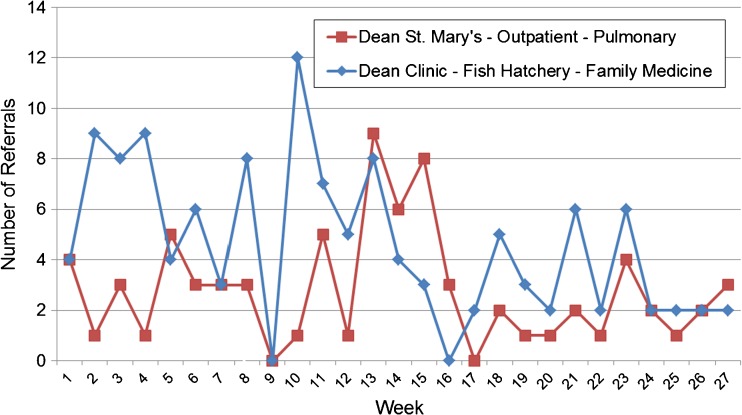
With the eReferral system, during a patient visit, the EHR prompts the clinic medical assistant (MA) or roomer to inquire about tobacco use as part of the standard EHR workflow (and as occurred with the paper fax system). The MA’s documentation of use activates a “Best Practice Advisory” (“BPA”—an Epic EHR tool to guide evidence-based clinical interventions) that electronically prompts the clinician to offer tobacco quitline services (see Figs. 1 and 2). The BPA gives the clinician the choice of selecting a WTQL “order” or documenting that the patient “declined” a referral to the WTQL. If the patient indicates an interest in the WTQL services, the clinician “accepts” the Best Practice Advisory which takes him/her to the eReferral order, which is automatically populated with the patient’s name and contact information, and presents options for the clinician to indicate optimal call times. Once completed, the eReferral is ready to be sent to Alere (Fig. 2). Each evening, the Dean EHR system electronically searches for the WTQL eReferrals, batches them, and electronically sends them to Alere. The exchange of patient information in both directions between Dean and the WTQL is via secure file transfer protocol (SFTP), which encrypts commands and data.
Fig 1.
eReferral to Wisconsin Tobacco Quit Line: clinic, patient, and data work flow
Fig 2.
Screenshots of the eReferral of tobacco users to the WTQL—roomer and clinician responsibilities
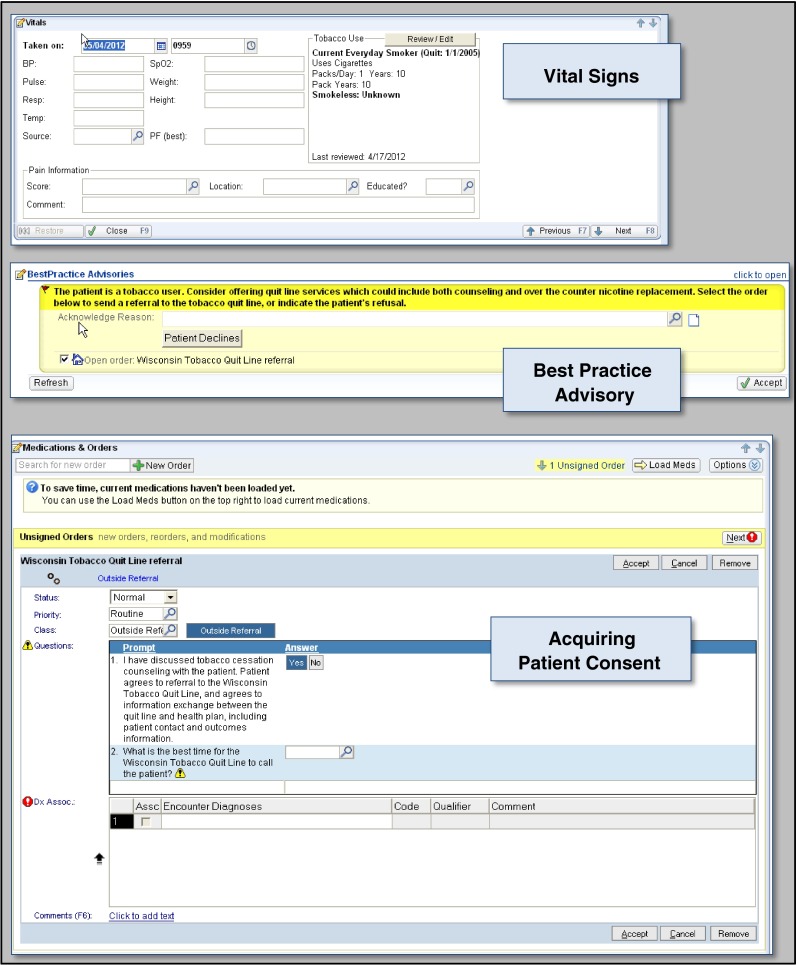
Once the WTQL receives an eReferral, they attempt to provide cessation services exactly as occurs with the paper fax referral. Once the WTQL completes treatment or exhausts the call attempts, they electronically send the eReferral treatment data back to the patient’s EHR, which automatically populates the patient’s EHR in two places—data on patient contact, counseling provided, and quit date are saved as a “referral outcome note” (Fig. 3), while provision of nicotine replacement medication (including the medication start and end dates based on the quit date) is documented in the medication list (Fig. 3).
