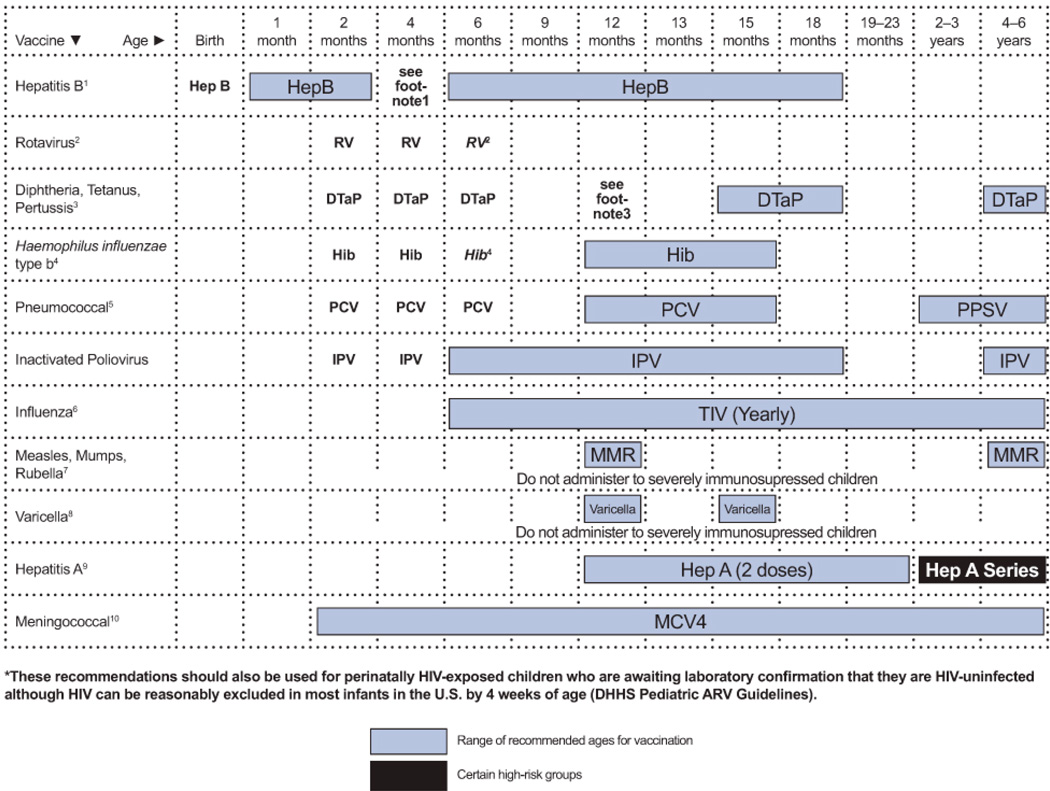
Figure 1. Recommended Immunization Schedule for HIV-Infected Children Aged 0–6 Years; United States, 2013 (Last updated November 6, 2013; last reviewed November 6, 2013).
This schedule summarizes recommendations for routine administration of vaccines for HIV-infected children 0–6 years and indicates the recommended ages for vaccine administration in this population for childhood vaccines licensed in the United States. Any dose not administered at the recommended age should be administered at a subsequent visit, when indicated and feasible. Licensed combination vaccines may be used whenever any component of the combination is indicated and other components of the vaccine are not contraindicated and if approved by the Food and Drug Administration for that dose of the series. Providers should consult the relevant Advisory Committee on Immunization Practices statement for detailed recommendations. Clinically significant adverse events that follow immunization should be reported to the Vaccine Adverse Event Reporting System (VAERS). Guidance about how to obtain and complete a VAERS form is available at http://www.vaers.hhs.gov or telephone 800-822-7967.
Hepatitis B vaccine (HepB)
Minimum age: Birth
- Administer monovalent HepB to all newborns before hospital discharge.
- If mother is hepatitis B surface antigen (HBsAg)-positive, administer HepB and 0.5 mL of hepatitis B immune globulin (HBIG) within 12 hours after birth.
