Abstract
A major medical education need in Sub-Saharan Africa includes expanding clinical training opportunities to develop health professionals. Medical education expansion is a complicated process that requires significant investment of financial and human resources, but it can also provide opportunities for innovative approaches and partnerships. In 2010, the U.S. President's Emergency Plan for AIDS Relief (PEPFAR) launched the Medical Education Partnership Initiative to invest in medical education and health system strengthening in Africa. Building on a 30-year collaborative clinical and research training partnership, the University of Nairobi in Kenya developed a pilot regional medical education program modeled on the WWAMI (Washington, Wyoming, Alaska, Montana, and Idaho) medical education program at the University of Washington in the United States. The University of Nairobi adapted key elements of the WWAMI model to expand clinical training opportunities without requiring major capital construction of new buildings or campuses. The pilot program provides short-term clinical training opportunities for undergraduate students and recruits and trains clinical faculty at 14 decentralized training sites. The adaptation of a model from the Northwestern United States to address medical education needs in Kenya is a successful transfer of knowledge and practices that can be scaled up and replicated across Sub-Saharan Africa.
Calls for medical education reform in Sub-Saharan Africa come from multiple stakeholders and prioritize increasing the number of students trained, revising core curricula to align with existing demands, improving teaching approaches, and addressing the maldistribution of physicians.1-3 Policymakers and educational institutions are increasingly recognizing the benefits of collaborative approaches to sharing best practices, including international partnerships.1,3 The University of Nairobi in Kenya and the University of Washington in the United States have collaborated for more than 30 years on medical and public health research, training, and service programs that build capacity in both institutions. With funding from the U.S. President's Emergency Plan for AIDS Relief (PEPFAR), through the Medical Education Partnership Initiative (MEPI), the two institutions have leveraged their partnership to develop and implement a program to expand clinical training opportunities at the largest medical school in Kenya without the need for major capital investment such as construction of new buildings or campuses.
In this article the authors, who have been involved in the partnership, present how it led to the development of a pilot regional medical education model based on the University of Washington's 43-year-old WWAMI (Washington, Wyoming, Alaska, Montana and Idaho) program.4 We describe key elements of the WWAMI program that we adapted to the Kenyan setting and consider directions for additional growth and expansion.
New Opportunity for Partnerships
The past decade has seen renewed focus on improving health-sector educational capacity in African countries, with the involvement of multinational and bilateral donors, private and corporate foundations, and African ministries of education and health.5 Common elements of successful partnerships among academic institutions in the United States, Canada, and Western Europe and academic faculty or institutions in Sub-Saharan Africa include strong local leadership and input into the agenda, development of clear strategic plans by the African partner, frequent bi-directional communication among leaders, and developing expertise across disciplines at the African institutions.6,7 These elements are the foundation for the strong partnership between the University of Nairobi and University of Washington collaborative research and training programs.
For example, the AIDS International Training and Research Program (AITRP), funded by the Fogarty International Center at the National Institutes of Health (NIH), has focused on Kenya as one of its primary target countries for training. During the past 25 years, AIRTP has supported 153 short- and long-term opportunities at the University of Washington for future Kenyan researchers, of whom more than one-third are affiliated with the University of Nairobi. Many Kenyan AITRP trainees who have trained at the University of Washington have made important scientific contributions and assumed leadership positions at the University of Nairobi. In addition, several University of Washington investigators and faculty members have spent substantial time in Kenya contributing to a robust collaborative relationship with reciprocal learning. The activities of these investigators have been both supported and shaped by their involvement in AITRP.8
In 2010, PEPFAR launched the MEPI program through the Office of the U.S. Global AIDS Coordinator in the U.S. Department of State and the NIH. MEPI funding directly supports 13 African institutions to strengthen existing and build new clinical and research capacity in Sub-Saharan African medical educational institutions and to strengthen the human resource capacity for health.5 In response to MEPI's call for proposals, a core group of faculty and administrators from the College of Health Sciences at the University of Nairobi, the School of Medicine and Department of Global Health at the University of Washington, and the School of Medicine at the University of Maryland, Baltimore, developed a pilot program to address challenges facing medical schools in Kenya, including the need for more clinical training opportunities. To address the dual objectives of improving instructional capacity and expanding the quantity of adequately trained medical professionals, the team proposed to adopt key elements of the WWAMI model to lay the foundation for a regional medical education model at the University of Nairobi College of Health Sciences from 2011 to 2015.
