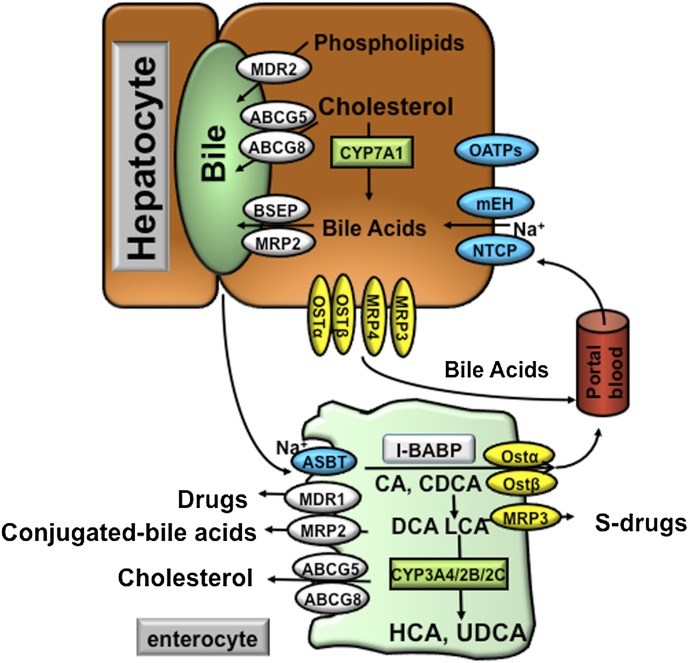
Fig. 4.
Bile acid transporters in the hepatocytes and enterocytes. At the basolateral membrane of the hepatocytes, the NTCP and mEH may be responsible for Na+-dependent uptake of conjugated bile acids, whereas OATPs show substrate specificity for unconjugated bile acids. At the canalicular membrane of the hepatocytes, the BSEP plays a major role in biliary secretion of bile acids, whereas the MRP2 mediates secretion of organic substrates including bile acids, bilirubin, and glutathione. ABCG5 and ABCG8 heterodimers transport cholesterol into the bile, whereas MDR2 is responsible for biliary secretion of phospholipids. At the basolateral membrane of the hepatocytes, organic solute transporters OSTα and OSTβ heterodimers, MRP3, and MRP4 mediate secretion of bile acids into the circulation. With cholestasis, both basolateral bile acid efflux and renal bile acid excretion are increased. After bile acids are released from the gallbladder into the intestine, ileal bile acid uptake is mediated by the ASBT. Intracellular bile acids are bound to the intestinal bile acid binding protein (IBABP). At the basolateral membrane, bile acid efflux is mediated by the OSTα and OSTβ heterodimers. At the apical membrane of the enterocytes, ABCG5 and ABCG8 heterodimers transport cholesterol back into the intestinal lumen, a process that limits intestine cholesterol absorption. CYP3A4, CYP2B, and CYP2C are involved in the metabolism and detoxification of LCA in the intestine. In the apical membrane of intestine, MDR1 effluxes drugs and MRP2 effluxes conjugated bile acids. In the sinusoidal membrane, MRP3 effluxes sulfur-conjugated drugs for renal excretion.