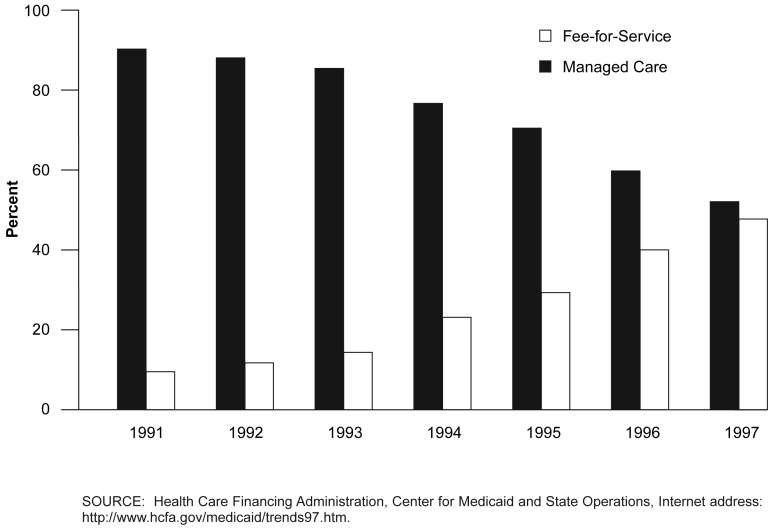
Figure 7. Distribution of Medicaid Enrollment: 1991-97.
Medicaid managed care enrollment has increased substantially since 1991.
- After experiencing large spikes in Medicaid spending in the 1988-91 period, States sought relief (as did employers) from skyrocketing costs by increasing enrollment in managed care. In Federal fiscal year (FY) 1991, managed care accounted for 9.5 percent of total Medicaid enrollment. By Federal FY 1997, nearly one-half (47.8 percent) of the Medicaid population was covered by some form of managed care.
- The Balanced Budget Act (BBA) of 1997 (Public Law 105-33) contained a number of provisions affecting Medicaid managed care plans. Under the BBA, States will be able to implement mandatory managed care programs without obtaining section 1915(b) or section 1115 waivers. States may also require most Medicaid recipients to enroll in managed care organizations (MCOs). Additionally, the MCOs are no longer required to enroll non-Medicaid members for 25 percent of total enrollment (Schneider, 1998). Most provisions of the BBA became effective in Federal FY 1998 and as such have had little effect on the 1997 figures.
- To date, however, most of the enrollment in Medicaid MCOs has been from comparatively low-cost groups (e.g., mothers and children) and relatively little from higher cost categories (the aged and disabled). Thus, the impact of increased MCO enrollment on Medicaid cost growth has been more modest than the nearly 50-50 enrollment distribution might suggest.