Abstract
Context:
Falls are a major public health problem in the elderly population. Fear of falling (FOF) among elderly persons can compromise quality of life by limiting mobility, diminished sense of well-being and reduced social interactions. India is undergoing a demographic transitional phase with urban elderly population of 6.72% in 2001. The major challenge would be on the prevention of falls among them. Hence there is a need to highlight the problems related to fall faced by the elderly in India.
Objective:
To study the prevalence of FOF and its correlates among the elderly population in urban area.
Materials and Methods:
250 elderly subjects above 60 years were randomly selected from urban area and interviewed for FOF using Short Fall Efficacy Scale-I (FES-I), history of falls and risk factors.
Results:
The prevalence of FOF among the elderly was 33.2%. The significant correlates of FOF were educational status, family type, associated health problems, history of fall in past 6 months, worried of fall again among fallers, fearfulness of fall again among fallers, restriction of daily activities and depression among them. The insignificant correlates were gender and socio-economic status.
Conclusion:
FOF is a health problem among the elderly living in urban India needs urgent attention. It represents a significant threat to socialization, independence and morbidity or mortality. Knowledge of correlates of FOF may be useful in developing multidimensional strategies to reduce it among elderly.
Keywords: Correlates, elderly, fall prevention, fear of falling, prevalence
INTRODUCTION
Ageing is a dynamic, progressive and physiological process accompanied by functional, morphological, biochemical and psychological changes. India being the second most populous country in the world has seen a sharp increase in the population of elderly and it has been projected that it would rise to about 324 million by 2050.[1] Falls are a major public health problem in the elderly population. Falls among them are recurrent and multifactorial episodes.[2,3] Every year accidental falls occur in nearly one-third of those aged more than 60 years, with 10% of these falls resulting in serious injury.[4] Falling in elderly persons can lead to disability, hospitalizations, and premature death.[5] It can also lead to reduced levels of independence, poorer quality of life, and high levels of anxiety.[6] Fear of falling (FOF) is a major health problem among the elderly living in communities, present in older people who have fallen but also in older people who have never experienced a fall. An estimated 30–55% of older persons acknowledge being afraid of falling, and approximately one third of them report restricting their activities. FOF has gained recognition as a specific health problem among older adults. The reported prevalence of FOF varied between 3–85%.[7] However, when FOF results in avoidance of activities and reduction of physical fitness, it is a risk factor for future falls and associated mortality, dysfunctioning, and premature nursing home admissions. FOF and activity avoidance may result in social isolation and inactivity, and threatens the quality of life if preventive measures are not taken in immediate future, the numbers of injuries caused by falls is projected to be 100% higher in the year 2030.[8]
Extensive research is available on the determinants and active ageing in developed countries, there is limited research on healthy ageing and FOF among elderly in developing countries like India. There is a lack of epidemiological, community based data on FOF from India and fall prevention is one of the issues that have not been given a sufficient attention. Hence the present study was planned to study the correlates of FOF in elderly Indian population living in urban area.
