Abstract
Objectives
The level of bone-conducted sound in the auditory meatus is increased at low frequencies by occlusion of the meatus, for example by the earmold of a hearing aid. Physical measures of this “occlusion effect” (OE) require vibration of the skull. In previous research, either self-voicing or audiometric bone-conduction vibrators have been used to produce this vibration, with the result that the OE could not be measured for frequencies below 125 Hz. However, frequencies below this can be important for music perception by hearing aid users. The objective was to develop and evaluate a method that gives a lower-bound estimate of the OE for frequencies below 125 Hz.
Design
A low-noise amplifier with extended low-frequency response was used to record the output of a miniature microphone inserted into the meatus of participants. The signal came from sounds of the heartbeat and blood flow of the participant, transmitted via bone-conduction through the walls of the meatus. A simultaneous recording was made of the carotid pulse to permit time-locked averaging (and hence noise reduction) of the microphone signal. Recordings were made from seven otologically and audiometrically normal participants, using clinical probe tips to produce the occlusion. Recordings were also made from an overlapping group of nine participants, using fast-setting impression material to provide a more consistent degree of occlusion. The difference in level of the recorded signal for unoccluded and occluded conditions provided a lower bound for the magnitude of the OE.
Results
The mean OE increased with decreasing frequency, reaching a plateau of about 40 dB for frequencies below 40 Hz. For some individual recordings, the OE reached 50 dB for frequencies below 20 Hz. With occlusion, the heartbeat became audible for most participants.
Conclusions
The OE can be very large at low frequencies. The use of hearing aids with closed fittings, which may be employed either to prevent acoustic feedback or to allow amplification of low frequencies, may lead to an unacceptable OE. We suggest reducing the OE by the use of a seal deep in the meatus, where the wall of the meatus is more rigid.
Keywords: Occlusion, earmold, hearing aid, bone conduction, heartbeat
INTRODUCTION
Bone conducted-sound can be heard via several paths, one of which involves the transmission of sound into the auditory meatus via vibration of the walls of the meatus. For sounds entering the cochlea via air conduction, the open meatus acts like a highpass filter, with low-frequency sounds being radiated away from the cochlea, out of the meatus (Tonndorf 1972). When the meatus is occluded, for example by a hearing aid earmold or by an earplug, the radiation impedance at the meatal entrance increases, causing an increase in the level of sound generated in the meatus by bone conduction, especially at low frequencies. This increase is called the “occlusion effect” (OE). The smallest OE is observed when the meatus is deeply plugged (von Békésy 1960, p 178). Shallow plugging produces the greatest OE, since the cartilaginous outer part of the wall of the meatus is the primary sound source (Zwislocki 1953; Stenfelt & Reinfeldt 2007). Models of the OE predict an effect in excess of 40 dB at 200 Hz for a very shallow insertion of the occluder (Stenfelt and Reinfeldt, 2007). However, empirical measures, show an OE up to about 30 dB (Killion et al. 1988), but typically much less (Vasil-Dilaj & Cienkowski 2011; Dillon 2012).
The OE is most noticeable with self-generated noises such as heel strikes or self-voicing. The latter has been used to measure the OE (Killion et al. 1988; Vasil-Dilaj & Cienkowski 2011). The lowest frequency at which occlusion can be characterized by this method is determined by the lowest fundamental frequency that the participant can produce, which is typically above 100 Hz for men and 180 Hz for women.
The OE can be characterized by subjective judgments, but these provide little or no information about how the effect varies with frequency. The OE is most easily measured objectively using a vibrating mass, such as an external vibrator, to produce the bone-conducted signal that excites the walls of the meatus. The bone-conduction stimulator used in audiometry has often been used as the source of vibration (Fagelson & Martin 1998; Stenfelt & Reinfeldt 2007; Small & Hu 2011), but this means that the OE cannot be estimated for frequencies below about 125 Hz, due to the design of audiometers. Non-audiometric vibrators have been used to produce vibration at lower frequencies, around 40 Hz, but not to measure the OE (Howell & Williams 1988; Howell et al. 1988). One complication with the use of external vibrators is that the OE depends on the site of stimulation and the direction of applied vibration, whereas body-generated sounds have multiple sites of origin. In order to generate average results, externally applied vibratory sources have commonly been used at multiple sites, such as the mastoid or frontal (forehead) bones (von Békésy 1948; Fagelson & Martin 1998; Stenfelt & Reinfeldt 2007).