Fig 3.
Screenshots depicting treatment services data from the WTQL that populates the patient’s EHR
Resource development, training, and data acquisition methods
Steps that we have previously taken to develop EHR modifications to facilitate smoking treatment and to support their implementation by healthcare settings are described in an earlier paper [11]. This earlier paper describes the planning process that led to the EHR modifications, methods to integrate the contributions of key stakeholders (health information technology staff, healthcare system representatives and clinicians, EHR vendor representatives, researchers), and the development of build guides and their quality improvement. Below, we describe the basic steps taken to develop the eReferral resource that is the topic of the current paper.
After initial meetings in September 2010 with the four stakeholders, Epic identified workable strategies for mapping and sharing data required to transmit eReferrals between Epic and the WTQL, and then devised tests to evaluate such functions. Next, Epic created a “build guide” for Dean IT staff to build and integrate the eReferral into their Epic EHR software; this required agreement regarding file names and format conventions. The eReferral mechanism from the health system to the Quit Line used an existing EHR functionality, i.e., “referral to a specialist.” The constructed referral mechanism generated unique patient, provider, and clinic identifiers to track the referral and treatment services provided data.
Standardized, defined, discrete data fields (Table 1) were used to facilitate extraction and sharing of data for meaningful use and quality measure achievement reporting. Key design characteristics built into the eReferral were that it be brief and convenient, with pick lists, check boxes, and scripted intervention language (clinical decision support) built into EHR screens.
Table 1.
eReferral data fields for closed-loop communication between EHR and WTQL
| The eReferral data fields used to transmit information from patient EHR to WTQL | Tobacco cessation service provision data fields used to transmit information from WTQL to patient EHR |
|---|---|
| Clinic name | Clinic identification number |
| Clinic identification number | Provider identification number |
| Provider name | eReferral identification number |
| Provider identification number | Patient identification number |
| Clinic address | Patient status: accepted services, declined services, unreachable |
| Clinic city | Disposition: general questions, materials only, one counseling call or multiple counseling calls |
| Clinic zip code | Nicotine replacement therapy and dose provided: patch, gum, or lozenge |
| Clinic county | Contact date (if contacted) |
| Clinic phone number | Planned quit date (if patient accepted services) |
| Clinic fax number | Quit status at registration (if accepted services) |
| Patient name | |
| eReferral identification number (unique number randomly generated for the eReferral by EHR) | |
| Patient identification number (unique patient number assigned by EHR) | |
| Gender | |
| Date of birth | |
| Pregnant (Y/N) | |
| Patient address | |
| Patient city | |
| Patient zip | |
| Patient county | |
| Patient primary phone number | |
| Patient secondary phone number | |
| Patient language preference | |
| Patient’s preferred time to receive call from WTQL |
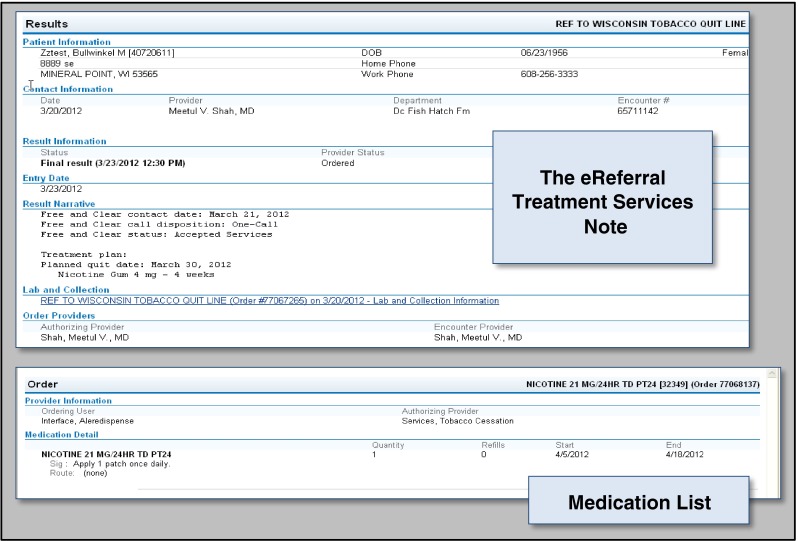