MATERIALS AND METHODS
The present cross-sectional study was undertaken in the urban field practice area in Raichur, Karnataka from June to August 2012. The research protocol was approved by the Institutional Ethics Committee. The study population comprised all elderly people above 60 years of age. The population served by the Urban Health Centre was 10,350. Hence the population of elderly would be around 1460 (8% of total population as per census). The sample size was calculated by software using Epi Info 7.0. The prevalence of fear of fall from previous study was taken as 25%, confidence limits of 5% and design effect as 1. The computed final sample for the present study was 241. The inclusion criteria was an elderly subject above 60 years of age and a resident from last 1 year in the study area. We obtained an informed written consent from the participants. The elderly who are relatives and visitors at the time of house visit were excluded. The elders with terminal illness and not willing to participate in the study were also excluded. The sample was obtained by systematic random sampling method. Data was collected using a standardised, semi-structured questionnaire and physical examination. A face-to-face interview was carried out with each of the participants at his or her home. The questionnaire collected information on socio-demographic characteristics. It also contained questions concerning falls, physical activity practice, activities of daily life (ability to watch TV, walk, taking shower, sit, lay down, stand up, going up and down stairs in an autonomous way), orthosis use, insomnia and reported morbidity. Falls history was assessed with a single item: how frequently have you fallen in the past 6 months. Height was measured using a wall-mounted stadiometer. Body weight was measured using standard weighing machine without shoes and the BMI was calculated from the values using the formula weight (kg)/height2 (m). The FOF was objectively assessed by using the Short Fall Efficacy Scale-I (FES-I). The Short FES-I is a seven-item shortened version of the FES-I and useful for practical purposes as requires less time and suitable for community based studies. The FES-I has excellent psychometric properties with very high internal reliability which have been demonstrated both in English and in a cross-cultural context.[9] Depression was assessed by geriatric depression scale short form that consist 15 questions. A score of ≥ 5 suggests depression. Data was entered in Microsoft Excel spreadsheet and analyzed using SPSS version 17.0 statistical software. For quantitative data, mean and standard deviation were computed. For qualitative data, proportions were computed. Appropriate tests of significance like chi-square and t test were used. Logistic regression was performed to test the association of FOF with other variables like age, gender, morbid conditions and other variables. All statistical tests were two-tailed, and a P value < 0.05 was considered statistically significant.
RESULTS
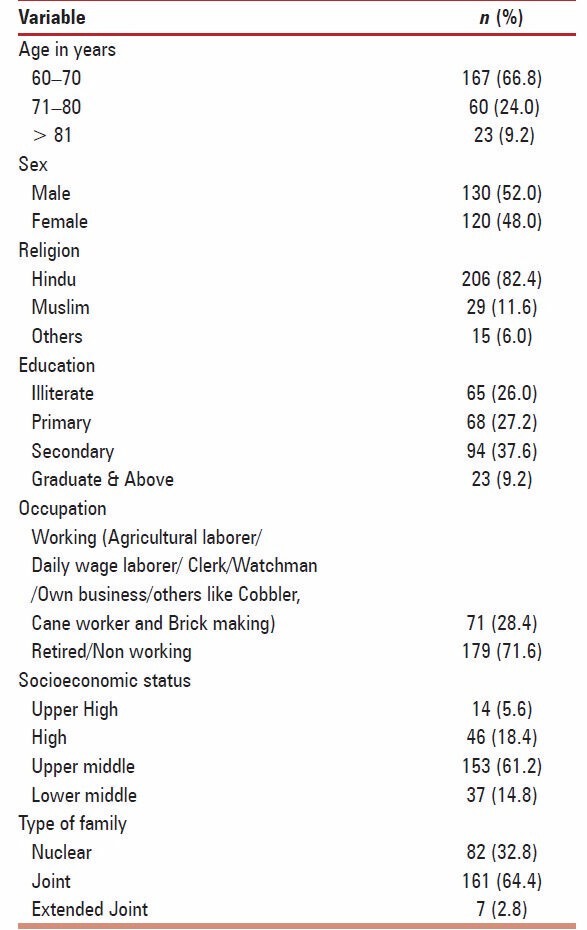
The sample consisted of 250 elderly above 60 years of age (range 60–96 years) that willingly participated in the present study. Fifty-two percent of these respondents were men and 48% were women. About 66.8% of respondents were within the age-group 60–70 years while those in the age group above 81 years were the least. The mean age ± standard deviation (SD) of all participants was 69.4 ± 7.5 years. The range of body mass index (BMI) was 15.2-31.4 with a mean ± SD of 23.9 ± 3.5 kg/m2 for the sample. Most of them were retired/not working, while only 28.4% were still working. Socio-demographic characteristics for the sample are summarized in Table 1.
Table 1.