Characterization of the occlusion effect is important for the design of systems to deliver amplified low-frequency sound into the meatus. There are at least two situations where this might be desirable. First, measures of audio quality show that, for listening to music, both normal and impaired listeners prefer an extended low-frequency response, including frequencies well below 125 Hz (Franks 1982; Moore & Tan 2003; Füllgrabe et al. 2007; Moore 2012). Hence, it is desirable that, at least for listening to music, hearing aids should amplify low frequencies when the user has a hearing loss at low frequencies, perhaps using a dedicated music program in the hearing aid. Although most current hearing aids have a response that rolls off below 200 Hz, an extended low-frequency response can be obtained, especially when a “closed” fitting is used (Füllgrabe et al. 2007).
The second situation applies to cases of combined electric and acoustic stimulation (EAS), using a cochlear implant together with a hearing aid. Candidates for EAS typically have “corner” audiograms, with some functional acoustic hearing only at low frequencies. Although acoustic stimulation alone typically leads to very poor speech intelligibility for such people, the addition of amplified low-frequency acoustic signals to the electric signals provided by the implant can lead to substantial improvements in intelligibility (Ching et al. 2004; Turner et al. 2004; Kong et al. 2005; Dorman et al. 2008).
The amplification of low frequencies using hearing aids is a challenge because of two factors. First, due to the reduced transmission of sounds through the middle ear at low frequencies (Puria et al. 1997), the sensitivity of normal human hearing decreases with decreasing frequency. Hence, compensation for the effects of a hearing loss requires the use of higher sound pressure levels (SPL) than at middle frequencies. Second, if the transducer is not sealed in the ear canal (for example, if an “open” fitting or large vent is used), most of the sound energy at low frequencies leaks out of the ear canal (Kates 2008), so little amplification is achieved. In practice, a sealed or “closed” fitting is required to produce useful amplification at low frequencies. The requirement for a closed fitting means that the OE may be high, unless deep insertion of the occluding device is achieved (Zwislocki 1953; Killion et al. 1988; Stenfelt & Reinfeldt 2007). Also, closed fittings are sometimes necessary to prevent acoustic feedback, even when low-frequency hearing is essentially normal. Hence, it is desirable to have information about the magnitude of the OE at low frequencies.
A possible novel method for estimating the OE at low frequencies arose during the course of a clinical investigation of “objective” pulsatile tinnitus, where different otometric tips were being used to retain a miniature microphone in the meatus. The signal was mainly derived from the heart beat and blood flow, and its spectrum was dominated by low frequencies. It occurred to us that the heartbeat could be used as a vibration source to characterize the OE over a frequency range where no published data seem to be available, namely from sub-sonic frequencies up to about 200 Hz. This range overlaps with the range where hearing aids with extended low-frequency response may be required to operate. The main purpose of the present study was to measure the magnitude of the OE at low frequencies for various degrees and types of occlusion of the meatus, using sounds generated in the skull by the heartbeat.
METHODS
Equipment
The microphone used for in-meatus recordings was a Knowles FG-23629-C36 (Knowles Electronics, Itasca, Illinois). This is a miniature electret microphone housed in a cylinder, 2.6 mm in diameter and 2.5 mm in length. The manufacturer’s data sheet shows that the response is “flat” between 100 and 4000 Hz. Above 4000 Hz the response rises slowly to +3 dB at 10000 Hz. Our own measurements, reported later, showed that the response was flat for frequencies from 100 down to 10 Hz.