As with the paper fax referral system, staff at two pilot clinics were trained immediately prior to the pilot launch to use the new the WTQL eReferral capacity. Training included a description of the WTQL services and emphasized workflow, roles, and responsibilities (e.g., to refer only patients interested in the WTQL treatment). As with the paper fax referral, clinics using the eReferral system received monthly reports regarding their weekly WTQL eReferral activity (see Fig. 4). In addition, in a step that was not done with paper fax referral training, UW-CTRI staff contacted the manager of each pilot clinic weekly for the first month and monthly for the remaining 5 months of the pilot period to offer additional training, respond to questions, and alert Dean IT and Alere staff about any issues, malfunctions, or clinic-requested fixes or alterations. Neither of the two clinics requested additional training. Data were collected from May to November 2012 and analyzed in 2013.
Fig 4.
Number of weekly WTQL eReferrals by the two pilot clinics (May–November 2012)
For both the paper fax and eReferral systems, data acquisition to establish the WTQL referral rates occurred via weekly reports to the UW-CTRI from the WTQL. Referral rates were based on a denominator reflecting the number of adult smokers seen in the clinics during the targeted time periods; this was obtained for both referral systems by querying an existing EHR field for all Dean Clinic EHR systems that reflected response to an existing vital signs question regarding tobacco use.
RESULTS
The WTQL eReferral mechanism was implemented in May of 2012 (both clinics had been using the paper fax referral mechanism for approximately 3 years prior to the eReferral demonstration project). Data collection for electronic referrals then continued for 6 months (May to November 2012). In the 12 months preceding the launch of the eReferral mechanism, the two participating clinics made a total of eight paper-based fax referrals to the WTQL (Table 2). During the first 6 months after the implementation of the eReferral system, the two clinics electronically referred a total of 199 adult patients (Table 2). Based on an analysis of the number of adult tobacco users visiting these clinics, 0.3 % of tobacco users (8 of 2,692) were referred in the 12 months prior to the eReferral implementation, while 13.9 % of tobacco users (199 of 1,429) were referred during the first 6 months of eReferral. The two pilot clinics averaged a total of eight WTQL eReferrals each week during the eReferral pilot data collection period (Fig. 4).
Table 2.
Referral and acceptance rates of quitline treatment services comparing paper fax to electronic referral systems
| Number of tobacco users referred | Proportion of all adult tobacco users seen who were referred for WTQL services | Number of tobacco users accepting services | Proportion of all adult tobacco users seen who accepted WTQL services | |
|---|---|---|---|---|
| WTQL paper fax referral outcomes (over 12 months) | 8 | 0.3 % (8 smokers referred of 2,692 smokers seen) |
4 | 0.15 % (4 smokers accepted services of 2,692 seen) |
| WTQL eReferral outcomes (over 6 months) | 199 | 13.9 % (199 smokers referred of 1,429 smokers seen) |
70 | 4.9 % (70 smokers accepted services of 1,429 seen) |
Of the 199 adult tobacco users referred to the WTQL via eReferral, 70 accepted cessation services, representing 4.9 % of all tobacco users attending a clinic visit during the eReferral study period. In contrast, during the 12 months prior to the eReferral pilot phase, of the eight tobacco users referred to the WTQL via paper fax referral, four accepted quitline services, representing 0.15 % of all tobacco users seen in the clinics during that time period (Table 2).
