Abstract
To assess the impact of Medicaid expansion for pregnant women in South Carolina and California, the authors compared change in rates of timely prenatal care, adverse infant and maternal health outcomes, and use of cesarean section for groups of pregnant women who were either uninsured or covered by Medicaid, versus women with private coverage. The results showed small and/or inconsistent changes. Provision of coverage may be the first logical step in improving health care for the uninsured, but outcomes may rely more on outreach, coordination of care, and non-medical interventions than on provision of insurance coverage per se.
Introduction
The United States has for many years ranked poorly in infant survival compared with other nations in the developed world (Liu et al., 1992; Dorgan, 1995). Although many factors contribute to this poor performance, concern about limited access to prenatal care has been particularly broad. Uninsured women may be up to five times as likely to delay prenatal care until late in pregnancy. They have a much higher rate of adverse health outcomes, including low birthweight and prematurity (Haas et al., 1993). Moreover, sick uninsured newborns receive fewer resources while in the hospital (Braveman et al., 1991).
Since its creation in 1965, Medicaid has been one of this country's most important vehicles for improving access to health care for the poor. Originally, however, Medicaid coverage for pregnant women was limited to a subset of the indigent population. The program provided coverage for pregnant women who were recipients of Supplemental Security Income or of Aid to Families with Dependent Children (AFDC), a group comprised of very poor unmarried mothers and their children (with incomes that were on average 47 percent of the Federal poverty level [FPL] in 1986). However, pregnant women without disability who were married, first-time mothers or who had incomes above the AFDC cutoff were excluded. Beginning in 1981, Federal legislation progressively expanded eligibility. Sequentially, Federal law required States to extend Medicaid coverage to all pregnant women with family incomes below the AFDC eligibility level, below 75 percent of the FPL, then 100 percent of the poverty level, and finally, by 1990, 133 percent of the poverty level. In addition, States were allowed to extend coverage to those with incomes up to 185 percent of the poverty level and receive Federal matching funds.
As might be expected, the Federal legislation has had a large impact on enrollment of pregnant women. For example, between 1987 and 1990, nearly 2.6 million more pregnant women enrolled in Medicaid. As of July 1994, 33 States and the District of Columbia set eligibility income limits beyond the minimum required (133 percent of the FPL) (Loranger and Lipson, 1995).
Despite the importance of the Medicaid expansion, study of its impact has proven difficult. States have been understandably reluctant to pursue randomized experiments. Use of administrative data to evaluate State-based “natural experiments” has not been easy. With rare exceptions, birth certificates lack information on insurance coverage, so these data by themselves cannot be used to study changes in prenatal care or health outcome by groups of women covered by Medicaid or other specific insurance coverage (Braveman et al., 1993). Instead, studying the utilization of prenatal care has depended on expensive and time-consuming linkages of birth certificates with hospital records or other administrative data (Haas et al., 1993; Haas, Udvarhelyi, and Epstein, 1993).
In this study we used such linked data to examine changes in prenatal care and infant and maternal health outcomes associated with Medicaid expansion in two States, South Carolina and California. We chose these States because of the availability of requisite data and because they represent different regions of the country.
Methods
Overall Strategy
Our goal was to assess the effect of providing Medicaid coverage to otherwise uninsured pregnant women on access to timely prenatal care, health outcomes, and use of medical services.
In South Carolina, Medicaid covered pregnant women with incomes below 100 percent of the FPL as of October 1987. In June 1989, Medicaid coverage was expanded to cover women with incomes up to 185 percent of the FPL. We were able to obtain South Carolina data for calendar years 1988-91. We used data on all births in calendar year 1988 and in the first 5 months of 1989 to characterize the pre-expansion period and all births between March 1, 1990, and December 31, 1991, to characterize the post-expansion period. The “post” years were chosen to ensure that eligible women could be covered by Medicaid for their entire pregnancy.
In California Medicaid covered pregnant women with incomes below 110 percent of the FPL as of 1986. In July 1989, Medicaid coverage was expanded to cover women with incomes up to 185 percent of the FPL. We were able to obtain California data for calendar years 1989-91, giving us 1 year less of pre-expansion data than in South Carolina. We used data on all births between January 1, 1989, and June 30, 1989, to characterize the pre-expansion period and all births between April 1, 1990, and December 31, 1991, to characterize the post-expansion period.
One key design issue concerns the study groups. We initially considered examining separately the change in process of care and health outcomes for two groups—the Medicaid population and those who were uninsured. However, we were concerned that separate comparisons of the process and outcomes of care of those groups pre- versus post-expansion would be misleading. We speculate, for example, that women in California with incomes between 110 percent and 185 percent of the FPL might be healthier than women with incomes below 110 percent of that level. Because the post-expansion group would then have included healthier women, comparison of outcomes pre- versus post-expansion for solely the Medicaid population would have shown improvement on this basis irrespective of whether the expansion had altered any individual's behavior or health outcome. We therefore examined the change in patterns of prenatal care and health outcomes for all women who were either uninsured or covered by Medicaid in the pre-expansion period compared with all women who were uninsured or covered by Medicaid in the post-expansion period. To control for temporal trends in the process of care and adverse birth outcomes, we used privately insured patients as a concurrent control group.
Data Sources
Hospital discharge abstracts for all South Carolina and California residents hospitalized respectively in a South Carolina or California hospital were used to identify all in-hospital deliveries of a single-gestation live birth of at least 500 grams during the study years noted. Insurance status was based on primary payer at the time of delivery. International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) (Public Health Service and Health Care Financing Administration, 1980) procedure and diagnosis codes were used to identify mothers and their infants from the discharge abstracts. The South Carolina and California birth registries provided birth certificate data on all births during the same time period.
