Introduction
Accurate estimates of the specific absorption rate (SAR) of RF power deposition during MRI are vital to patient safety. However, the accuracy of scanner SAR estimates is questionable in light of thermally-derived SAR measurements (1,2). Independent measurements are essential for the assessment of RF burn injuries resulting from MRI (2,3), and for accurately documenting SAR exposure during the testing of medical implants and leads, whose presence typically exacerbates local heating (4). Unfortunately, the dynamic range (DR) of MRI RF transmit pulses is high, and available commercial devices have limited DR, buffer size and channels available for monitoring the power flow through the scanner at multiple locations.
We have developed a high-DR, MRI-compatible, battery-operated 6-channel, power profiling system for monitoring and recording RF power in real time. The system is broadband capable to operate up to 400 MHz. We used it to monitor the RF power delivered to 11 volunteers during whole-body 3T MRI in real-time. We found that true measured SAR varied considerably from the scanner’s estimates.
Methods
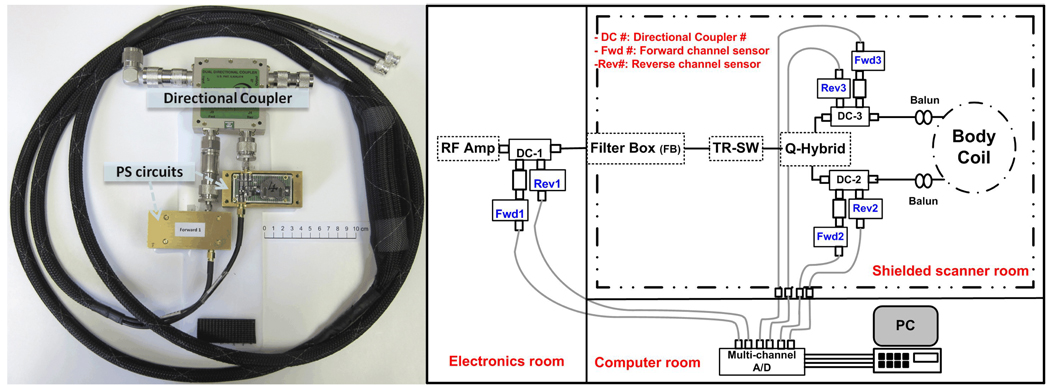
Six power sensor (PS) circuits were assembled from logarithmic amplifier IC’s (AD8310) and attached to the forward and reverse channels of three (50 dB) directional couplers (Werlatone Inc.). A 10 dB attenuator was attached to the three forward channels to enable measurements of up to 50 kW of peak power. The output of each of the six PS circuits are sampled at 200 kHz by a USB National instruments data acquisition system (USB-6251) controlled by a laptop computer that also stores the power measurement data. Figure 1 shows a picture of one of the three power profiling assemblies and a schematic of the system configured to monitor RF power.
Figure 1.
Picture (left) of one of the three power profiling modules showing the directional coupler and PS circuits. Right is a schematic for the power measurement setup.
Results
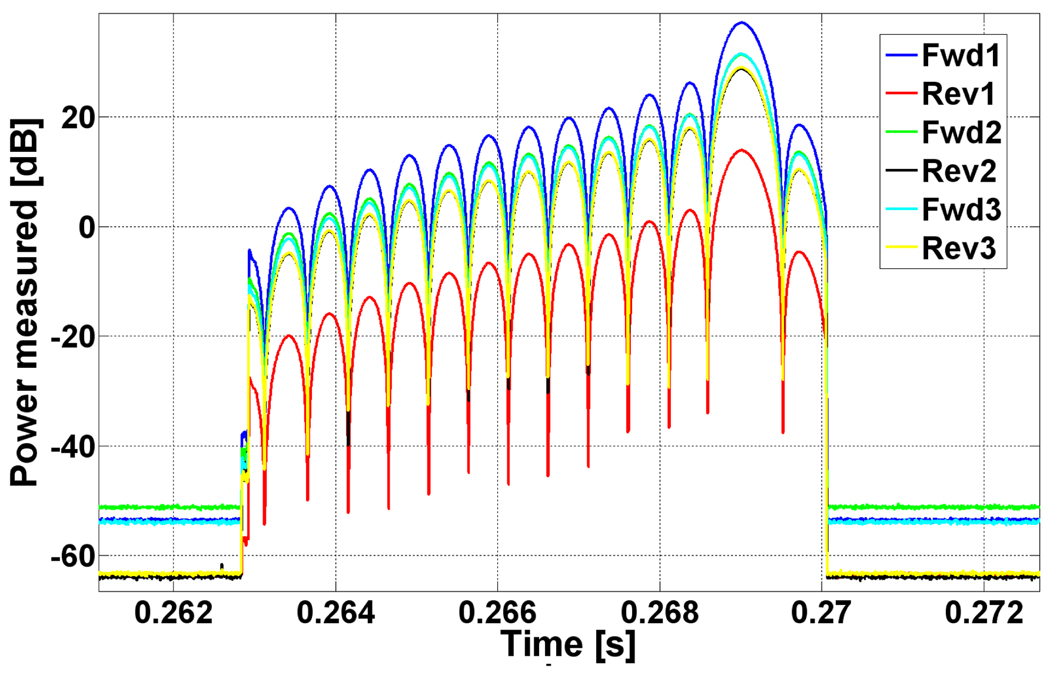
Each PS circuit was calibrated using a continuous wave RF source against an independent power meter (Ladybug Technologies LLC, LB480A). Tests show that the PS circuit deviates less than ~0.8 dB from linear performance over a 90dB DR. MRI experiments showed no interference or image degradation with the monitors connected. Figure 2 exemplifies 6-channel recordings of an asymmetric, multi-lobe, slice selective RF pulse.