Socio-demographic characteristics of participants
Altogether, 36.8% of the participants have experienced at least one fall within 6 months preceding the study. The nature of the fall was tripping or slipping in 63 (25.2%) elderly out of the total fallers. Following the fall, 63 (25.2%) sustained some injury like bruises and lacerations, 26 (10.4%) fractures and amongst 2 (0.8%), nothing significant. Majority of them (73.2%) had some associated illness like diabetes mellitus (34.4%), hypertension (18.8%), and other illnesses (22.0%) like asthma, CVA, rheumatoid arthritis, cancer, cataract/refractive errors etc. Depression (score > 5) was found in 11.2% of the elderly by use of geriatric depression scale. Delay in getting up after fall was reported by 12.4% of the elderly. The findings are shown in Table 2.
Table 2.
Characteristics of participants with regards to fall and fear of falling
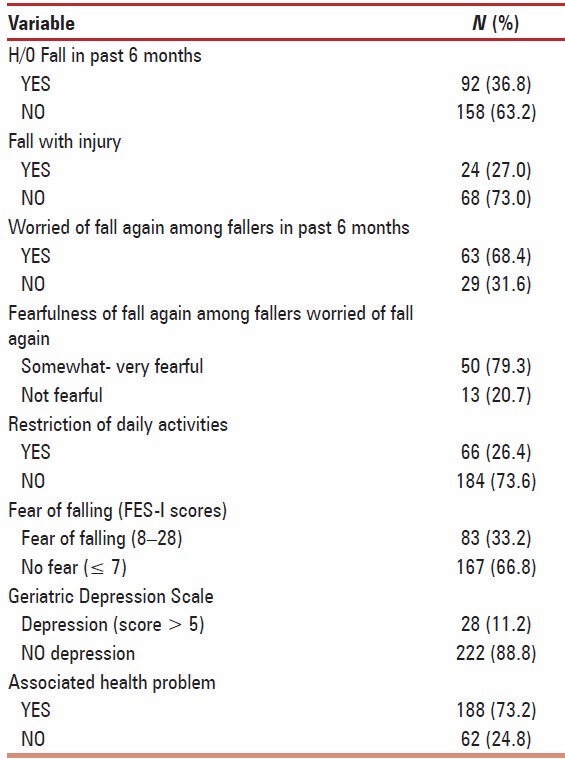
The prevalence of fear of fall assessed objectively among all the elderly by use of Short FES-I was 33.2%. Out of all, 36.8% of them gave a history of fall in past 6 months. Among the elderly who had a fall in past 6 months, 63.5% of them were worried about falling again. At the time of interview, 20% elderly were very fearful, 60.4% were somewhat fearful and remaining 19.6% were not fearful that they may fall again. With regards to restriction on daily activities after fall, 26.4% had restricted their activities. Among the elderly who had restricted daily activities, 45.4% had restricted to outdoors only, 30.3% had restricted to indoors only and remaining 24.3% had restricted to both indoor and outdoor.
