Abstract
Acute lymphoblastic leukemia presenting with bone involvement and multiple osteolytic lesions has been commonly reported in pediatric population. Various myeloid and lymphoid malignancies can rarely present with bony lesions. We are reporting an adult female patient with acute lymphoblastic leukemia who presented with paraparesis and multiple osteolytic lesions in skull initially giving false impression of multiple myeloma.
Keywords: Acute lymphoblastic leukemia (ALL), Osteolytic lesions, Paraparesis
Case Report
A 27 year old female presented in September 2011 at Regional Cancer Centre JIPMER with complaints of back pain in lower thoracic area for 1 month. Pain was dull aching in nature, persisted throughout the day and not relieved or aggravated by change in posture. It progressed gradually during 1 month period. Patient developed acute onset weakness and numbness of both lower limbs 5 days before coming to the hospital. Patient initially was able to walk with support and over a period of 2 days became bed ridden.
Fig. 1.
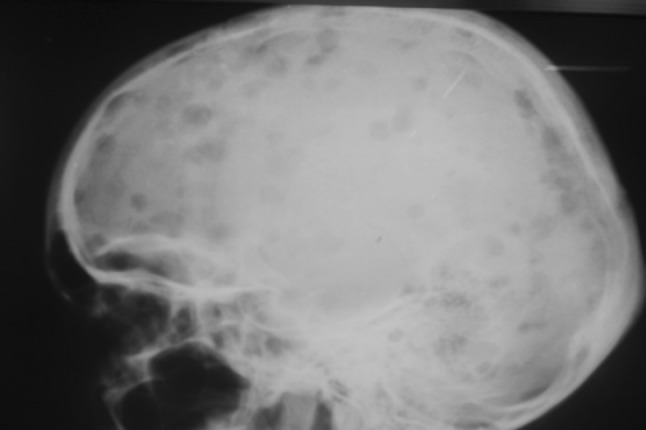
X-ray skull lateral view showing multiple osteolytic lesions
Fig. 2.
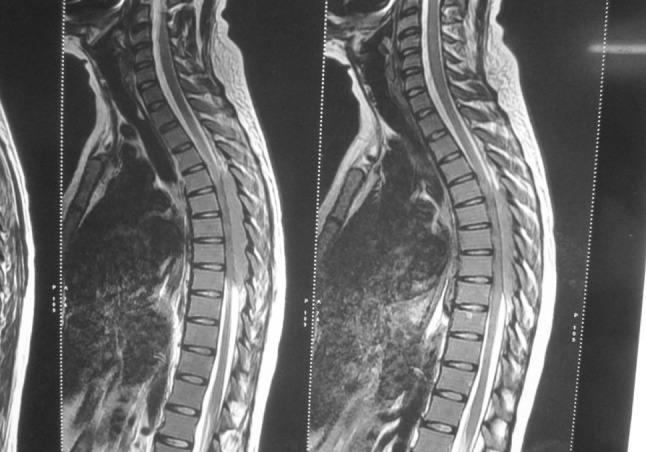
MRI spine-poorly defined T1 hypointense lesion measuring 80.6 × 9.3 (CC × AP) mm noted in the spinal canal in the dorsal subarachnoid space at D4–D8 levels compressing the cord. The lesion is predominantly involving the dorsal and right lateral aspect displacing the cord anteriorly
There was no history of headache, vomiting, chest pain, cough, expectoration, bone pains, bleeding, recurrent infections, radicular pain, band like sensation, bladder and bowel involvement or trauma.
Past history was significant as patient was diagnosed as a case of megaloblastic anemia in March 2010 and treated with B12 and folate supplementation with partial improvement. Later on she was lost to follow up.
General examination was unremarkable except mild pallor. Examination of neurological system revealed normal higher mental function, no cranial nerve involvement and absence of neck rigidity. Weakness of both lower limbs was present (power 3/5 in both limbs). Tone was normal and deep tendon reflexes were increased. Bilateral planters were extensor. Pain and temperature sensations were diminished (50 %) below T6 spinal level. Examination of abdomen, chest, cardiovascular system, musculoskeletal system and breast was within normal limits.
