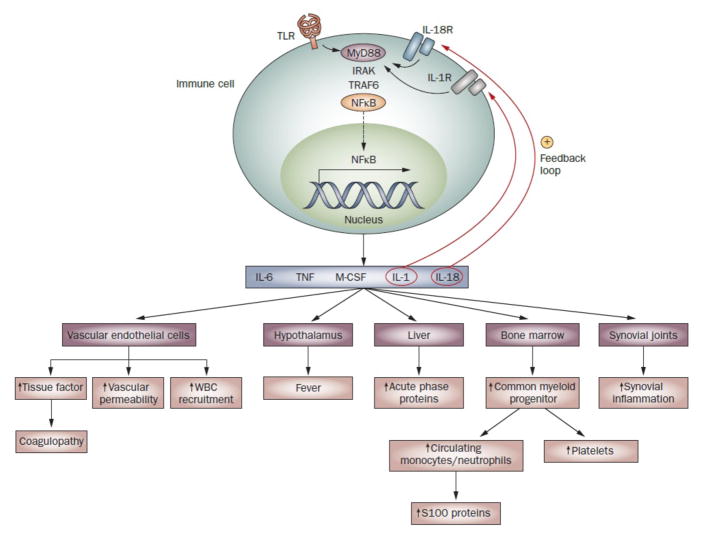
Figure 1.
Perpetuation of innate immune responses in sJIA. Innate immune pathways activated in sJIA are normally triggered by the recognition of pathogen-associated molecular patterns by TLRs expressed on innate immune cells, but can also be triggered by endogenous ligands in inflammatory conditions. These intracellular pathways lead to activation of the transcription factor NFκB, which is translocated into the nucleus where it upregulates expression of genes encoding several proinflammatory cytokines. These cytokines initiate the inflammatory cascade through their effects on the hypothalamus, bone marrow, liver and vascular endothelial cells. Activated vascular endothelial cells act as a procoagulant surface and are likely to contribute to the coagulopathy of sJIA.107 Antibodies against endothelial cells reportedly occur in sJIA,108 although the relevance of this latter finding is unclear. The cytokines also drive joint inflammation, by stimulating osteoclast-mediated bone resorption, osteoblast apoptosis, inhibition of chondrocyte proteoglycan synthesis and synoviocyte secretion of enzymes that degrade matrix and cartilage. Since signaling through IL-1R and IL-18R shares the downstream portion of the TLR4 signaling pathway, IL-1 and IL-18 provide positive feedback loops that further contribute to perpetuation of the inflammatory responses in sJIA. Abbreviations: IL-1R, IL-1 receptor; IL-18R, IL-18 receptor; M-CSF, macrophage colony-stimulating factor; NFκB, nuclear factor κB; sJIA, systemic juvenile idiopathic arthritis; TLR, Toll-like receptor; TNF, tumor necrosis factor; WBC, white blood cell.