DISCUSSION
Today, healthcare systems are simultaneously faced with a public health imperative, a refractory challenge, and an unprecedented opportunity. The public health imperative is the need to reduce tobacco use. The refractory challenge is the need to efficiently and cost-effectively engage smokers in evidence-based tobacco treatment [4, 23–25]. The unprecedented opportunity arises from the availability of the EHR, its rapid adoption by healthcare organizations, and the support of its use through important policy and practice initiatives (e.g., the 2009 HITECH Act [5] and the 2010 Affordable Care Act [9, 10]). One example of rapid EHR adoption is that provider e-prescribing via an EHR in the USA has increased from 7 % in 2008 to 54 % in 2012 [26]. The current case study provides tentative evidence that strategic EHR enhancements, placed within standard clinic workflow, can increase the number of smokers inducted into evidence-based smoking treatment, thereby addressing the imperative to more effectively treat tobacco use in healthcare settings. Specifically, this evidence suggests that EHR modifications permitting easy referral to a state tobacco quitline with closed-loop feedback increased the rate at which smokers were referred to and received treatment from the quitline.
Prior research supports the potential of the EHR to increase the rate at which patients are inducted into tobacco treatment [11, 19, 27]. The current case study, however, is the first to use the EHR to link clinicians directly with a smoking treatment resource outside their healthcare system while providing a closed-loop function that provides EHR feedback on the fate of the referral. These features are important because they increase the scope of EHR-guided patient care beyond an individual healthcare system, allowing for efficient delivery and integration of care both within and outside a healthcare system. Importantly, the external referral includes feedback to the clinician about the services provided as a result of the referral. Research suggests that such feedback is a potent influence on the clinician’s willingness to make referrals [28, 29].
This case study suggests that an efficient, EHR-integrated eReferral to the WTQL enhanced referral rates considerably over those obtained with a paper fax referral system. The quitline referral rate increased by a factor of about 46 (Table 2) when the eReferral system replaced the paper fax referral system. This increase may be inflated somewhat by at least two factors. First, the paper fax system was evaluated over a longer time period (12 months) than was the eReferral system (6 months). Even though the eReferral system was designed to impart little staff burden, perhaps, over time, staff use might nevertheless decline and erode referral rates. Second, there was somewhat greater post-implementation training support for the eReferral system than for the paper fax system. Finally, we were unable to assess the number of patients who refused a referral vs. those patients who were not asked about their interest in a referral.
Credence in the current results is supported by prior research that evaluated a similar set of EHR enhancements. Kruse and colleagues [27] developed and tested EHR modifications that provided clinicians in two community health centers with a 1-click link to refer smokers to their healthcare systems’ in-house tobacco care management system. The referral rate observed in Kruse study (15 %) was very similar to that seen in the current study (13.9 %). In addition, the referral rate observed with the paper fax system in the two research clinics seems representative of clinics in general. Together, these two clinics referred 8 patients for quitline treatment over 1 year; similarly, the WTQL data show that the average referral rate for the 556 clinics with active paper fax systems was 3.4 patients/clinic/year.
The EHR enhancements met the three feasibility goals established at the start of the pilot project: (a) The eReferral system appeared to mesh well with existing clinic workflow and responsibilities; (b) eReferrals were effectively transmitted daily from the clinic sites to the quitline vendor in a HIPAA-compliant way; and (c) quitline services provided as a result of the quitline referral were electronically transmitted in a HIPAA-compliant way back to the individual patient’s EHR. The success of the enhancements was no doubt fostered by collaboration of the major stakeholders (Epic, Alere, Dean, and UW-CTRI) at all phases of planning and implementation, repeated quality assurance evaluation, and modification of the planned EHR changes and workflow in response to quality assurance evaluations. In addition, there was a concerted effort to secure input from all relevant professional perspectives at all stages of development, i.e., from healthcare system leadership, front-line clinic staff, and information technology experts (from Epic, Alere, and Dean). However, while the results of this case study suggest that the tested EHR modifications were feasible and acceptable to clinic personnel, stronger support for this conclusion would require additional research that formally assesses the impact of such EHR modifications on indices of clinic performance and attitudes.