Investigations performed during hospital stay are given in the table below
| Investigations | Results |
|---|---|
| Hemogram | Hb = 8 g/dl, TLC = 2,000/cmm, DLC = N32 %, L54 %, bands 2 %, blasts 12 %, platelets = 50,000/cmm |
| Peripheral smear | Normocytic normochromic RBC with increased rouleaux formation, leucopenia with relative lymphocytosis and blasts, moderate thrombocytopenia |
| Serum calcium | 9.0 mg/dl |
| Serum uric acid | 2.2 mg/dl |
| Serum LDH | 655 U/l |
| Serum phosphorus | 2.8 mg/dl |
| X-ray thoraco-lumbar spine | Normal study |
| X ray skull | Multiple punched out lesions (Fig. 1) |
| Urine Bence Jones protein | Negative |
| Serum electrophoresis | No M band seen |
| Serum FLC | Not done |
| MRI spine | Lesion in dorsal subarachnoid space compressing spinal cord from D4 to D8 level (Fig. 2) |
| MRI brain | Normal study |
| CSF study | Neutrophil, 2/cmm; lymphocyte, 16/cmm; cytospin-blasts present |
| CSF-immunophenotyping | Not done |
| Bone marrow aspiration | Blasts 92 %, SBB-negative |
| Bone marrow biopsy | Infiltration by Tdt+ve, CD10+ve, CD3−ve, and CD20−ve blasts suggestive of pre B ALL. Grade I marrow fibrosis present |
She was diagnosed as Pre B acute lymphoblastic leukemia with CNS involvement. Rest of the radiological survey was normal on X-Ray. MRI was not done for skeletal survey. Patient was initially investigated on the lines of Myeloma also. Bone marrow aspiration and biopsy findings were confirmative of acute lymphoblastic leukemia so lesion biopsy and serum FLC assay was not done. Patient was started on GMALL protocol with Triple intrathecal therapy. The weakness in both lower limbs started improving within 48 h so local site radiotherapy was not considered. Over 2 weeks period power improved to the extent of 4/5 with therapy. Post induction bone marrow examination was in remission and CSF was clear. Patient is currently having consolidation phase 1 chemotherapy and doing well.
Discussion
This patient presented with many unusual findings like initial presentation with back pain and paraparesis, presence of multiple lytic lesions in skull and no lymphadenopathy giving initial impression as a case of metastasis or multiple myeloma. We reviewed the literature and did a pubmed search to find the reported cases presenting in this manner.
Skeletal lesions can occur in various malignant hematological conditions. Myeloid and lymphoid malignancies can present with bone involvement and osteolytic lesions. In myloid neoplasms skeletal lytic lesions have rarely been described in acute megakaryocytic leukemia [1] and both chronic phase and blast crises of CML [2, 3]. Among lymphoid neoplasms non Hodgkins lymphoma, adult T cell leukemia, hairy cell leukemia, chronic lymphoid leukemia can present with bony lesions uncommonly [4]. Multiple myeloma, Waldenstrom’s macroglobulinemia, eosinophilic granuloma, are other conditions which have skeletal involvement and osteolytic lesion as a common presentation. Hypercalcemia can be present in these situations [5]. The mechanism leading to the lytic lesions noted in these patient remains uncertain. Probable causes of bony lesions may be involvement by tumor cells itself in leukemia, bone involvement in lymphoma or parathormone related peptide mediated.
Acute lymphoblastic leukemia is a common leukemia in childhood. They usually present with fever, bone and joint pains, bleeding manifestations, lymphadenopathy and hepatosplenomegaly. Case reports of children and adolescents presenting with bone pain and osteolytic lesions are plenty but only one adult patient with osteolytic lesion in acute lymphoblastic leukemia has been reported by Stein and Boughton [5] to the best of our knowledge.
Parathyroid hormone-related peptide (PTHrP) has been found to be elevated in serum in child presenting with generalized osteolytic lesion and hypercalcemia. Reverse transcriptase-polymerase chain reaction and immuno histochemistry showed in one study that lymphoblasts produced PTHrP directly [6]. Multiple osteolytic lesions with necrosis of bone marrow has also been reported in pediatric patients [7].
Our patient also had paraspinal mass and the initial presentation was paraparesis. Spinal cord compression is a rare but serious complication of leukemia. Reports of children presenting in similar fashion and undergone unnecessary surgery for mass lesion which turned out to be leukemia has been reported. A simple bone marrow examination in such patient can avoid surgery in such a patients [8].