Regional Medical Education in the Northwest U.S.
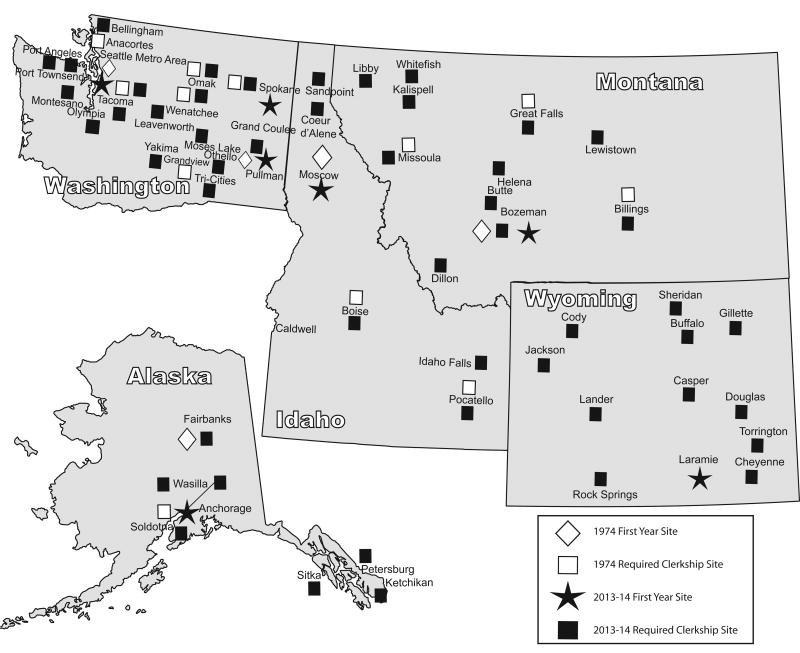
Medical education in the United States has seen fluctuation in the number and capacities of medical schools needed to train an optimal number, skill mix, and geographic distribution of physicians.4,9 In 1971, the University of Washington School of Medicine developed a community-based regional medical education program in response to a national need for more physicians. The founding goals of the program were to provide publicly supported medical education to citizens of the Northwest, create community-based medical education, increase the number of primary care physicians, and address the maldistribution of physicians in a cost-effective way.4 The WWAMI model includes regional campuses with a partner university in each of the five states and clinical training opportunities across a region where more than one-third of the population lives in rural, underserved areas. In 2013, more than 5,000 community faculty physicians in more than 180 active clinical sites taught students in required and elective clerkships (Figure 1). Settings include community clinics, private practices, and affiliated hospitals; students choose a combination of states and sites for their required and elective clerkships. In addition, many sites are used to train medical residents and serve as centers for continuing medical education for physicians and other health care professionals. The WWAMI model has been successful because of partnerships with physicians, local and state medical associations, other health care organizations, and state governments.10
Figure 1.
In the WWAMI model, first-year basic sciences are offered at the Seattle, Washington, campus and at five regional campuses. Second-year medical students train in Seattle, and students in the third and fourth years are offered clerkship sites located in Seattle and in the five-state region. In 1974, University of Washington School of Medicine students could choose from 10 sites in four states outside of Seattle. In 2013, there were 180 locations across five states involved in training physicians. This includes six first-year sites and more than 130 required clerkship sites, including those outside of Seattle.