- If mother’s HBsAg status is unknown, administer HepB within 12 hours after birth. Determine mother’s HBsAg status as soon as possible and if HBsAg-positive, administer HBIG as soon as possible
- The HepB series should be completed with either monovalent HepB or a combination vaccine containing HepB. The second dose should be administered at ages 1 through 2 months. Monovalent HepB should be used for doses administered before 6 weeks. The final dose should be administered no earlier than age 24 weeks. Infants who did not receive a birth dose should receive 3 doses of a HepB-containing vaccine on an age-appropriate schedule
- It is permissible to administer 4 doses of HepB when combination vaccines are administered after the birth dose. If monovalent HepB is used for doses after the birth dose, a dose at age 4 months is not needed.
- Infants born to HBsAg-positive mothers should be tested for HBsAg and the antibody to HBsAg (anti-HBs) after completion of at least 3 doses of a licensed HepB series, at ages 9 through 18 months(generally at the next well-child visit).
- Testing is recommended for HIV-infected children and should be performed 1 to 2 months after administration of the last dose of the vaccine series using a method that allows determination of a protective level of anti-HBs (≥10 mIU/mL).
- Children with anti-HBs < 10 mIU/mL after the primary schedule should receive a second series, followed by anti-HBs testing 1 to 2 months after the third dose, which usually is more practical than serologic testing after one or more doses of vaccine.
- In HIV-infected children, the need for booster doses has not been determined. Annual anti-HBs testing and booster doses when anti-HBs levels decline to < 10 mIU/mL should be considered in individuals with ongoing risk for exposure. See MMWR 2005:54(No. RR-16).
Rotavirus vaccine (RV)
-
Practitioners should consider the potential risks and benefits of administering rotavirus vaccine to infants with known or suspected altered immunocompetence. Consultation with an immunologist or infectious disease specialist is advised. Limited safety and efficacy data are available for the administration of rotavirus vaccines to infants who are potentially immunocompromised, including those who are HIV-infected. However, the following considerations support vaccination of HIV-exposed or HIV-infected infants:
- In infants born to HIV-positive mothers, the HIV diagnosis may not be established before the age of the first rotavirus vaccine dose (only 1.5%–3% of HIV-exposed infants in the United States will eventually be determined to be HIV-infected), and
- Vaccine strains of rotavirus are considerably attenuated.
- The maximum age for the first dose in the series is 14 weeks and 6 days; for the final dose in the series, it is 8 months and 0 days. Vaccination should not be initiated for infants aged 15 weeks and 0 days or older.
- If Rotarix® is administered at ages 2 and 4 months, a dose at 6 months is not indicated.
Diphtheria and Tetanus Toxoids and Acellular Pertussis Vaccine (Dtap)
- The fourth dose may be administered as early as age 12 months, provided that at least 6 months have elapsed since the third dose.
Haemophilus Influenzae Type B Conjugate Vaccine (Hib)
- If PRP-OMP (PedvaxHIB® or ComVax® [Hep B-Hib]) is administered at ages 2 and 4 months, a dose at age 6 months is not indicated.
- Hiberix should not be used for doses at ages 2, 4, or 6 months for the primary series but may be used as the final dose in children aged 12 months through 4 years.
- One dose of Hib vaccine should be administered to unvaccinated or partially vaccinated persons aged 5 years or older who have leukemia, malignant neoplasms, anatomic or functional asplenia (including sickle cell disease), HIV infection, or other immunocompromising conditions.
Pneumococcal Vaccine
- A PCV series begun with 7-valent PCV (PCV7) should be completed with 13-valent PCV (PCV13). A single supplemental dose of PCV13 is recommended for children aged 14 months through 71 months who have received an age-appropriate series of PCV7. For incompletely vaccinated children aged 24 months through 71 months, administer 2 doses of PCV13 at least 8 weeks apart. Children who have previously received 3 PCV doses need only 1 dose.
- Children aged 2 years or older also should receive PPSV after their last PCV dose.
Trivalent Inactivated Influenza Vaccine (TIV)
- Administer annually to HIV-infected children aged 6 months through 6 years and to all their eligible close contacts (including household members). TIV is recommended for HIV-infected children.
- For healthy, non-pregnant close contacts aged 2 years through 49 years, either live, attenuated influenza vaccine (LAIV) or TIV may be used.
- Children receiving TIV should receive 0.25 mL if aged 6 through 35 months or 0.5 mL if aged 3 years or older.