Quitline use is effective in boosting rates of smoking cessation, but it is underutilized, with only about 1 % of smokers in the USA using quitlines each year [30–33] and only 17 % of these reporting that a healthcare provider referred them to this cessation treatment [30]. Thus, our baseline referral rate to the WTQL of 0.3 % of smokers visiting the two clinics is consistent with national data. Moreover, the approximately 14 % WTQL referral rate after implementation of the eReferral system is substantial and would represent more than 4 million referrals if achieved among the approximately 30 million smokers who visit a primary care physician each year [1]. However, the extent to which such increases in referral rates reduce smoking prevalence depends upon patient follow-through once the referral is made and the effectiveness of the treatment program to which patients are referred.
One limitation of this project is that it involved only two clinics, one healthcare system, one quitline vendor, and one EHR vendor. Another is that the rates of eReferral were compared to rates for a paper fax referral system that had been in place for about 3 years; the lower rates of the latter may, in part, reflect decreased enthusiasm for the system over time. In addition, future research should adopt more formal experimental designs to investigate these EHR enhancements under conditions of greater experimental control. Further, these enhancements should be tested against control conditions that are matched with regard to training and support resources and include measurement of quit rates among patients referred to quitline cessation services. A further direction for future research might be to have the EHR engage in iterative tracking of patient’s treatment and smoking status in order to promote continued offer of treatment support as appropriate. Also, to the extent that these EHR enhancements are effective, it would be important to explore their cost-effectiveness and their long-term impact on smoking prevalence within healthcare systems.
Since this pilot project was completed, the UW-CTRI has continued working with its collaborators to create a more robust, modern, and efficient eReferral mechanism using healthcare reform/meaningful use compatible EHR functionality. The new EHR enhancements will include real-time, secure transmissions of data and constitute a standards-based solution (in content and communications methods) that could be implemented with other commercially available EHR platforms and quitline vendors.
In summary, this case study suggests the feasibility and effectiveness of a closed-loop EHR-based mechanism that electronically refers adult tobacco users visiting healthcare clinics to an external tobacco cessation quitline. Over a 6-month test period, approximately 14 % of smokers visiting two different clinics were electronically referred to the WTQL, and 33 % of those referred accepted quitline cessation services (almost 5 % of all smokers seen). This service acceptance rate is slightly lower than the fax-based referral system; it is possible that only the most treatment-motivated smokers are referred under a fax referral system (there is a high threshold for referral). It is possible that the acceptance rate of quitline cessation service would increase with additional EHR enhancements such as iterative cycles of follow-up tracking of smoking status and treatment engagement. Finally, other externally based clinical services could be similarly linked with a patient’s EHR, thus permitting EHR guidance and monitoring of an expanded range of clinical resources and services.
Acknowledgments
This project was supported by grant number 5P50CA143188 from the National Cancer Institute.
Footnotes
Implications
Practice: Electronic health records (EHRs) can be used to identify patients who use tobacco and to securely and electronically link these patients to external telephone-based tobacco cessation treatment, with services provided electronically transmitted back to the referred patient’s EHR.
Policy: EHRs are becoming ubiquitous in healthcare and provide a unique opportunity to efficiently refer patients to external prevention services, including tobacco cessation.
Research: EHR-based, closed-loop referral systems can be effectively tested and implemented in healthcare systems.