Medical Education in Kenya
Kenya, like many countries in Sub-Saharan Africa, faces a health workforce crisis that critically affects its capacity to improve health outcomes. Kenya suffers from a chronic loss of medical school graduates to other countries in Africa, Europe, and North America, as well as to non-governmental organizations.11 There is also a significant maldistribution of physicians within Kenya, with acute shortages overall, but especially in rural and underserved areas. In 2010, 32% of all physicians worked in Nairobi Province, which has only 8% of the population. This maldistribution characterizes the preference of physicians to be situated in urban areas, and highlights the challenge of retaining doctors in rural settings.12
As in the United States, strategies to address shortages and maldistribution of physicians in Kenya have included increasing enrollment at existing medical schools and developing new medical schools. Five public universities currently train doctors in Kenya. Prior to 2007, Kenya had only two medical schools; the three other public schools were accredited in the past five years. Each school has its own teaching and assessment methods but has a core curriculum mandated by the Kenya Medical Practitioners and Dentists Board and other regulating bodies.
The University of Nairobi has a long history of medical education, beginning in 1967 with the opening of the Faculty of Medicine. The College of Health Sciences was established in 1985 and includes the Schools of Medicine, Dental Sciences, Nursing Sciences, Pharmacy, Public Health and two institutes. The College of Health Sciences faces challenges to increase its graduate output. Most important among these are overcrowding of students in its tertiary teaching hospital, a limited number of faculty, and an increasing number of students. Over the past decade, an increase in the number of students has strained the capacity of both faculty and clinical teaching sites. Most of the clinical training is delivered in a tertiary setting at Kenyatta National Hospital, the primary teaching hospital for the College of Health Sciences. Although decentralized clinical training was previously identified as an option to reduce congestion of training in tertiary care settings, the University of Nairobi had not invested in decentralization because of its limited faculty capacity and lack of additional clinical teaching sites.
Engaging Leadership at All Levels
In October 2010, the NIH's Fogarty International Center awarded the University of Nairobi a five-year, $12.5 million grant in partnership with the University of Washington and the University of Maryland, to implement the Partnership for Innovative Medical Education in Kenya (PRIME-K) program. PRIME-K aims to enhance the quantity and quality of medical education, retain medical graduates and faculty, and support regionally relevant research. The University of Washington received a subcontract to support the development of a pilot decentralized training program that builds on key elements of the WWAMI model.
University of Nairobi leaders and College of Health Sciences faculty members involved in the PRIME-K program wanted to understand the development of the WWAMI program from its beginnings as an experimental medical education program in 1971 to a best-practice model with widespread participation in and ownership of the program by key stakeholders today. Initially, the College of Health Sciences faculty had several concerns, including that students would not receive high-quality clinical instruction and mentorship, that staff at the decentralized sites would lack motivation to teach students, and that sites would not have adequate facilities to support student learning. Interestingly, these were also significant concerns when the WWAMI program was started. To ensure that the PRIME-K program avoided these concerns and employed the same best practices that have led to WWAMI's continued success, PRIME-K leaders engaged with WWAMI faculty from the earliest planning stages to develop a pilot program and identify opportunities for expansion.
As a first step in developing the pilot program, a team including all health science deans and faculty leaders from the University of Nairobi and the Kenya Ministry of Health met with key stakeholders in the WWAMI program at University of Washington for 10 days in May 2011. Stakeholders included leadership from the University of Washington's Schools of Medicine, Nursing, Dentistry, Pharmacy and Public Health, regional deans of the WWAMI program, course directors, faculty members, and students. The University of Washington team emphasized that the WWAMI program gradually expanded its comprehensive approach to train and retain primary care health professionals through medical school education, graduate medical education, a physician assistant training program, and support for practicing health professionals. This approach has resulted in increased recruitment and retention of WWAMI-trained physicians in the region. The Kenyan team also visited clinical training sites in Eastern Washington and Idaho to gain an overview of the key strategies and administrative aspects of the program. The visit provided opportunities for knowledge exchange, discussion, and strengthening of relationships that have proven to be invaluable for program implementation.