Data Merging
We were required to link mother's discharge abstract data, infant's discharge abstract data, and infant's birth certificate data for each delivery because each of the three data files contained different variables that were part of our analysis. To preserve confidentiality, the State of South Carolina performed the merger of records from that State. The data elements used for matching included: hospital, mother's date of birth, baby's date of birth, baby's race, mother's race, presence of cesarean section, baby's sex, county and ZIP Code of residence, health insurance number, and birthweight. Data elements were matched sequentially until there was a unique match.
Successful merges were obtained for 46,368 deliveries in 1988 and the first 5 months of 1989 (65.6 percent of birth certificate records, 71.8 percent of mothers' discharge abstract records, 76.0 percent of infant discharge abstract records) and 86,813 deliveries in the last 10 months of 1990 and 1991 (88.1 percent of birth certificate records, 91.4 percent of mothers' discharge abstract records, 91.3 percent of infant discharge abstract records). The match rates are higher in 1990 and 1991 because several variables, including ZIP Code, mother's date of birth, and cesarean section were available in more than one data source (i.e., both mother's discharge abstract and birth certificate) then but not in 1988-89. The match rate is higher for discharge abstracts because the State did not obtain complete hospital records, and hence the denominator is smaller for discharge abstracts. This should not cause any appreciable bias because the rate of missing abstracts is modest (5-10 percent), and even if abstracts were systematically rather than randomly missing (e.g., by payer status), that bias would be present in both years and would minimally affect our analysis of the change over time. From the pre-expansion period, 923 matched records (1.99 percent) and 1,816 matched records from the post-expansion period (2.09 percent) were excluded for one or more of the following reasons: out-of-hospital births, multiple gestation, birthweight under 500 grams, unknown payer, or Medicare or other non-Medicaid government payer.
For California we obtained the raw discharge abstract and birth certificate files and excluded records indicating out-of-State residency, multiple gestation, birthweight under 500 grams, delivery at home or in a hospital with less than 10 deliveries annually, unknown payer, mother's age under 14 years or over 42 years or fetal death (ICD-9-CM code 656.4, fetal death; and procedure codes 73.8, destruction of fetus; 74.3, ectopic pregnancy; and 74.91 and 75.0, termination). We then performed the linkage ourselves using a probabilistic matching algorithm in two stages (Newkombe et al., 1959; Felligi and Sunter, 1969; Dubois, 1969; Bell et al., 1992). First, we linked baby's birth certificate and mother's discharge abstract using a series of variables that included hospital, cesarean section, baby's date of birth, ZIP Code of residence, mother's date of birth, and race. Successful merges were obtained for 240,735 deliveries in the first 6 months of 1989 (95.3 percent of mothers' discharge abstracts, 92.1 percent of birth certificates), and 956,902 deliveries between April 1, 1990, and December 31, 1991 (95.6 percent of mothers' discharge abstracts, 92.2 percent of birth certificates). The success of the merge in California was greater than that in South Carolina because of differences in the number and character of common variables on the different data sets.
In a second stage, we linked these combined records to the infant discharge abstracts. However, because the infant discharge abstracts lacked data on mother's date of birth, the match rate was lower. Three-way matches were obtained for 189,602 deliveries in 1989 (75.1 percent of mothers' discharge abstracts, 72.5 percent of birth certificates, 74.7 percent of infant discharge abstracts) and 736,705 deliveries in 1990-91 (73.6 percent of mothers' discharge abstracts, 71.0 percent of birth certificates, 73.4 percent of infant discharge abstracts). We used data from the two-way match for all analyses except for those that involved intrauterine growth retardation (IUGR)/prematurity and baby's length of stay (i.e., baby's length of stay greater than mother's length of stay and mother's length of stay greater than baby's length of stay) because these variables were based on data from the baby's discharge abstracts. For analyses of prematurity and length of stay we used the subset of patients with a three-way match.
Outcome Variables
We examined variables that were indicators of access to timely prenatal care, infant and maternal health outcomes, and utilization of care. To examine access to care, we used birth certificate data to characterize women by whether they had initiated care during the first trimester and whether they had initiated care before the third trimester. The adverse birth outcomes analyzed were low birthweight (less than 2,500 grams), IUGR/prematurity (ICD-9-CM codes 764.0-765.1), and baby's length of hospital stay longer than mother's length of stay. To assess adverse maternal outcome, we examined whether the mother's length of stay was at least 1 day longer than her infant's stay. We also examined utilization of cesarean section. All data on adverse outcomes were obtained from discharge abstracts except for low birthweight, which was recorded on birth certificates.
Data Analysis
To examine the effect of the program on the principal study variables, we first calculated rates for indices of timely prenatal care, adverse infant and maternal outcomes, and use of cesarean section for each payer group. To control for temporal trends in potential confounders, we directly standardized pre-expansion period rates to post-expansion population characteristics based on mother's age, race, level of education, and marital status. (Standardizing post-expansion rates to pre-expansion characteristics would not have materially affected our estimates.) We term these standardized rates “raw.” We compared these raw rates for the uninsured/Medicaid population with those of the privately insured. To assess the effect of the program, we examined the change in the interpayer difference for these rates between the pre-expansion period and the post-expansion period. Our hypothesis was that the Medicaid expansion would narrow the gap in timely prenatal care and health outcomes between the uninsured/Medicaid women and women with private health insurance. We also expected that expansion of Medicaid would be associated with an increase in use of cesarean section for uninsured/Medicaid women relative to women with private insurance. Confidence intervals (CIs) for pre-expansion to post-expansion differences in rates were calculated using standard techniques (Kleinbaum, Kupper, and Morgenstern, 1982). Records with missing values for mother's age, race, level of education, and marital status (1.7 percent of births in South Carolina and 2.5 percent of births in California) were excluded from these analyses.