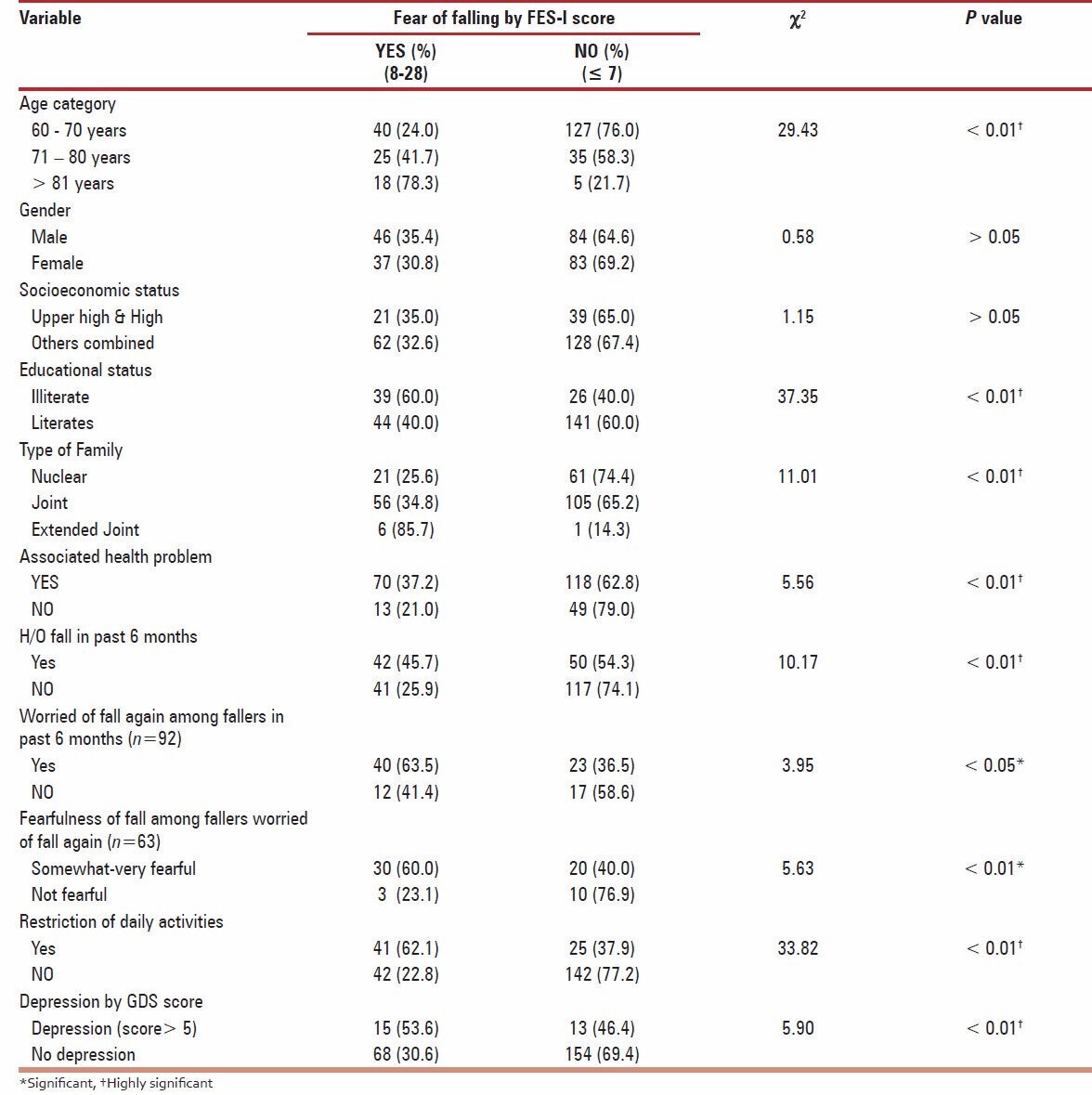
The variable FOF assessed by FES-I scale was dichotomized into FOF (score > 8) and no FOF (score < 7). The association between FOF and different variables was studied by applying chi-square test. It was observed that the prevalence of FOF increased with age and was statistically significant. No statistically significant gender differences were seen for FOF among men and women as shown in Table 3. FOF did not differ much in upper (35%) and lower socioeconomic groups (32.6%) and was statistically insignificant. Illiterates were found to have a significantly higher FOF (60%) as compared to literates (40%). Most of the elderly belonged to joint and extended joint families, they were found to have a higher FOF than elderly from nuclear family. The elderly who had an associated health problem had a higher FOF compared to elderly with no health problem and this difference was statistically significant. History of fall in past 6 months showed a significant association with FOF. We also observed that the FOF of 63.5% was found to be significantly higher among the fallers who were worried of falling again compared to those who were unworried. Higher FOF (60.0%) was found among fallers who were somewhat- very fearful at the time of interview than who were not fearful (23.1%). The elderly who had restricted their daily activities had a significantly higher FOF than who were ambulatory without any restriction of daily activities. Depression among elderly was significantly associated with development of higher FOF as compared to elderly without depression. The correlates of FOF among the elderly are shown in Table 3. We performed a stepwise logistic regression to determine predictors for FOF. The model derived from the logistic multivariate analysis showed that age (OR = 3.2, 95% CI = 3.0-4.2; P < 0.01), education (OR = 3.1, 95% CI = 1.3-6.9; P < 0.01), history of fall in past 6 months (OR = 2.6, 95% CI = 1.2-5.6; P < 0.01) and restriction of daily activities (OR = 3.6, 95% CI = 1.6-7.8; P < 0.001) were independently associated with FOF among the elderly.