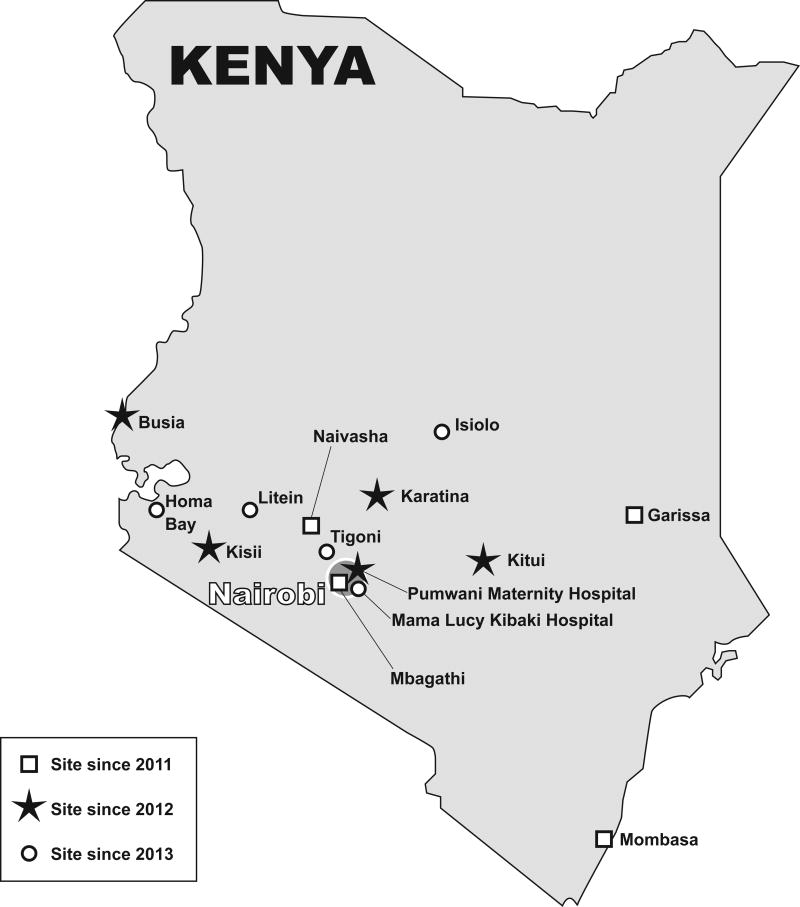
The PRIME-K program currently provides eight-weeks of elective clinical training for School of Medicine students in specific specialty areas, including obstetrics and gynecology, pediatrics and child health, internal medicine, surgery, and public health. This has been expanded to include short-term rotations for students from the Schools of Dental Sciences, Nursing Sciences, and Pharmacy at 14 non-tertiary health facilities across Kenya (Figure 2). Preclinical instruction and required clinical rotations take place at the University of Nairobi campuses and Kenyatta National Hospital in Nairobi. The College of Health Sciences leadership plans to have required clinical rotations for each of the schools occur at the network of decentralized training sites in the near future.
Figure 2.
The PRIME-K program has steadily increased the number of training sites since its inception. In 2011, the PRIME-K program partnered with four district and provincial hospitals as pilot sites. In 2012, five additional sites were added, including four district hospitals and a maternity hospital in Nairobi. In 2013, the program added five additional sites, for a total of 14.
Investing in Relationships
Over the past 40 years, a focus on partnerships among all stakeholders and participants across five states has been a key factor in WWAMI's success. Similarly, since its inception nearly four years ago, the PRIME-K program has emphasized dialogue and full partnership with key stakeholders in medical education to change training approaches in a sustainable manner. Some of these stakeholders include the Kenya Ministry of Health, the Ministry of Education, health professional regulatory authorities, and other universities. PRIME-K created an advisory board consisting of members of the College of Health Sciences management, the principal investigator, faculty members, and representatives from the Ministry of Health. The inclusion of government stakeholders on the advisory board helps ensure support for the program within the Ministry of Health and facilitates linkages with the national health professional regulatory authorities.
Building a Network of Training Sites
After the 2011 visit to the University of Washington, the College of Health Science's leadership and members of the PRIME-K program developed several criteria for pilot sites. Sites needed to be provincial or district hospitals that had been accredited by the Kenya Medical Board and the Ministry of Health to serve as internship sites for medical school graduates. Sites also needed to have medical specialists on staff and represent different geographical regions. Through an extensive consultation process with key stakeholders, the Ministry of Health leadership recommended that PRIME-K focus on four public hospitals as initial sites. The Ministry of Health provides guidance on site expansion and the program now includes 14 decentralized training sites across Kenya.