Confounding from Decline in Private Insurance
Between the pre- and post-expansion years, the proportion of women with private insurance decreased in both States by 6 to 7 percentage points. This may have come from employers' dropping private insurance in response to the expansion of Medicaid coverage (Cutler and Gruber, 1996). We call those who dropped private coverage “switchers.” Because the switchers may have been on average better risks (i.e., they may have had better access to care and better health outcomes) than the Medicaid/uninsured group for reasons apart from their coverage, we were concerned that the decline in private coverage might have led to a factitious improvement in measured access to care and outcomes.
Our strategy was to bound the possible improvement that could have come from a changed risk mix. We treated the raw or standardized estimates as an upper bound on the improvement that may have occurred from the insurance expansions, because those estimates would attribute any remaining uncontrolled improvement in the risk mix among the Medicaid/uninsured group to the provision of insurance. To derive a lower bound, we performed a simulation that held constant the proportion with Medicaid or no insurance at post-expansion levels but assumed that the decline in private insurance came at random from the privately insured population. To the degree that the decline in fact did not come at random but rather came from those who were worse-than-average risks among the privately insured population (i.e., the poorer risks were more likely to lose private coverage), our estimate will understate the gain from the expansion of coverage. We term the simulated numbers “adjusted” values. If the variables we use to standardize, such as mother's education, control well for risk, the raw and adjusted values should tell the same story, and in fact they do.
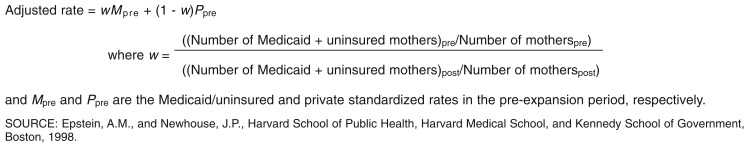
Specifically, to calculate adjusted numbers, we simulated a comparison in which the proportions of the population that were privately insured and Medicaid/uninsured remained constant at the post-expansion levels. We imposed constant proportions by simulating a switch from private insurance to Medicaid/uninsured in the pre-expansion period. We first determined the proportion of privately insured in the pre-expansion period that would be required to lose coverage to make the proportions of privately insured and Medicaid/uninsured equal the post-expansion values. We then constructed “adjusted” pre-expansion rates that equaled the weighted average of the Medicaid/uninsured pre-expansion standardized rate and the private pre-expansion standardized rate, where the weight on the Medicaid/uninsured rate equaled their pre-expansion share/post-expansion share and the weight on the private rate was (1 -the Medicaid/uninsured weight). The resulting expression is shown in Figure 1.
Figure 1. Adjusting Rates to Account for the Decline in Private Insurance.
For example, in South Carolina, in the pre-expansion period, 60.0 percent of the population was privately insured, and 40.0 percent was covered by Medicaid or was uninsured (Table 1), whereas in the post-expansion period, 52.9 percent of the population was privately insured, and 47.1 percent was covered by Medicaid or uninsured. To arrive at an adjusted, pre-expansion, Medicaid-plus-uninsured rate, we calculated the sum of South Carolina's Medicaid/uninsured pre-expansion rate times 0.4/0.471, plus the pre-expansion private rate times 0.071/0.471. This allowed us to simulate a comparison of pre-expansion versus post-expansion patterns of care in which 52.9 percent of the population in both periods was privately insured and 47.1 percent of the population was Medicaid/uninsured, and the additional Medicaid/uninsured in the pre-period were a random sample from the private group. In California we performed a similar adjustment. Variances were computed as a weighted average of the variances of the means that were being combined.
Table 1. Characteristics of the Study Population1.
| Characteristic | South Carolina | California | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Pre-Expansion2 | Post-Expansion3 | Pre-Expansion4 | Post-Expansion3 | |||||
|
|
|
|
|
|||||
| Number | Percent | Number | Percent | Number | Percent | Number | Percent | |
| Number | 45,455 | — | 84,997 | — | 241,284 | — | 958,738 | — |
| Mean Age | 25 ± 5.6 | — | 24 ± 5.7 | — | 26.7 ± 5.7 | — | 26.8 ± 5.9 | — |
| Primary Payer | ||||||||
| Medicaid | 12,465 | 27.4 | 35,726 | 42.0 | 78,798 | 32.7 | 391,351 | 40.9 |
| Uninsured | 5,709 | 12.6 | 4,287 | 5.0 | 25,694 | 10.7 | 78,882 | 8.2 |
| Private | 27,271 | 60.0 | 44,984 | 52.9 | 136,243 | 56.6 | 486,669 | 50.9 |
| Race | ||||||||
| White | 27,174 | 60.0 | 51,130 | 60.3 | 114,494 | 47.6 | 399,829 | 41.8 |
| Black | 18,149 | 40.0 | 33,648 | 39.7 | 21,025 | 8.7 | 76,038 | 8.0 |
| Hispanic | — | — | — | — | 77,968 | 32.4 | 371,456 | 38.9 |
| Other, Not White5 | — | — | — | — | 26,986 | 11.2 | 108,657 | 11.4 |
| Education | ||||||||
| High School Graduate | 34,278 | 75.5 | 64,454 | 76.0 | 68,817 | 29.5 | 315,207 | 33.7 |
| Not High School Graduate | 11,120 | 24.5 | 20,296 | 24.0 | 164,810 | 70.5 | 620,108 | 66.3 |
| Marital Status | ||||||||
| Married | 31,284 | 68.8 | 55,651 | 66.1 | 169,092 | 70.2 | 642,743 | 67.1 |
| Not Married | 14,158 | 31.2 | 28,511 | 33.9 | 71,643 | 29.8 | 314,159 | 32.8 |
| Access to Care | ||||||||
| Care Initiated in the First Trimester | 29,678 | 65.9 | 58,856 | 69.6 | 175,561 | 73.6 | 690,548 | 72.8 |
| Care Initiated Before the Third Trimester | 40,614 | 90.1 | 78,273 | 92.5 | 221,804 | 93.0 | 886,954 | 93.5 |
| Adverse Infant Health Outcomes | ||||||||
| Low Birthweight | 3,411 | 7.5 | 6,304 | 7.4 | 12,264 | 5.1 | 44,825 | 4.7 |
| IUGR/Prematurity | 2,693 | 5.9 | 6,023 | 7.1 | 10,770 | 5.7 | 38,408 | 5.2 |
| Baby's LOS Greater than Mother's LOS | 4,837 | 10.7 | 9,890 | 11.6 | 15,431 | 8.1 | 58,691 | 8.0 |
| Adverse Maternal Health Outcomes | ||||||||
| Mother's LOS Greater than Baby's LOS | 1,203 | 2.70 | 1,596 | 1.9 | 3,242 | 1.7 | 12,135 | 1.7 |
| Utilization | ||||||||
| Cesarean Section | 10,920 | 24.0 | 19,823 | 23.3 | 54,855 | 22.9 | 210,262 | 22.0 |
Includes all births in South Carolina and California for which mother and newborn discharge abstracts were merged with birth certificate data.