The microphone was connected using a 3-wire configuration (power, signal, ground) with a 1-mm diameter multi-core screened cable. The cable had markers to allow a controlled insertion depth in the meatus. Biocompatibility for skin contact was achieved by encapsulation of the wired device in medical-grade heatshrink sleeving, leaving an opening over the microphone gauze. To prevent potentially damaging ingress of foreign material such as cerumen, this opening was capped by a 2-mm diameter 680-ohm acoustic damper, retained by friction with the heatshrink sleeving. The damper itself comprised a gauze housed in a plastic cylinder. In preparation for insertion in the meatus, the damper was removed, the capsule and cable were cleaned with disinfectant and dried, and a clean damper was inserted.
A second miniature transducer, a vibrometer, was used to record arterial pulsation from a position near the larynx (see below for details), in order to produce a low-noise reference signal of the heart beat. The Knowles BU-27135-000 vibrometer had a size of 8 × 5.5 × 4.1 mm and a response to acceleration that was flat between 100 and 4000 Hz. Its response below 100 Hz was reported by a company representative to be substantially similar to its mid-frequency response. Above 4000 Hz, the response rose, with a resonance peaking above 10000 Hz. The vibrometer was also connected using a 3-wire configuration and sealed in medical-grade heatshrink tubing.
Both transducers were powered from a custom-made battery-powered preamplifier with variable gain. The −3 dB response of the preamplifier was from 0.5 to above 10000 Hz. For the microphone channel, the gain was variable between +13 and +57 dB. For the vibrometer channel, the gain was variable between +40 and +84 dB, and a low-pass filter with a slope of −12 dB/oct and a cut-off frequency of 4700 Hz was applied. The low-pass filter was intended to reduce the level of the vibrometer resonance in the preamplifier output.
The microphone and vibrometer outputs of the preamplifier were recorded on separate channels of an Edirol (Roland Corp., Hamamatsu, Japan) R-44 digital recorder with 24-bit resolution. The low-frequency response from electrical input to digital file had a shallow roll-off; the response was −3 dB at 5 Hz. The sampling rate of 48000 Hz provided an upper frequency limit well in excess of the abilities of the transducers, but was used for simplicity.
All recordings were obtained in a double-brick-walled chamber with a suspended floor. All internal surfaces of the chamber were lined with 10 cm of acoustically absorbing foam.
Microphone Calibration
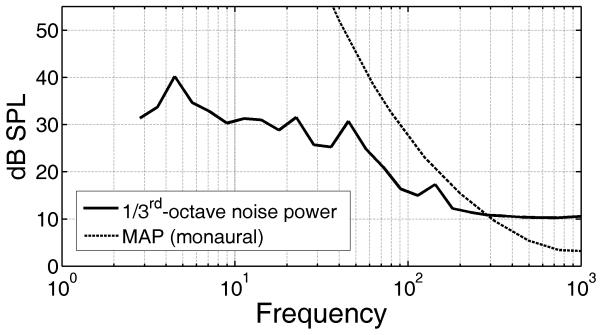
The sensitivity of the microphone was determined by comparing its characteristics to the known calibration of a Bruel & Kjaer Type 4192 microphone in the Zwislocki coupler at the end of the meatus of a KEMAR manikin. The acoustic signal was provided by a Tannoy (Tannoy Ltd., Coatbridge, Scotland) Precision 8D powered loudspeaker reproducing narrowband (< 0.5-octave) low-noise noise bands (LNN, Pumplin 1985) for a range of center frequencies from 10 to 500 Hz. LNN is noise that is synthesized to have very low envelope fluctuations. The LNN property was desirable to achieve low distortion at a level sufficiently high to avoid any influence of background noise, even at very low frequencies, where the loudspeaker output was lower than for mid-range frequencies. Although the preamplifier and R-44 both had variable and stepped controls for adjustment of sensitivity, all recordings were made to digital file with the controls left in a fixed, calibrated position. It was therefore always possible to convert a digital root-mean-square value of the recorded signal back into an equivalent sound pressure level (SPL) at the microphone input. The 680-ohm acoustic damper used with the microphone did not materially alter the microphone response at these relatively low frequencies. The combination of the equivalent input noise of the microphone and room background noise was measured by making recordings with the microphone placed inside a sound-isolated room with no internal sources of sound. The solid line in Figure 1 shows the 1/3rd-octave power levels of the input-referred noise. Total power was equivalent to 44 dB SPL for this recording, but could be as high as 48 dB SPL (unweighted). Although the spectrum of this “noise floor” was consistently flat for frequencies above 200 Hz, in some recordings there were “bumps” at low frequencies related to building (4-5 Hz), occasional indeterminate (~20 Hz) or electrical-mains (~50 Hz and harmonics) noise sources, their level and frequency varying between recordings. The dashed line in Fig. 1 shows the monaural minimum audible pressure (MAP) at the eardrum based on predictions of the loudness model of Moore and Glasberg (2007). Comparison of the two curves indicates that the microphone could reproduce sounds below the threshold of human hearing, for frequencies up to 300 Hz.
