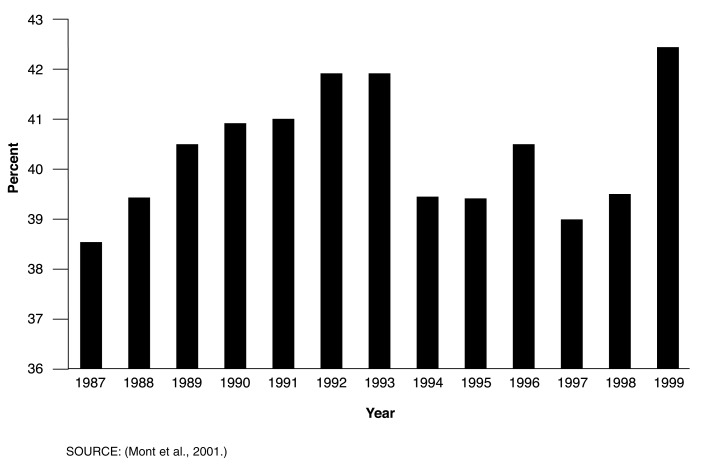
Figure 1. Workers' Compensation Medical Benefits as a Share of Total Workers' Compensation Benefits: United States, 1987-1999.
- Workers' compensation, financed by employers, provides benefits (including medical and rehabilitative expenses and partial wage replacement) to workers sustaining occupational injuries or diseases and survivor benefits to dependents. In 2000, medical benefits of $19.0 billion were paid through Federal and State programs; additional administrative and underwriting costs bring total expenditures to $23.3 billion (Centers for Medicare & Medicaid Services, 2002).
- All States except Texas mandate and set requirements for workers' compensation. Plans cover most, but not all, workers. The Federal Government maintains its own workers' compensation programs covering Federal civilian employees; longshore, harbor, and other maritime workers; and coal miners with black lung disease.
- From 1960 to 1981, medical benefits accounted for roughly 33 percent of total State workers' compensation benefits, before rising sharply to 42 percent in the early 1990s (Mont et al., 2001).
- Rising medical costs prompted employers to adopt managed care workers' compensation plans, a step that is in part credited with slowing cost growth. Additionally, lower injury rates, benefit changes, safety and return-to-work programs, anti-fraud measures, and tightening of eligibility standards likely contributed to slowing growth (Mont et al., 2001; American Academy of Actuaries, 2000).
- After several years of slowing, expenditure growth is rising again. The waning influence of managed care in controlling costs and an uptick in claim frequency are likely contributors to this trend. In addition, rising copayments and deductibles in non-workers' compensation medical plans may have resulted in some cost-shifting to workers' compensation plans (American Academy of Actuaries, 2000; Mont et al., 2001).