1988.
1990-91.
1989.
Includes Asian and Native American births.
NOTES: LOS is length of stay. Percentages may not add to 100 percent because of rounding. Numbers may not add to totals because of missing data. IUGR is intrauterine growth retardation.
SOURCE: Epstein, A.M., and Newhouse, J.P., Harvard School of Public Health, Harvard Medical School, and Kennedy School of Government, Boston, 1998.
Results
Patient Population
Table 1 displays the characteristics of the study population in the two study States during the 2 study years. The proportion of pregnant women covered by Medicaid increased substantially in both South Carolina (27 percent to 42 percent) and California (33 percent to 41 percent). The proportion of pregnant women who were uninsured decreased (13 percent to 5 percent and 11 percent to 8 percent in South Carolina and California, respectively), as did the proportion with private insurance (60 percent to 53 percent and 57 percent to 51 percent, respectively).
Changes in overall patterns of care and health outcomes were inconsistent (Table 1). For example, in South Carolina but not California, the proportion of pregnant women initiating care in the first trimester increased (from 66 to 70 percent). In spite of this evidence that access improved overall in South Carolina, the proportion of infants in that State with IUGR/prematurity and the proportion with length of stay greater than mother's length of stay increased. Use of cesarean section went down in both States.
Changes by Payer in South Carolina
Table 2 shows raw and adjusted rates in South Carolina of initiation of prenatal care, adverse infant and maternal outcomes, and use of cesarean section in the pre-expansion and post-expansion periods for pregnant women who had Medicaid or who were uninsured, and women with private coverage. The adjusted rates are adjusted for the decline in private insurance; both the raw and adjusted rates are standardized to population characteristics in terms of age, education, marital status, and race during the post-expansion period.
Table 2. Rates and Confidence Intervals for Selected Measures of Care for Medicaid/Uninsured Women and Women With Private Insurance: South Carolina, 1988-91.
| Measure | Statistical Adjustment | Before Medicaid Expansion 1988-89 | After Medicaid Expansion 1990-91 | Difference in Risk3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||||
| Medicaid/Uninsured Rate | Private Rate | Difference in Risk1 | Medicaid/Uninsured Rate | Private Rate | Difference in Risk2 | Rate | 95-Percent Confidence Interval | ||||
|
|
|
||||||||||
| Rate | Confidence Interval | Rate | Confidence Interval | ||||||||
| Initiation of Care During the First Trimester | Raw | 48.5 | 72.5 | -23.99 | -25.07, -22.91 | 58.6 | 76.3 | -17.66 | -18.46, -16.86 | 6.33 | 4.99, 7.67 |
| Adjusted | 51.9 | 72.5 | -20.64 | -21.64, -19.63 | 58.6 | 76.3 | -17.66 | -18.46, -16.86 | 2.98 | 1.69, 4.26 | |
| Initiation of Care Before the Third Trimester | Raw | 84.0 | 93.1 | -9.15 | -9.89, -8.41 | 89.9 | 94.5 | -4.59 | -5.11, -4.08 | 4.56 | 3.66, 5.46 |
| Adjusted | 85.3 | 93.1 | -7.87 | -8.58, 7.16 | 89.9 | 94.5 | -4.59 | -5.11, -4.08 | 3.28 | 2.40, 4.16 | |
| Low Birthweight | Raw | 8.4 | 7.3 | 1.09 | 0.43, 1.76 | 8.1 | 6.6 | 1.43 | 0.93, 1.93 | 0.34 | -0.50, 1.17 |
| Adjusted | 8.2 | 7.3 | 0.94 | 0.31, 1.57 | 8.1 | 6.6 | 1.43 | 0.93, 1.93 | 0.49 | -0.32, 1.29 | |
| IUGR/Prematurity | Raw | 6.4 | 6.0 | 0.37 | -0.23, 0.97 | 7.6 | 6.5 | 1.09 | 0.60, 1.58 | 0.72 | -0.06, 1.49 |
| Adjusted | 6.4 | 6.0 | 0.32 | -0.24, 0.88 | 7.6 | 6.5 | 1.09 | 0.60, 1.58 | 0.77 | 0.02, 1.51 | |
| Baby's LOS Greater than Mother's LOS | Raw | 14.0 | 9.0 | 5.07 | 4.29, 5.84 | 13.8 | 9.6 | 4.17 | 3.56, 4.78 | -0.90 | -1.88, 0.09 |
| Adjusted | 13.4 | 9.0 | 4.37 | 3.64, 5.10 | 13.8 | 9.6 | 4.17 | 3.56, 4.78 | -0.20 | -1.15, 0.75 | |
| Mother's LOS Greater than Baby's LOS | Raw | 3.0 | 2.8 | 0.19 | -0.22, 0.59 | 2.1 | 1.7 | 0.39 | 0.13, 0.64 | 0.20 | -0.28, 0.68 |
| Adjusted | 2.9 | 2.8 | 0.16 | -0.22, 0.54 | 2.1 | 1.7 | 0.39 | 0.13, 0.64 | 0.23 | -0.23, 0.68 | |
| Cesarean Section | Raw | 21.3 | 25.1 | -3.76 | -4.84, -2.68 | 20.7 | 25.1 | -4.45 | -5.23, -3.67 | -0.69 | -2.02, 0.64 |
| Adjusted | 21.9 | 25.1 | -3.24 | -4.23, -2.25 | 20.7 | 25.1 | -4.45 | -5.23, -3.67 | -1.21 | -2.47, 0.05 | |
Medicaid/uninsured compared with private insurance, 1988-89.