Fig. 1.
Equivalent input noise from the microphone and extraneous sounds in the recording room devoid of personnel, expressed as 1/3rd-octave power levels (solid line). The dashed line shows the monaural Minimum Audible Pressure (MAP) for adult humans, estimated using the model of Moore and Glasberg (2007).
Recording technique
Design and use of all equipment and procedures performed on participants had approval from the Cambridgeshire I Research Ethics Committee (NHS) and the NRES Committee East of England (reference 11/H0306/2). Recordings were made from two groups of participants. The first group comprised three female participants (6 ears) and four male participants (7 ears; results for one ear were excluded due to poor recording quality), forming a control group involved in a clinical study of pulsatile tinnitus (PT). It was desired to use eartips that produced significant attenuation of external airborne sounds while avoiding an excessive OE. For this purpose, standard-sized foam or rubber eartips were used for retention of the microphone in the meatus. Due to their non-custom shape, a perfect seal of the tip in the meatus was not always achieved. Although the recordings were sufficiently accurate over the frequency range required for the PT study (200-4000 Hz), great variability was observed in the recorded sound levels at lower frequencies. The insertion of these eartips involved distortion of the eartip shape and resulted in a compression of the meatal walls that varied around the circumference of the eartips. Constriction of the capillaries in the meatal wall could affect the source of the sounds in the meatus. This could lead to errors in the estimated OE because the constriction would not occur with the unoccluded meatus. Since we wished to characterize the OE at very low frequencies, a second set of recordings was made using nine participants fitted with custom eartips made from two-part fast-setting silicone impression material (5 male, 4 female, 12 ears in total; results for six ears were not obtained due to problems in obtaining a good ear impression while not blocking the microphone). Two males and two females had also been employed in experiment 1. Custom eartips were made with the intention of producing stiffer and better-sealed earplugs, but ones that did not apply substantial compression to the walls of the meatus. This was intended to lead to less variable and more valid estimates of the OE. The increase in stiffness was intended to extend the effectiveness of the plugging to ultra low frequencies (< 20 Hz).
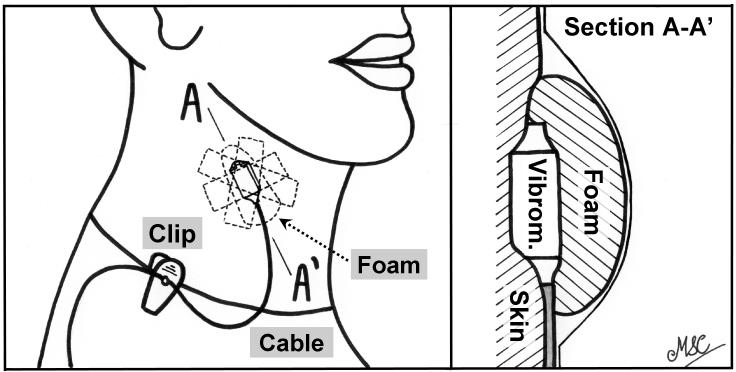
In the work reported here, all participants had normal external ears, as determined by otoscopy, and no history of middle-ear dysfunction. For all recordings, the carotid pulse was identified by finger and a vibrometer was positioned over this site (posterior and slightly superior to the larynx). The method of attachment is shown in the two panels of Figure 2. The vibrometer was secured in place over the carotid artery with Micropor™ tape. After leaving a short loop in the vibrometer cable, the cable was clipped to the participant’s clothing to reduce the transmission of vibration signals generated by movement of the cable. A second layer of tape held a pre-compressed expanding foam earplug over the vibrometer. As the earplug expanded, it provided local pressure of the vibrometer to the skin, improving the sensitivity to vibration. This is shown in more detail in the right-hand panel of Fig. 2, which is a cross-sectional detail along line A-A’ in the left-hand panel. After attachment, the quality of the heartbeat signal picked up by the vibrometer was assessed using an oscilloscope. The signal was required to provide a good representation of the systolic and diastolic phases of the heartbeat cycle, leading to stable triggering of the oscilloscope. If necessary, the vibrometer was re-positioned until a suitable signal was produced. This signal formed the reference signal for timing of the heartbeat cycle.