Developing Community-based Adjunct Faculty
A key element of the WWAMI program is ensuring the quality of clinical teaching and mentorship at the sites. Unpublished surveys of WWAMI physicians completed every five years indicate a sustained interest by volunteer faculty in participating in WWAMI because of the stimulation and enjoyment students bring to their practices despite the decreased clinical productivity these physicians report.10 WWAMI has found that faculty development, or teaching the faculty to teach, is a key element of success for decentralized training sites. In the PRIME-K program, health care workers from decentralized training sites who are interested in adjunct faculty positions at the University of Nairobi participate in a three-day training program on clinical teaching and mentoring delivered by faculty members. These faculty regularly visit the sites to support training activities and also provide lectures and clinical consultations for adjunct faculty. The College of Health Sciences has formalized a process for selection and accreditation of adjunct faculty, and many have been selected for these positions at the university.
Future Challenges and Opportunities for Growth
The partnership between the University of Nairobi and the University of Washington is built on clinical and research training collaborations that span more than 30 years. The process of adapting the WWAMI model in Kenya provides an opportunity to transfer knowledge and practices and strengthens the relationship between the two institutions. Both programs have strong evaluation components that actively include key stakeholders and use outcomes to guide program development and decision-making.
Since October 2011, more than 300 medical, nursing, dental, and pharmacy students have completed elective rotations; more than 180 staff members from decentralized sites have been trained in clinical teaching and mentoring; and approximately 30 staff have been accredited as adjunct faculty at the University of Nairobi. This initial accomplishment will pave the way for future PRIME-K activities as the program evolves, including training medical residents at attachment sites, recruiting students from rural and underserved areas, expanding the network of clinical sites to include private practices, and conducting a cost-effectiveness analysis of the program. These initiatives will leverage ongoing collaborations with the University of Washington and lessons learned by the WWAMI program.
As the WWAMI program evolves, strong partnerships will help it sustain and build the networks necessary to adapt to an ever-changing health care landscape. A similar approach can be used by the PRIME-K program to ensure that its training model meets the changing health workforce needs in Kenya. The WWAMI program has adapted over its 43-year history to address many unknown factors, including unpredictable funding sources and dynamic political processes. Strategic advocacy and partnerships will also help PRIME-K diversify funding mechanisms and expand clinical training opportunities for students at the University of Nairobi and across Kenya.
Acknowledgments
The authors acknowledge the design contributions of Brandon Guthrie, acting instructor of global health and epidemiology, University of Washington School of Public Health, and Todd Carey, program coordinator, regional affairs, University of Washington School of Medicine.
Funding/Support: Funding for this work came from MEPI through award number 1R24TW008889, funded by the Office of the U.S. Global AIDS Coordinator and the National Institutes of Health (NIH).
Footnotes
Other disclosures: None reported.
Ethical approval: Reported as not applicable.
Disclaimers: The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or any other agency.
Contributor Information
Ms. Mara J. Child, Clinical instructor of global health, University of Washington School of Public Health, and deputy director, Health Alliance International, Seattle, Washington.
Dr. James N. Kiarie, Associate professor of obstetrics and gynecology, College of Health Sciences, University of Nairobi, Nairobi, Kenya, and affiliate associate professor of global health and epidemiology, University of Washington School of Public Health, Seattle, Washington.
Dr. Suzanne M. Allen, Clinical professor of family medicine and vice dean for regional affairs, University of Washington School of Medicine, Seattle, Washington.
Dr. Ruth Nduati, Professor of pediatrics and child health, University of Nairobi College of Health Sciences, Nairobi, Kenya.
Dr. Judith N. Wasserheit, Professor of global health and medicine, adjunct professor of epidemiology, and vice chair of global health, University of Washington Schools of Medicine and Public Health, Seattle, Washington.
Dr. Minnie W. Kibore, Program coordinator for PRIME-K, University of Washington School of Public Health, Seattle, Washington.
Dr. Grace John-Stewart, Professor of global health, medicine, and epidemiology and adjunct professor of epidemiology, University of Washington Schools of Medicine and Public Health, Seattle, Washington.