Medicaid/uninsured compared with private insurance, 1990-91.
Medicaid/uninsured compared with private insurance, 1988-89 to 1990-91.
NOTES: Both raw and adjusted analyses are directly standardized to post-expansion population characteristics to account for temporal changes in mother's age, race, level of education, and marital status. Adjusted analyses are weighted to adjust for decline in the proportion of persons with private insurance during the study years. LOS is length of stay. IUGR is intrauterine growth retardation.
SOURCE: Epstein, A.M., and Newhouse, J.P., Harvard School of Public Health, Harvard Medical School, and Kennedy School of Government, Boston, 1998.
To assess the impact of the Medicaid expansion, we examined the change between 1988-89 and 1990-91 in the interpayer differences between women covered by Medicaid or who were uninsured on the one hand and privately insured women on the other. For example, in 1988-89 the raw difference in the proportion of South Carolina women initiating care in the first trimester was 24.0 percentage points (48.5 percent versus 72.5 percent). This decreased to 17.7 percentage points after Medicaid expansion yielding an improvement of 6.3 percentage points (95-percent CI 5.0 to 7.7). The adjusted rates suggest that changes in the provision of private coverage likely accounted for up to one-half of the observed increase in the proportion of pregnant women initiating care in the first trimester. After adjustment, the interpayer difference in the pre-expansion period in the proportion of women initiating care in the first trimester was 20.6 percentage points (51.9 percent versus 72.5 percent). This difference decreased to 17.7 percentage points during the post-expansion period, an improvement of 3.0 percentage points (95-percent CI, 1.69, 4.26). Raw and adjusted rates of initiation of care before the third trimester also improved for the Medicaid/uninsured group.
Despite these improvements in timely initiation of care, our analyses showed no improvement in infant and maternal health outcomes for women who had coverage with Medicaid or who were uninsured. For example, in 1988-89, the raw interpayer difference between women covered by Medicaid or who were uninsured and privately insured women in the rate of low birthweight was 1.1 percentage points. We hypothesized that the interpayer difference would decrease significantly. However, the findings were contrary to our expectations—an increase in the interpayer difference to 1.4 percentage points in 1990-91, a change that was not statistically significant. The pattern in both raw and adjusted analyses was similar for the other health outcomes we assessed, except baby's length of stay greater than maternal length of stay, which showed an improvement that was not statistically significant. Also contrary to expectations, relative use of cesarean section did not increase for the Medicaid/uninsured population.
Changes by Payer in California
We performed a parallel set of analyses using data from California (Table 3). Contrary to expectation, the results provide evidence that Medicaid was associated temporally with reduction in the early initiation of prenatal care. For example, the raw data suggest that the interpayer difference in the proportion of women initiating care in the first trimester increased from 16.8 percent to 17.3 percent. After adjustment for the change in the proportion of the population covered by private insurance, the interpayer difference increased from 14.8 percent to 17.3 percent, a change of 2.5 percentage points (95-percent CI, 2.1-3.0 percent).
Table 3. Rates and Confidence Intervals for Selected Measures of Care for Medicaid/Uninsured Women and Women With Private Insurance: California, 1989-91.
| Measure | Statistical Adjustment | Before Medicaid Expansion 1988-89 | After Medicaid Expansion 1990-91 | Difference in Risk3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||||
| Medicaid/Uninsured Rate | Private Rate | Difference in Risk1 | Medicaid/Uninsured Rate | Private Rate | Difference in Risk2 | Rate | 95-Percent Confidence Interval | ||||
|
|
|
||||||||||
| Rate | Confidence Interval | Rate | Confidence Interval | ||||||||
| Initiation of Care During the First Trimester | Raw | 62.8 | 79.5 | -16.78 | -17.20, -16.36 | 64.2 | 81.5 | -17.26 | -17.47, -17.05 | -0.48 | -0.95, -0.01 |
| Adjusted | 64.8 | 79.5 | -14.76 | -15.16, -14.36 | 64.2 | 81.5 | -17.26 | -17.47, -17.05 | -2.50 | -2.95, -2.05 | |
| Initiation of Care Before the Third Trimester | Raw | 89.1 | 96.0 | -6.90 | -7.17, -6.64 | 91.0 | 97.0 | -5.99 | -6.11, -5.87 | 0.91 | 0.62, 1.21 |
| Adjusted | 89.9 | 96.0 | -6.07 | -6.33, -5.82 | 91.0 | 97.0 | -5.99 | -6.11, -5.87 | 0.08 | -0.20, 0.37 | |
| Low Birthweight | Raw | 5.7 | 4.5 | 1.15 | 0.94, 1.34 | 5.1 | 4.3 | 0.81 | 0.71, 0.91 | -0.34 | -0.58, -0.10 |
| Adjusted | 5.5 | 4.5 | 1.01 | 0.81, 1.22 | 5.1 | 4.3 | 0.81 | 0.71, 0.91 | -0.20 | -0.43, 0.02 | |
| IUGR/Prematurity | Raw | 6.0 | 5.2 | 0.75 | 0.50, 1.01 | 5.4 | 5.0 | 0.44 | 0.32, 0.57 | -0.31 | -0.59, -0.03 |
| Adjusted | 5.9 | 5.2 | 0.67 | 0.43, 0.90 | 5.4 | 5.0 | 0.44 | 0.32, 0.57 | -0.23 | -0.49, 0.04 | |
| Baby's LOS Greater than Mother's LOS | Raw | 9.7 | 6.9 | 2.78 | 2.48, 3.08 | 9.0 | 6.8 | 2.18 | 2.03, 2.33 | -0.60 | -0.93, -0.26 |