Fig. 2.
Drawing to show the attachment technique used to obtain a good signal from the vibrometer when placed over the carotid artery (left-hand panel). A cross section along line A-A’ is shown in the right-hand panel. The foam earplug has expanded, and this, combined with tension from the Micropor tape, applied extra pressure between the vibrometer (“Vibrom.”) and the skin.
In the first set of recordings, the tip of the microphone capsule was placed 5-10 mm beyond the entrance of the meatus, as judged using the markers on the cable. It either rested on the meatal wall, effectively giving an open fit, or was retained in a similar position with one of several types of otometric probe tip. For all recordings, the cable was either taped to the skin or clipped to the clothing of the participant to restrict movement of the capsule and reduce the possibility of cable-conducted sound vibrating the capsule. In increasing order of occlusion, the tips were: (1) a conical “rubber” tip as used in paediatric audiology, with entrance diameter of 4 mm and final diameter of 8 mm; (2) a 10-mm or (3) a 13-mm diameter Etymotic Research expanding foam eartip (ER3-14B and −14A, respectively), suitable for an ER3 insert earphone; and (4) a 12-mm diameter “rubber” mushroom tip suitable for a tympanometer. For the foam tips, the semi-rigid plastic tube was removed and the microphone inserted in its place. For the rubber tips, the microphone was inserted to make a good seal in the conical aperture intended for the probe normally used with such a tip. It was possible to use all tips with all ears.
In the second set of recordings, a thinned foam otoblock (as used for taking ear impressions) was inserted into the meatus to a depth of 2-4 mm, and the microphone was inserted until it touched the otoblock. The thinning was performed to reduce acoustic attenuation of meatal signals reaching the microphone: the otoblock produced < 0.1 dB reduction in level for frequencies in the region of interest (4-200 Hz). The meatus was then back-filled with a two-part fast-setting silicone impression material, as done when taking an impression for an earmold. After the material had set, the occluded-meatus recording was made. Lack of disturbance of the set material ensured a good seal of the meatus, reducing the possibility of slit leaks. The open-meatus recording was made either before making the impression or after removing the impression. The microphone was inserted to a similar depth in the meatus as used for the closed-meatus recording.
The participant was seated on a fabric-covered foam-padded chair, in an upright, relaxed posture, instructed to breathe through an unconstricted nose and mouth, and requested not to move during the recording period. The room lighting was produced by low-noise, high-frequency fluorescent tubes and so was not expected to produce noise in the frequency range of interest. Except for the ventilation, all noise-producing equipment was switched off or removed from the chamber for the first set of recordings. For the second set of recordings, involving the custom earmolds, the ventilation fans were switched off during each recording. All recordings were made for a minimum duration of 30 s.