References
- 1.Fiore MC, Jaen CR, Baker TB, et al. Treating Tobacco Use and Dependence: 2008 Update. Rockville, MD: U.S. Department of Health and Human Services, U.S. Public Health Service; 2008. [Google Scholar]
- 2.Centers for Disease Control and Prevention Quitting smoking among adults—United States 2001–2010. MMWR. 2011;60(44):1513–1519. [PubMed] [Google Scholar]
- 3.Wewers ME, Stillman FA, Hartman AM, Shopland DR. Distribution of daily smokers by stage of change: current population survey results. Prev Med. 2003;36(6):710–720. doi: 10.1016/S0091-7435(03)00044-6. [DOI] [PubMed] [Google Scholar]
- 4.Jamal A, Dube SR, Malarcher AM, Shaw L, Engstrom MC. Tobacco use screening and counseling during physician office visits among adults—National Ambulatory Medical Care Survey and National Health Interview Survey, United States, 2005–2009. MMWR. 2012;61(Suppl):38–45. [PubMed] [Google Scholar]
- 5.Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med. 2010;363(6):501–504. doi: 10.1056/NEJMp1006114. [DOI] [PubMed] [Google Scholar]
- 6.Marcotte L, Seidman J, Trudel K, Berwick DM, Blumenthal D, Mostashari F, Jain SH. Achieving meaningful use of health Information technology: a guide for physicians to the EHR incentive programs. Arch Int Med. 2012;172(9):731–736. [DOI] [PubMed]
- 7.Hsiao CJ, Hing E. Use and Characteristics of Electronic Health Record Systems Among Office-Based Physician Practices: United States, 2001–2012. NCHS Data Brief No. 111. Hyattsville, MD: National Center for Health Statistics; 2012. [PubMed] [Google Scholar]
- 8.Charles D, King J, Patel V, Furukawa MF. Adoption of electronic health record systems among U.S. non-federal acute care hospitals: 2008–2012. ONC Data Brief, no 9. 2013. http://www.healthit.gov/sites/default/files/oncdatabrief9final.pdf. Access verified 12 Nov 2013.
- 9.U.S. Department of Health and Human Services. Patient Protection and Affordable Care Act. 2011. http://www.gpo.gov/fdsys/pkg/FR-2011-07-15/pdf/2011-17610.pdf. Access verified 12 Nov 2013.
- 10.Koh HK, Sebelius KG. Promoting prevention through the Affordable Care Act. N Engl J Med. 2010;363(14):1296–1299. doi: 10.1056/NEJMp1008560. [DOI] [PubMed] [Google Scholar]
- 11.Lindholm C, Adsit R, Bain P, et al. A demonstration project for using the electronic health record to identify and treat tobacco users. WMJ. 2010;109(6):335–340. [PMC free article] [PubMed] [Google Scholar]
- 12.Hivert MF, Grant RW, Shrader P, Meigs JB. Identifying primary care patients at risk for future diabetes and cardiovascular disease using electronic health records. BMC Health Serv Res. 2009;9:170. doi: 10.1186/1472-6963-9-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rattay KT, Ramakrishnan M, Atkinson A, Gilson M, Drayton V. Use of an electronic medical record system to support primary care recommendations to prevent, identify, and manage childhood obesity. Pediatrics. 2009;123(Suppl 2):S100–S107. doi: 10.1542/peds.2008-1755J. [DOI] [PubMed] [Google Scholar]
- 14.Bordowitz R, Morland K, Reich D. The use of an electronic medical record to improve documentation and treatment of obesity. Fam Med. 2007;39(4):274–279. [PubMed] [Google Scholar]
- 15.Goldberg HI, Neighbor WE, Cheadle AD, Ramsey SD, Diehr P, Gore E. A controlled time-series trial of clinical reminders: using computerized firm systems to make quality improvement research a routine part of mainstream practice. Health Serv Res. 2000;34(7):1519–1534. [PMC free article] [PubMed] [Google Scholar]
- 16.Fraser D, Baker TB, Fiore MC, Adsit RA, Christiansen BA. Electronic health records as a tool for recruitment of participants in clinical effectiveness research: lessons learned from tobacco cessation. Transl Behav Med. 2013;(3):244-52. [DOI] [PMC free article] [PubMed]