| Adjusted | 9.4 | 6.9 | 2.47 | 2.18, 2.75 | 9.0 | 6.8 | 2.18 | 2.03, 2.33 | -0.29 | -0.61, 0.03 | |
| Mother's LOS Greater than Baby's LOS | Raw | 2.1 | 1.5 | 0.61 | 0.47, 0.76 | 1.9 | 1.4 | 0.51 | 0.44, 0.58 | -0.11 | -0.27, 0.05 |
| Adjusted | 2.0 | 1.5 | 0.55 | 0.41, 0.68 | 1.9 | 1.4 | 0.51 | 0.44, 0.58 | -0.04 | -0.19, 0.11 | |
| Cesarean Section | Raw | 20.7 | 24.3 | -3.60 | -4.02, -3.19 | 20.6 | 23.5 | -2.92 | -3.13, -2.72 | 0.68 | 0.22, 1.14 |
| Adjusted | 21.1 | 24.3 | -3.17 | -3.56, -2.79 | 20.6 | 23.5 | -2.92 | -3.13, -2.72 | 0.25 | -0.19, 0.68 | |
Medicaid/uninsured compared with private insurance, 1989.
Medicaid/uninsured compared with private insurance, 1990-91.
Medicaid/uninsured compared with private insurance, 1989 to 1990-91.
NOTES: Both raw and adjusted analyses are directly standardized to post-expansion population characteristics to account for temporal changes in mother's age, race, level of education, and marital status. Adjusted analyses are weighted to adjust for decline in the proportion of persons with private insurance during the study years. LOS is length of stay. IUGR is intrauterine growth retardation.
SOURCE: Epstein, A.M., and Newhouse, J.P., Harvard School of Public Health, Harvard Medical School, and Kennedy School of Government, Boston, 1998.
We also examined adverse health outcomes and use of cesarean section. The raw data showed relative improvement among the Medicaid/uninsured population in infant health outcomes and an increase in use of cesarean section. For example, interpayer differences in low birthweight decreased from 1.15 percent to 0.81 percent, a change of 0.34 percentage points (95-percent CI>0.10, -0.58 percent). After adjustment the improvements in rates of low birthweight, IUGR/prematurity, and baby's length of stay greater than mother's length of stay diminished but remained of borderline statistical significance (p = 0.08, p = 0.10, p = 0.08, respectively). The change in use of cesarean section was no longer statistically significant.
Patterns of Care for High-Risk Subgroups
We performed a similar set of analyses in both States for women with less than a high school education and for black women. In South Carolina the results were qualitatively similar to those in the overall analyses. In California there were some minor differences. Among women without a high school education, those who were uninsured or covered by Medicaid were relatively less likely to initiate care in the first trimester after the expansion; the findings for initiation of care before the third trimester, however, disappeared. In both raw and adjusted analyses, the improvements in rates of low birthweight and IUGR/prematurity were statistically significant (p < 0.05). For black women, deterioration in timely initiation of care was not evident. Even after adjustment, the improvements in rates of low birthweight and newborn length of stay greater than mother's length of stay and the increase in use of cesarean section were statistically significant.
Discussion
Expansion of Medicaid to cover a greatly increased proportion of poor, uninsured pregnant women has been one of the most prominent health policy initiatives during the latter part of the 1980s and 1990s. The legislative program was developed to improve access to care and birth outcomes for poor pregnant women who, without Medicaid, would otherwise have been uninsured. The Medicaid expansion almost undoubtedly led to substantial increased enrollment of these individuals, with a commensurate increase in Federal and State expenditures (Liska et al., 1995). Information on the impact of this program on access to prenatal care and birth outcomes is of substantial policy importance.
Our findings confirm that legislation to expand Medicaid coverage led to substantial increases in the proportion of pregnant women enrolled in Medicaid in the two study States; however, the effects on access to care and health outcomes in our study were inconsistent. In South Carolina the expansion of Medicaid was associated with a small improvement in timely initiation of prenatal care but no apparent improvement in the outcomes of care. In California statistics on timely initiation of care actually deteriorated for those who were uninsured or covered by Medicaid. Infant health outcomes appeared to improve, although the numbers that were adjusted for change in the proportion of the population with private insurance were of borderline statistical significance.
Braveman and colleagues previously noted that access barriers persisted after Medicaid eligibility expansion for patients in California who were uninsured or covered by Medicaid. Yet it may seem counterintuitive that statistics for these groups on timely initiation of care actually deteriorated. The explanation may lie in concurrent changes in the California medical delivery system (Loranger and Lipson, 1995). Before the Medi-Cal eligibility expansion, financial barriers for uninsured pregnant women were offset by the State-funded Community Based Perinatal Services Program. Assuming that the Medicaid expansions would obviate the need for alternative coverage, the State phased out the Community Based Perinatal Services Program and may have, in fact, reduced access for women who remained uninsured.