Table 3.
Correlates of fear of falling among the participants
DISCUSSION
The results obtained from the present community based study showed that the prevalence of FOF among the elderly Indian population in urban (study) area was 33.2%. Hence FOF was common in this sample of elderly persons but lower to that reported as 44.2% by Kumar S et al.,[6] in a hospital based study. Similarly in another community based Indian study by Sebestina AD et al.,[10] reported fear of fall in 38.4% elderly participants. Community-based epidemiologic studies have found that 21–61%[11,12,13] of elderly people experience some degree of FOF. Community studies that are limited to elderly people who have actually fallen have reported prevalence rates of 32–83%,[14,15] strikingly 33–46% of community-dwelling elders who have not fallen also report FOF. In the present study, 45.7% subjects had FOF with history of fall and 25.9% subjects had FOF with no history of fall in last 6 months, consistent with previous reports. This suggests that the elderly develop the FOF with or without the history of falls. The correlation between falls and FOF has been well demonstrated[12,16,17] but the temporal relationship between these two syndromes in a population based sample is less clear. Previous studies[18,19] have found that increasing age is a significant predictor of FOF which is in consistent with the findings of present study to find an association between age and FOF. Advanced age is indicative of a decline in functional reserve and that the perception of these losses can generate a feeling of low self-esteem and FOF.[11,12,14,20] Andresen et al.,[21] did not detect any statistical correlation between ageing and fear of fall. The risk for FOF increases with age and may result from the accumulated effect of multiple conditions. In the present study, the significant correlates associated with FOF among elderly were age, educational status, type of family, associated health problem, history of fall in previous 6 months, restriction of daily activities and depression. This study also reveals the complexity of the FOF syndrome that needs a multifactorial approach to prevent it. In a study by Kempen G et al.,[22] found that female sex, restriction of activity of daily living and history of falls in previous 6 months were correlated independently with severe FOF. Restriction of daily activities was found among 62.1% elderly who had FOF. Activity restriction is, in itself, a risk factor for falls because it can lead to muscle atrophy, deconditioning, poorer balance and reduced physical conditioning. Curtailment of activities can also lead to social isolation.[12,23,24] Thus, FOF can contribute to both functional decline and impaired quality of life. In summary, there is a growing body of evidence that suggests, FOF may constitute an important risk factor for unnecessary restriction of activity.[24,25] Depression and anxiety are commonly found in people experiencing a FOF.[26] Similar findings were found in present study as FOF showed a significant association with depression. FOF can increase the risk of falls through a reduction in social participation and loss of personal contact—which in turn increase isolation and depression.
Of the predictors for FOF among elderly (age above 70 years, educational status as illiterate, history of fall in past 6 months and restriction of daily activities), only educational status and restriction of daily activities are potentially modifiable. Based on these predictors, we can identify individuals at high risk of falling; interventions could be put into place to reduce FOF. This study confirms that FOF is a condition found in Indian elderly and there is a need for interventional studies to prevent and limit the consequences of falls in elderly persons, in particular the development of FOF.