Leukemic/lymphomatous masses spread via lymphatics and through intervertebral foramina and cause cord compression before bone destruction [9]. Plain X-rays may be falsely inefficient in detecting bony involvement in leukemias in comparison to primary or metastatic solid tumours [10]. Biopsy of the mass would be necessary for diagnosis in patients presenting with isolated paraspinal mass when overt clinical symptoms or findings or laboratory abnormalities suggestive of leukemia are absent. Examination of cerebrospinal fluid may help with the diagnosis. Acute lymphoid malignancies initial presentation with lower limb weakness is exceedingly rare. In one series of 1,412 children with acute lymphocytic leukemia only 5 (0.35 %) presented with a spinal mass [10]. Early chemotherapy, radiotherapy and physical rehabilitation offer the best chance of cure and functional recovery.
Conclusion
Hematological malignancies like acute lymphoblastic leukemia and lymphomas can rarely present with osteolytic lesions and neurological involvement in pediatric patients. We reported this patient for two reasons, first as this adult female with ALL presented with paraparesis due to paraspinal mass lesions and secondly was found on further investigations to have multiple osteolytic lesions in skull mimicking multiple myeloma. Complete work up lead to diagnosis of Pre-B acute lymphoblastic leukemia.
References
- 1.Muler JH, Valdez R, Hayes C, et al. Acute megakaryocytic leukemia presenting as hypercalcemia with skeletal lytic lesions. Eur J Haematol. 2002;68:392–396. doi: 10.1034/j.1600-0609.2002.02715.x. [DOI] [PubMed] [Google Scholar]
- 2.Kwong YL, Ng I, Leung S. Osteolytic skeletal lesions in chronic myeloid leukemia. Pathology. 1990;22:123–125. doi: 10.3109/00313029009063795. [DOI] [PubMed] [Google Scholar]
- 3.Kubota K, Yanagisawa T, Kurabayashi H, et al. Hypercalcemia associated with osteolytic lesions in the extramedullary blast crisis of chronic myelogenous leukemia: report of a case. Blut. 1989;59:458–459. doi: 10.1007/BF00349068. [DOI] [PubMed] [Google Scholar]
- 4.Rossi J, Bataille R, Chappard D, et al. B cell malignancies presenting with unusual bone involvement and mimicking multiple myeloma. Am J Med. 1987;83:10–16. doi: 10.1016/0002-9343(87)90491-8. [DOI] [PubMed] [Google Scholar]
- 5.Stein A, Boughton BJ. Common acute lymphoblastic leukaemia in an adult with hypercalcemia and lytic bone lesions. Br J Haematol. 1988;70:503. doi: 10.1111/j.1365-2141.1988.tb02526.x. [DOI] [PubMed] [Google Scholar]
- 6.Shimonodan H, Nagayama J, Nagatoshi Y. Acute lymphocytic leukemia in adolescence with multiple osteolytic lesions and hypercalcemia mediated by lymphoblast-producing parathyroid hormone-related peptide: a case report and review of the literature. Pediatr Blood Cancer. 2005;45(6):333–339. doi: 10.1002/pbc.20357. [DOI] [PubMed] [Google Scholar]
- 7.Abbas A, Husain AH, Abdelaal A, et al. Acute lymphoblastic leukemia presenting with extensive skeletal lesions and bone marrow necrosis. Med Pediatr Oncol. 2001;37:64–66. doi: 10.1002/mpo.1167. [DOI] [PubMed] [Google Scholar]
- 8.Buyukavci M, Karacan M, Olgun H, Tan H. Significance of bone marrow examination in the diagnostic process of paraspinal mass in children: a case report. J Pediatr Hematol Oncol. 2003;25(10):822–823. doi: 10.1097/00043426-200310000-00018. [DOI] [PubMed] [Google Scholar]
- 9.Ch’ien LT, Kalwinsky DK, Peterson G, et al. Metastatic epidural tumors in children. Med Pediatr Oncol. 1982;10:455–462. doi: 10.1002/mpo.2950100505. [DOI] [PubMed] [Google Scholar]
- 10.Pui C-H, Dahl GV, Hustu HO, Murphy SB. Epidural spinal cord compression as the initial finding in childhood acute leukemia and non Hodgkin lymphoma. J Pediatr. 1985;106:788–792. doi: 10.1016/S0022-3476(85)80357-7. [DOI] [PubMed] [Google Scholar]