- Administer 2 doses (separated by at least 4 weeks) to children aged younger than 9 years per current influenza vaccine recommendations.
Inactivated Polio Vaccine (IPV)
- If 4 or more doses are administered prior to age 4 years, an additional dose should be administered at ages 4 through 6 years.
- The final dose in the series should be administered on or after the fourth birthday and at least 6 months after the previous dose.
Measles, Mumps, and Rubella Vaccine (MMR)
- Two doses of MMR vaccine for all HIV-infected individuals aged ≥12 months who do not have evidence of current severe immunosuppression (i.e., individuals aged ≤5 years must have CD4 T lymphocyte [CD4] percentages ≥15% for ≥6 months; and individuals aged >5 years must have CD4 percentages ≥15% and CD4 ≥200 lymphocytes/mm3 for ≥6 months) or other current evidence of measles, rubella, and mumps immunity. In cases when only CD4 cell counts or only CD4 percentages are available for those older than age 5 years, the assessment of severe immunosuppression can be based on the CD4 values (count or percentage) that are available. In cases when CD4 percentages are not available for those aged ≤5 years, the assessment of severe immunosuppression can be based on age-specific CD4 counts at the time CD4 counts were measured; i.e., absence of severe immunosuppression is defined as ≥6 months above age-specific CD4 count criteria: CD4 count >750 lymphocytes/mm3 while aged ≤12 months and CD4 count ≥500 lymphocytes/mm3 while aged 1 through 5 years.
- The first dose should be administered at ages 12 months through 15 months and the second dose at ages 4 years through 6 years, or as early as 28 days after the first dose.
- Individuals with perinatal HIV infection who were vaccinated prior to establishment of effective combination antiretroviral therapy (cART) should receive 2 appropriately spaced doses of MMR vaccine once effective cART has been established (for individuals aged ≤5 years: must have CD4 percentages ≥15% for ≥6 months; and for individuals aged >5 years: must have CD4 percentages ≥15% and CD4 ≥200 lymphocytes/mm3 for ≥6 months) unless they have other acceptable current evidence of measles, rubella, and mumps immunity.
Varicella Vaccine
- Limited data are available on safety and immunogenicity of varicella vaccine in HIV-infected children aged 1 year through 8 years in CDC immunologic categories 1 and 2 (CD4 T-lymphocyte percentages 15% or greater) and clinical categories N, A, and B.
- Single-antigen varicella vaccine should be considered for HIV-infected children who have CD4 percentages ≥15%. Eligible children should receive 2 doses 3 months apart, with the first dose administered as soon as possible after the first birthday.
- Varicella vaccine is not recommended for HIV-infected children who have evidence of severe immunosuppression (CD4 percentage <15% at any age; for those older than age 5 years, CD4 count <200 cells/mm3).
- MMRV vaccine has not been studied in HIV-infected children and should not be substituted for singleantigen varicella vaccine.
Hepatitis A Vaccine (HepA)
- Administer to all children aged 12 months through 23 months. The 2 doses in the series should be administered at least 6 months apart.
- Children who are not fully vaccinated by age 2 years can be vaccinated at subsequent visits.
- HepA is also recommended for children 24 months and older who live in areas where vaccination programs target older children, who are at increased risk of infection, or for whom immunity against hepatitis A is desired. See MMWR 2006;55(No. RR-7).
Meningococcal Vaccine
- Administer MCV4 to children aged 2 years through 6 years who have functional asplenia and certain other high-risk groups. A primary series of 2 doses should be administered with a minimum interval of 8 weeks. See MMWR 2007;56(48):1265–6.
- Administer MCV4-D (Menactra) to infants/children 9 months through 23 months who have persistent complement component deficiency, are traveling to an area endemic for meningococcal disease, or are involved in a meningococcal outbreak.
- Children who received MPSV4 ≥3 years previously and remain at increased risk of meningococcal disease should be revaccinated with MCV4.
- HIV-infected children are not considered at increased risk of meningococcal disease because of HIV infection, per se. Although the efficacy of MCV4 among HIV-infected children is unknown, providers can vaccinate HIV-infected children.
- HIV-infected children who remain at increased risk of meningococcal disease should be vaccinated every 5 years thereafter.