CONCLUSION
FOF has emerged as a multifactorial entity distinct from falls and as an important risk factor for falls among the elderly population living in urban India. It prevails in older adults with and without the history of falls. FOF represents a significant threat to socialization, independence and morbidity or mortality. Assessments of older individuals should include FOF and fall history. Knowledge of risk factors of FOF may be useful in developing multidimensional strategies to decrease it and improve the quality of life of elderly. Some potentially modifiable risk factors associated with FOF have been identified in the present study. Successful management of FOF requires a combined and concerted effort on the part of the treating team. In conclusion, our results will encourage further research on this emerging public health problem in India.
ACKNOWLEDGEMENT
This research paper is from the project selected by the ICMR as STS- 2012 project. All the authors are thankful to ICMR and duly acknowledge their support.
Footnotes
Source of Support: ICMR funded STS-2012 Project
Conflict of Interest: None declared.
REFERENCES
- 1.Age care statistics. [Last cited on 2007 Oct 6]. Available from: http:// www.helpageindia.com .
- 2.van Helden S, Wyers CE, Dagnelie PC, van Dongen MC, Willems G, Brink PR, et al. Risk of falling in patients with a recent fracture. BMC Musculoskelet Disord. 2007;8:55. doi: 10.1186/1471-2474-8-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kumar A, Verma A, Yadav M, Srivastava AK. Fall: The accidental injury in Geriatric Population. J Indian Acad Forensic Med. 2011;33:175–8. [Google Scholar]
- 4.Ganz DA, Bao Y, Shekelle PG, Rubenstein LZ. Will my patient fall? JAMA. 2007;297:77–86. doi: 10.1001/jama.297.1.77. [DOI] [PubMed] [Google Scholar]
- 5.Baker SP, Harvey AH. Fall injuries in the elderly. Clin Geriatr Med. 1985;1:501–12. [PubMed] [Google Scholar]
- 6.Kumar S, Vendhan G, Awasthi S, Tiwari M, Sharma VP. Relationship between fear of falling, balance impairment and functional mobility in community dwelling elderly. Indian J Phys Med Rehabil. 2008;19:48–52. [Google Scholar]
- 7.Mann R, Birks Y, Hall J, Torgerson D, Watt I. Exploring the relationship between fear of falling and neuroticism: A cross-sectional study in community-dwelling women over 70. Age Ageing. 2006;35:143–7. doi: 10.1093/ageing/afj013. [DOI] [PubMed] [Google Scholar]
- 8.Kannus P, Palvanen M, Niemi S, Parkkari J. Alarming rise in the number and incidence of fall-induced cervical spine injuries among older adults. J Gerontol A Biol Sci Med Sci. 2007;62:180–3. doi: 10.1093/gerona/62.2.180. [DOI] [PubMed] [Google Scholar]
- 9.Kempen GI, Yardley L, van Haastregt JC, Zijlstra GA, Beyer N, Hauer K, et al. The Short FES-I: A shortened version of the falls efficacy scale-international to assess fear of falling. Age Ageing. 2008;37:45–50. doi: 10.1093/ageing/afm157. [DOI] [PubMed] [Google Scholar]
- 10.Sebestina AD, Shringarpure A, Karol J. Circumstances and consequences of falls in Indian older adults. Indian J Occup Ther. 2008;40:1–11. [Google Scholar]
- 11.Arfken CL, Lach HW, Birge SJ, Miller JP. The prevalence and correlates of fear of falling in elderly persons living in the community. Am J Public Health. 1994;84:565–70. doi: 10.2105/ajph.84.4.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Howland J, Lachman ME, Peterson EW, Cote J, Kasten L, Jette A. Covariates of fear of falling and associated activity curtailment. Gerontologist. 1998;38:549–55. doi: 10.1093/geront/38.5.549. [DOI] [PubMed] [Google Scholar]