Previous studies that examined changes in the process and outcomes of prenatal care in relation to expanded Medicaid coverage have shown inconsistent effects. Piper, Ray, and Griffin (1990) examined the expansion of Medicaid in Tennessee to married women without a concomitant change in income eligibility or the eligibility-determination process. The study showed no change in first trimester prenatal care or birth outcomes, although women directly affected by the mandate could not be separated from the statewide sample. Haas et al. (1993) and Haas, Udvarhelyi, and Epstein (1993) examined Healthy Start, a program in Massachusetts that was a prototype for the Medicaid expansion. This program provided coverage for pregnant women with incomes of up to 185 percent of the FPL who would otherwise have been uninsured. Again there was no significant impact on either patterns of prenatal care or health outcomes (Haas et al., 1993; Haas, Udvarhelyi, and Epstein, 1993). Dubay et al. (1995) examined the association of Medicaid expansion with changes in the proportion of women receiving early prenatal care in Tennessee, California, Georgia, and Michigan. Only Tennessee showed an increase, although the data were aggregate State numbers that were not broken down by payer.
Currie and Gruber (1996) analyzed aggregate State data and found that Medicaid expansion in the late 1980s had no impact on infant health, but earlier expansions targeted at poor women reduced incidence of low birthweight. Coulam et al. (1995) analyzed national vital statistics files and found a small but significant association between Medicaid expansions and reduced rates of delayed prenatal care and poor birth outcomes, including preterm birth and low birthweight. This group of analysts also examined the impact of Medicaid expansion in Missouri in January, 1998. They found that despite a substantial increase in enrollment, low-income women did not increase their utilization of prenatal care services or show improved birth outcomes. More recently, Long and Marquis (1997) examined the impact of Medicaid expansion in Florida and found an improvement in early initiation of care and the proportion of infants born with low birthweight. They attributed this positive impact in part to contemporaneous growth in the public health delivery system.
Perhaps it should not be surprising that the impact of Medicaid expansion on initiation of care and health outcomes is either small or inconsistent across different States. Provision of coverage per se is only one aspect of health care policy that affects access to prenatal care. We have already noted concurrent changes in the California “safety net” that may have affected access to care for uninsured pregnant women. Others have noted impediments to access such as bureaucratic problems in the application and certification process and a shortage of obstetrical providers willing to accept Medicaid patients (Loranger and Lipson, 1995). These factors, as well as outreach, undoubtedly vary across States. Even if provision of insurance coverage leads to improved access, the impact of prenatal care on birth outcomes such as low birthweight may be small, especially for patients who are not at particularly high risk (Huntington and Connell, 1994; Strobino et al., 1995; Strobino et al., 1986; Peoples, Grimson, and Daugherty, 1984; Expert Panel on the Content of Prenatal Care, 1989; Kaestner, 1998).
Our study has important limitations. First, our data include limited measures of the process of care. In California, there was a deterioration in early initiation of care, although health outcomes showed some improvement. Presumably, this improvement was related to changes in the process of care other than the time of initiation. Administrative records contain limited clinical information and no data on smoking or drinking; it is possible that unmeasured clinical factors may have affected our findings. There may be other clinical conditions that are prevented or ameliorated by prenatal care that were not adequately included in our database. For example, anemia may be an important source of maternal morbidity, but it is not reliably recorded in hospital discharge abstracts. We were unable to merge data for all of the patients. Change in the number of illegal aliens in California may have affected the composition of the uninsured group. The primary payer noted at time of delivery was assumed to be the payer for both delivery and prenatal care. Some individuals may have lost or gained insurance during the prenatal period. Finally, our study included only two States. There is substantial variation among State Medicaid programs. Our findings are instructive, but it would be premature to generalize nationally.
Finally, our investigation is quasi-experimental. Because infant mortality is a multifaceted problem that encompasses broader issues such as poverty and poor education, it is possible that temporal changes in these and related areas accounted for our results. In particular, we noted a temporal decline in private insurance coverage. To control for its impact, we calculated adjusted rates by assuming a random loss of insurance within the insured cohort. This assumption implies that within the insured group, the loss of insurance is uncorrelated with the likelihood of a poor birth outcome. However, if those at a greater risk of a poor outcome within the privately insured group are more likely to lose insurance, our assumption of random loss of insurance will understate any improvement in outcomes attributable to the expansion of insurance. Because our raw or unadjusted figures probably overstate the improvement in outcomes, the unadjusted and adjusted figures should bound the true change under the plausible assumption that on average those losing private insurance were more likely than others with private insurance to have a poor birth outcome. Our qualitative conclusions about outcomes and initiation of care, however, are similar with both raw and adjusted data.
In summary, provision of insurance coverage appears to have an inconsistent impact on timely access to care and health outcomes. These results should be underscored as we move rapidly into an era of Medicaid managed care. Organizations that provide integrated care may be able to provide superior outreach and continuity of care to the Medicaid population. Further study of the impact of Medicaid expansion in States that utilize managed care seems particularly important. Provision of coverage may be the first logical step in improving access to prenatal care and related maternal and infant health outcomes for the Medicaid population. However, much remains to be done. The final solution may rely more on outreach and coordination of care and non-medical interventions than on provision of insurance coverage per se.
Acknowledgments
We are grateful to the Health Facility Data Division and the Department of Health Services in California; and the Division of Research and Statistical Services, the Department of Vital Statistics and the Hospital Association in South Carolina for providing us with data for this study. We appreciate programming assistance from Margaret Welch, programming and analytic assistance from Loraine Scampini and Margaret Volya, and help with manuscript preparation from Johanna Myers. We especially appreciate aid from Jennifer Haas, M.D., who generously provided advice on data merging and analytic approaches.
Footnotes
Arnold M. Epstein and Joseph P. Newhouse are with Harvard University. This work was supported by the Robert Wood Johnson Foundation. The opinions expressed herein are those of the authors and do not necessarily represent the views of the Harvard University, the Robert Wood Johnson Foundation, or the Health Care Financing Administration.
Reprint Requests: Arnold M. Epstein, M.D., M.A., Department of Health Policy and Management, Harvard School of Public Health, 677 Huntington Avenue, Boston, MA 02115.