Mr. Francis J. Njiri, Program monitoring and evaluation manager for PRIME-K, University of Nairobi College of Health Sciences, Nairobi, Kenya.
Dr. Gabrielle O'Malley, An associate professor of global health, and director of implementation science, I-TECH, University of Washington School of Public Health, Seattle, Washington.
Mr. Raphael Kinuthia, Training coordinator for PRIME-K, University of Nairobi College of Health Sciences, Nairobi, Kenya.
Dr. Tom E. Norris, Professor and chair of family medicine, University of Washington School of Medicine, Seattle, Washington.
Dr. Carey Farquhar, Professor of medicine and global health and adjunct professor of epidemiology, University of Washington Schools of Medicine and Public Health, Seattle, Washington.
References
- 1.Frenk J, Chen L, Bhutta ZA, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet. 2010 Dec 4;376(9756):1923–1958. doi: 10.1016/S0140-6736(10)61854-5. [DOI] [PubMed] [Google Scholar]
- 2.Greysen SR, Dovlo D, Olapade-Olaopa EO, Jacobs M, Sewankambo N, Mullan F. Medical education in sub-Saharan Africa: a literature review. Med Educ. 2011 Oct;45(10):973–986. doi: 10.1111/j.1365-2923.2011.04039.x. [DOI] [PubMed] [Google Scholar]
- 3.Mullan F, Frehywot S, Omaswa F, et al. Medical schools in sub-Saharan Africa. Lancet. 2011 Mar 26;377(9771):1113–1121. doi: 10.1016/S0140-6736(10)61961-7. [DOI] [PubMed] [Google Scholar]
- 4.Ramsey PG, Coombs JB, Hunt DD, Marshall SG, Wenrich MD. From concept to culture: The WWAMI program at the University of Washington School of Medicine. Acad Med. 2001 Aug;76(8):765–775. doi: 10.1097/00001888-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Mullan F, Frehywot S, Omaswa F, et al. The Medical Education Partnership Initiative: PEPFAR's effort to boost health worker education to strengthen health systems. Health Aff (Millwood) 2012 Jul;31(7):1561–1572. doi: 10.1377/hlthaff.2012.0219. [DOI] [PubMed] [Google Scholar]
- 6.Kolars JC, Cahill K, Donkor P, et al. Perspective: partnering for medical education in Sub-Saharan Africa: seeking the evidence for effective collaborations. Acad Med. 2012 Feb;87(2):216–220. doi: 10.1097/ACM.0b013e31823ede39. [DOI] [PubMed] [Google Scholar]
- 7.Kolars JC. Taking down ‘the Ivory Tower’: leveraging academia for better health outcomes in Uganda. Bmc International Health and Human Rights. 2011 Mar;11(Suppl 1):S1. doi: 10.1186/1472-698X-11-S1-S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Daniels J, Nduati R, Farquhar C. Kenyan women medical doctors and their motivations to pursue international research training. Education for health. 2013 May-Aug;26(2):89–97. doi: 10.4103/1357-6283.120700. [DOI] [PubMed] [Google Scholar]
- 9.Norris TE, Coombs JB, House P, Moore S, Wenrich MD, Ramsey PG. Regional solutions to the physician workforce shortage: The WWAMI experience. Acad Med. 2006 Oct;81(10):857–862. doi: 10.1097/01.ACM.0000238105.96684.2f. [DOI] [PubMed] [Google Scholar]
- 10.Allen SM, Ballweg RA, Cosgrove EM, et al. Challenges and Opportunities in Building a Sustainable Rural Primary Care Workforce in Alignment With the Affordable Care Act: The WWAMI Program as a Case Study. Acad Med. 2013;88:1862–1869. doi: 10.1097/ACM.0000000000000008. [DOI] [PubMed] [Google Scholar]
- 11.Machayo J, Keraro V. Brain drain among health professionals in Kenya: A case of poor working conditions? - A critical review of the causes and effects. Prim J Bus Admin Manage. 2013;3(6):1047–1063. [Google Scholar]
- 12.Dogbey B. Kenya Mobility of Health Professionals. Brussels, Belgium: International Organization for Migration; Mar, 2012. [Google Scholar]