- 13.Tinetti ME, Richman D, Powell L. Falls efficacy as a measure of fear of falling. J Gerontol. 1990;45:P239–43. doi: 10.1093/geronj/45.6.p239. [DOI] [PubMed] [Google Scholar]
- 14.Drozdick LW, Edelstein BA. Correlates of fear of falling in older adults who have experienced a fall. J Clin Geropsychol. 2001;7:1–13. [Google Scholar]
- 15.Vellas BJ, Wayne SJ, Romero LJ, Baumgartner RN, Garry PJ. Fear of falling and restriction of mobility in elderly fallers. Age Ageing. 1997;26:189–93. doi: 10.1093/ageing/26.3.189. [DOI] [PubMed] [Google Scholar]
- 16.Fessel KD, Nevitt MC. Correlates of fear of falling and activity limitation among persons with rheumatoid arthritis. Arthritis Care Res. 1997;10:222–8. doi: 10.1002/art.1790100403. [DOI] [PubMed] [Google Scholar]
- 17.Tinetti ME, Mendes de Leon CF, Doucette JT, Baker DI. Fear of falling and fall-related efficacy in relationship to functioning among community- living elders. J Gerontol. 1994;49:M140–7. doi: 10.1093/geronj/49.3.m140. [DOI] [PubMed] [Google Scholar]
- 18.Delbaere K, Crombez G, Van Den Noortgate N, Willems T, Cambier D. The risk of being fearful or fearless of falls in older people: An empirical validation. Disabil Rehabil. 2006;28:751–6. doi: 10.1080/09638280500304794. [DOI] [PubMed] [Google Scholar]
- 19.Martin FC, Hart D, Spector T, Doyle DV, Harari D. Fear of falling limiting activity in young-old women is associated with reduced functional mobility rather than psychological factors. Age Ageing. 2005;34:281–7. doi: 10.1093/ageing/afi074. [DOI] [PubMed] [Google Scholar]
- 20.Howland J, Peterson EW, Levin WC, Fried L, Pordon D, Bak S. Fear of falling among the community dwelling elderly. J Aging Health. 1993;5:229–43. doi: 10.1177/089826439300500205. [DOI] [PubMed] [Google Scholar]
- 21.Andresen EM, Wolinsky FD, Miller JP, Wilson MM, Malmstrom TK, Miller DK. Cross-sectional and longitudinal risk factors for falls, fear of falling, and falls efficacy in a cohort of middle-aged African Americans. Gerontologist. 2006;46:249–57. doi: 10.1093/geront/46.2.249. [DOI] [PubMed] [Google Scholar]
- 22.Kempen GI, van Haastregt JC, McKee KJ, Delbaere K, Zijlstra GA. Socio-demographic, health related and psychosocial correlates of fear of falling and avoidance of activity in community-living older persons who avoid activity due to fear of falling. BMC Public Health. 2009;9:170. doi: 10.1186/1471-2458-9-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harding S, Gardener A. Fear of falling. Aust J Adv Nurs. 2009;27:94–100. [Google Scholar]
- 24.Bertera EM, Bertera RL. FOF and activity avoidance in a national sample of older adults in the United States. Health Soc Work. 2008;33:54–62. doi: 10.1093/hsw/33.1.54. [DOI] [PubMed] [Google Scholar]
- 25.Murphy S, Tickle-Degnen L. Participation in daily living tasks among older adults with fear of falling. Am J Occup Ther. 2001;55:538–44. doi: 10.5014/ajot.55.5.538. [DOI] [PubMed] [Google Scholar]
- 26.Gagnon N, Flint AJ, Naglie G, Devins GM. Affective correlates of fear of falling in elderly persons. Am J Geriatr Psychiatry. 2005;13:7–14. doi: 10.1176/appi.ajgp.13.1.7. [DOI] [PubMed] [Google Scholar]