References
- Bell RM, Keesey J, Schenker E, et al. The urge to merge: Linking vital statistics records and Medicaid claims for very low birthweight infants. Santa Monica: Rand; 1992. California, 1980-1987. [Google Scholar]
- Braveman PA, Egener S, Bennett T, Showstack J. Differences in hospital resource allocation among sick newborns according to insurance coverage. Journal of the American Medical Association. 1991 Dec 18;266(23):3300–3308. [PubMed] [Google Scholar]
- Braveman P, Bennett T, Lewis C, et al. Access to prenatal care following major Medicaid eligibility expansions. Journal of the American Medical Association. 1993 Mar 10;269(10):1285–1289. [PubMed] [Google Scholar]
- Coulam RF, Cole N, Irvin C, et al. Final report of the evaluation of the Medicare Catastrophic Care Act: Impacts on maternal and child health programs and beneficiaries. Cambridge, MA.: Abt Associates; Dec 19, 1995. Contract Number HCFA 500-87-0063. [Google Scholar]
- Currie J, Gruber J. Saving babies: the efficacy and cost of recent changes in the Medicaid eligibility of pregnant women. Journal of Political Economy. 1996 Dec;104(6):1263–1296. [Google Scholar]
- Cutler DM, Gruber J. Does Public Insurance Crowd Out Private Insurance? Quarterly Journal of Economics. 1996 May;111(2):391–430. [Google Scholar]
- Dorgan CA, editor. Statistical Record of Health & Medicine. New York: Gale Research, Inc.; 1995. [Google Scholar]
- Dubay LC, Kenney GM, Norton SA, Cohen BC. Local responses to expanded Medicaid coverage for pregnant women. The Milbank Quarterly. 1995;73(4):535–563. [PubMed] [Google Scholar]
- Dubois NSDA., Jr A solution to the problem of linking multivariate documents. Journal of the American Statistical Association. 1969 Mar;64(325):163–174. [Google Scholar]
- Expert Panel on the Content of Prenatal Care. Care for Our Future: The Content of Prenatal Care. Washington, DC.: U.S. Public Health Service; 1989. [Google Scholar]
- Felligi IP, Sunter AB. A theory of record linkage. Journal of the American Statistical Association. 1969 Dec;64(328):1183–1210. [Google Scholar]
- Haas JS, Udvarhelyi IS, Epstein AM. The effect of health coverage for uninsured women on maternal health and the use of a cesarean section. 1. Vol. 270. Journal of the American Medical Association; Jul 7, 1993. pp. 61–64. [PubMed] [Google Scholar]
- Haas J, Udvarhelyi IS, Morris CN, Epstein AM. The effect of providing health coverage to poor uninsured women in Massachusetts. 1. Vol. 269. Journal of the American Medical Association; Jan 6, 1993. pp. 87–91. [PubMed] [Google Scholar]
- Huntington J, Connell FA. For every dollar spent—the cost-savings argument for prenatal care. New England Journal of Medicine. 1994 Nov 10;331(19):1303–1307. doi: 10.1056/NEJM199411103311910. [DOI] [PubMed] [Google Scholar]
- Kaestner R. The Effect of Medicaid on the Content and Site of Prenatal Care. Chicago: Jan 5, 1998. Paper presented at the American Economic Association. [Google Scholar]
- Kleinbaum DG, Kupper LL, Morgenstern H. Epidemiologic research: Principles and quantitative methods. Belmont, CA.: Lifetime Learning Publications; 1982. [Google Scholar]
- Liska D, Oberman K, Lyons B, Long P. Medicaid expenditures and beneficiaries National and state profiles and trends, 1984-1993. The Kaiser Commission on the Future of Medicaid; Washington, DC.: Jul, 1995. [Google Scholar]
- Liu K, Moon M, Sulvetta M, Chawla J. International infant mortality rankings: a look behind the numbers. Health Care Financing Review. 1992;13(4):105–117. [PMC free article] [PubMed] [Google Scholar]
- Long SH, Marquis SM. The Effects of Florida's Medicaid Eligibility Expansion for Pregnant Women. American Journal of Public Health. 1998;88:371–376. doi: 10.2105/ajph.88.3.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loranger L, Lipson D. The Medicaid expansions for pregnant women and children. Washington DC: The Alpha Center; 1995. [Google Scholar]
- Newkombe HB, Kennedy JM, Axford SJ, James AP. Automatic linkage of vital records. Science. 1959 Oct 16;130(3381):954–959. doi: 10.1126/science.130.3381.954. [DOI] [PubMed] [Google Scholar]
- Peoples MD, Grimson RC, Daugherty GL. Evaluation of the effects of the North Carolina improved pregnancy outcome project: Implications for state-level decision making. American Journal of Public Health. 1984 Jun;74(6):549–554. doi: 10.2105/ajph.74.6.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piper JM, Ray WA, Griffin MR. Effects of Medicaid eligibility on prenatal care and pregnancy outcome in Tennessee. Journal of the American Medical Association. 1990 Nov 7;264(17):2219–2223. [PubMed] [Google Scholar]
- Public Health Service and Health Care Financing Administration. The International Classification of Diseases, 9th Revision, Clinical Modification. 2nd. Washington, DC.: U.S. Department of Health and Human Services; 1980. [Google Scholar]
- Strobino D, Chase GA, Kim YJ, et al. The impact of the Mississippi improved child health project on prenatal care and low birthweight. American Journal of Public Health. 1986 Mar;76(3):274–278. doi: 10.2105/ajph.76.3.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strobino D, O'Campo P, Schoendorf KC, et al. A strategic framework for infant mortality reduction: Implications for “Healthy Start.”. The Milbank Quarterly. 1995;73(4):507–533. [PubMed] [Google Scholar]