Figure 2.
Example of the 6-channel real-time power profile of a ~7ms RF, asymmetric, selective RF pulse.
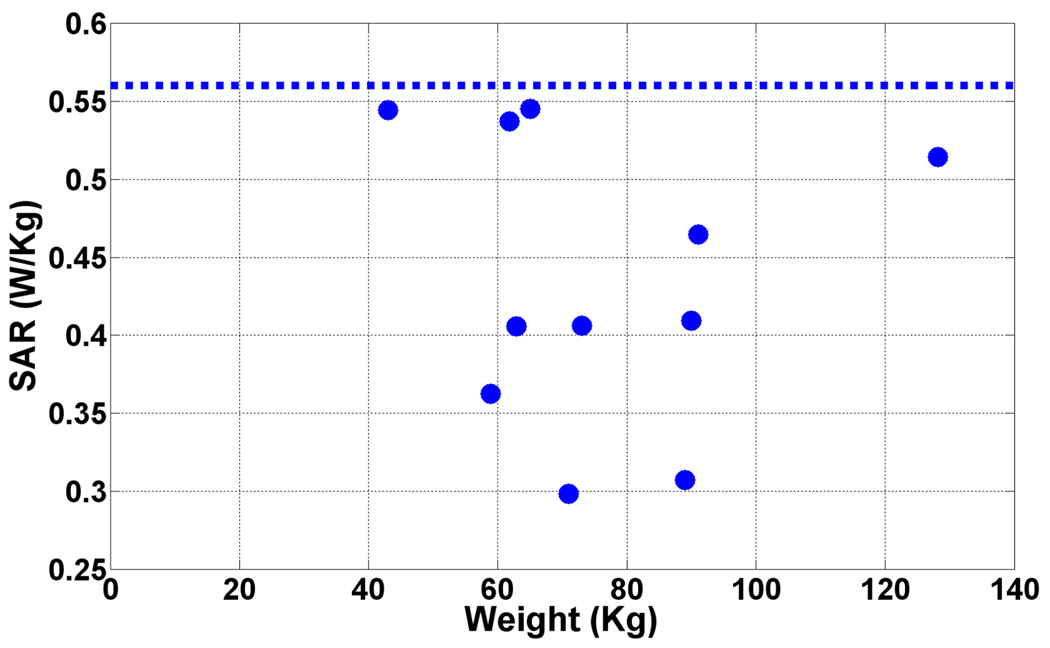
Eleven consenting subjects were scanned in a Philips 3T Achieva scanner. The scanner’s SAR (Power/weight) estimate was noted (5). For short pulses (~1ms), the scanner’s power monitor at the RF power amplifier agree with our system within 2±2%, but disagreed for longer modulated pulses (~7ms). Figure 3 shows that the scanner overestimates the delivered SAR in many cases.
Figure 3.
Measured SAR in 11 volunteers (solid dots) with long pulses. The dashed line is the scanner’s estimated SAR which is high.
Discussion
Determining the true power deposited in the body is a challenge. We successfully built a flexible, real-time multi-channel power monitoring system and determined the true power and SAR delivered to adult volunteers. This typically differed from the estimates provided by the scanner. Similar measurements are planned on other vendors’ scanners at various field strengths.
Acknowledgments
Support: NIH grant R01 EB007829
References
- 1.Shellock FG. JMRI. 2007;26:1182–1185. doi: 10.1002/jmri.21176. [DOI] [PubMed] [Google Scholar]
- 2.Stralka JP, et al. JMRI. 2007;26:1296–1302. doi: 10.1002/jmri.21141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. http://bit.ly/7WwfBT.
- 4.Bottomley, et al. Med. Phys. 2010;37:3828–3843. doi: 10.1118/1.3439590. [DOI] [PubMed] [Google Scholar]
- 5.El-Sharkawy, et al. ISMRM. 2010;3853 [Google Scholar]