- 17.Bates DW, Ebell M, Gotlieb E, Zapp J, Mullins HC. A proposal for electronic medical records in U.S. primary care. J Am Med Inform Assoc. 2003;10(1):1–10. doi: 10.1197/jamia.M1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kemper AR, Uren RL, Clark SJ. Adoption of electronic health records in primary care pediatric practices. Pediatrics. 2006;118(1):e20–e24. doi: 10.1542/peds.2005-3000. [DOI] [PubMed] [Google Scholar]
- 19.Bentz CJ, Bayley BK, Bonin KE, et al. Provider feedback to improve 5A’s tobacco cessation in primary care: a cluster randomized clinical trial. Nicotine Tob Res. 2007;9(3):341–349. doi: 10.1080/14622200701188828. [DOI] [PubMed] [Google Scholar]
- 20.Linder JA, Ma J, Bates DW, Middleton B, Stafford RS. Electronic health record use and the quality of ambulatory care in the United States. Arch Intern Med. 2007;167(13):1400–1405. doi: 10.1001/archinte.167.13.1400. [DOI] [PubMed] [Google Scholar]
- 21.Greenwood DA, Parise CA, Macaller TA, et al. Utilizing clinical support staff and electronic health records to increase tobacco use documentation and referrals to a state quitline. J Vasc Nurs. 2012;30(4):107–111. doi: 10.1016/j.jvn.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 22.Boyle R, Solberg L, Fiore M. Use of electronic health records to support smoking cessation. Cochrane Database Syst Rev. 2011 (Issue 12:1-19. Art. No.: CD008743). [DOI] [PubMed]
- 23.Papadakis S, McDonald P, Mullen KA, Reid R, Skulsky K, Pipe A. Strategies to increase the delivery of smoking cessation treatments in primary care settings: a systematic review and meta-analysis. Prev Med. 2010;51(3–4):199–213. doi: 10.1016/j.ypmed.2010.06.007. [DOI] [PubMed] [Google Scholar]
- 24.Quinn VP, Stevens VJ, Hollis JF, et al. Tobacco-cessation services and patient satisfaction in nine nonprofit HMOs. Am J Prev Med. 2005;29(2):77–84. doi: 10.1016/j.amepre.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 25.Solberg LI, Asche SE, Boyle RG, Boucher JL, Pronk NP. Frequency of physician-directed assistance for smoking cessation in patients receiving cessation medications. Arch Intern Med. 2005;165(6):656–660. doi: 10.1001/archinte.165.6.656. [DOI] [PubMed] [Google Scholar]
- 26.Gabriel ME, Furukawa MF, Vaidya V. Emerging and encouraging trends in e-prescribing adoption among providers and pharmacies. Am J Manag Care. 2013;19(9):760-4. [PubMed]
- 27.Kruse GR, Kelley JH, Linder JA, Park ER, Rigotti NA. Implementation of an electronic health record-based care management system to improve tobacco treatment. J Gen Intern Med. Aug 4 2012;(12):1690-6. [DOI] [PMC free article] [PubMed]
- 28.Cantrell J, Shelley D. Implementing a fax referral program for quitline smoking cessation services in urban health centers: a qualitative study. BMC Fam Pract. 2009;10:81. doi: 10.1186/1471-2296-10-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Holtrop JS, Malouin R, Weismantel D, Wadland WC. Clinician perceptions of factors influencing referrals to a smoking cessation program. BMC Fam Pract. 2008;9:18. doi: 10.1186/1471-2296-9-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.North American Quitline Consortium. 2011. Results from the 2010 NAQC Annual Survey of Quitlines. http://www.naquitline.org/?page=survey2010. Access verified 12 Nov 2013.
- 31.Cummins SE, Bailey L, Campbell S, Koon-Kirby C, Zhu SH. Tobacco cessation quitlines in North America: a descriptive study. Tob Control. 2007;16(Suppl 1):i9–i15. doi: 10.1136/tc.2007.020370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ossip-Klein DJ, McIntosh S. Quitlines in North America: evidence base and applications. Am J Med Sci. 2003;326(4):201–205. doi: 10.1097/00000441-200310000-00010. [DOI] [PubMed] [Google Scholar]
- 33.North American Quitline Consortium. 2009. Increasing reach of tobacco cessation quitlines: a review of the literature and promising practices. (C. Bronar, MA, J.Saul, PhD). Phoenix, AZ. http://c.ymcdn.com/sites/www.naquitline.org/resource/resmgr/issue_papers/naqc_issuepaper_increasingre.pdf