ANALYSIS AND RESULTS
Recordings were transferred to a PC for off-line analysis. All processing involved custom software written in MATLAB™. The vibrometer signal was used to provide timing pulses from the start of the systolic phase of the heartbeat; once identified, short segments of the microphone signal were extracted for averaging. This time-synchronous averaging had the effect of improving the ratio of the signal generated via vibration of the meatal wall (which stayed approximately constant from one heartbeat to the next) relative to the background noise (which varied across heartbeats). Artifactual noise was present in both recording channels from many sources, such as infrasonic building vibration, participant movement and experimenter movement. This was removed or reduced from the recordings by the software, to produce a low-noise waveform synchronized with the heartbeat period. If either signal in each recording was identified as containing even short segments of noise higher than the long-term level of the periodic component of each signal, the microphone signal for that particular “beat” was discarded from further processing. Additionally, after every event identified as “high level”, the preceding 0.25 s and following 0.5 s were identified as unsuitable for averaging. This was done to ensure that build ups to, or decays from, a noise event were not included in the averaging. For open-meatus recordings, the net effect of these processes of rejection meant that averages were sometimes based on as few as 10 heartbeats. For closed-meatus recordings, averages were typically based on about 25 heartbeats.
After finding the trigger points for each heartbeat, the mean beat period was calculated over the duration of each recording. Inspection of the power spectral density (psd) of the averaged signals showed that most acoustic power occurred at frequencies below about 30 Hz. Additionally, there was often a strong component related to electrical-mains interference. To reduce the influence of this mains interference on the estimate of the overall signal level and of the overall OE, the entire microphone recording was lowpass filtered using an 8th-order elliptic filter with a cut-off frequency of 28 Hz and a stopband response < −90 dB. The filter response was −4 dB at 30 Hz, and < −80 dB for frequencies exceeding 50 Hz: this removed the interference at 50 Hz and above from the data, while preserving the frequency range where most of the acoustic power fell. The low-pass filtered microphone signal was then used to generate an average heartbeat-period-synchronous waveform using the method described above, again discarding any previously identified “noisy” periods. The total power was calculated in a window extending from −0.2 to +0.5 periods around the trigger point, to measure power primarily during the active part of the heartbeat cycle.
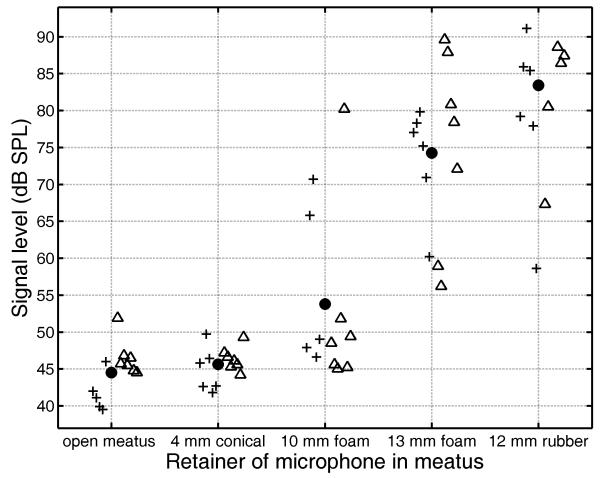
Figure 3 shows the total sub-28 Hz power measured for each eartip used in the first set of recordings. Grand means for each eartip are shown as solid circles. Individual results are shown by crosses to the left of the abscissa marker for female ears, and by open triangles to the right of the abscissa marker for male ears. Results for the 4-mm conical tip were similar to those for the open meatus, indicating minimal or no OE. For the 10-mm foam tip, for most ears the levels were only a little above those recorded in the open meatus. However, for one male and two female ears, there was a substantial increase, indicating an OE. For the 13-mm foam and 12-mm rubber tips, an OE was obtained for all ears, ranging from moderate (12-15 dB) to very large (about 40 dB). The clustering of results between 40 and 50 dB SPL for the open meatus and 4-mm conical tip reflects the noise floor of the microphone recording system. From the calibration recordings, the similarly low-pass filtered (but non-averaged) signal had a total power between 44 and 48 dB SPL. The range reflected the varying structure-borne noise such as door slams in other parts of the building. Since this noise was uncorrelated with the heartbeat, the averaging process reduced its influence on the levels reported in Fig. 3.
Fig. 3.
Results from the first group of participants, showing total power levels for heartbeat-synchronous waveforms for frequencies up to 28 Hz, for each eartip used to retain the microphone in the meatus. For each tip, results for female ears are shown by crosses to the left of the abscissa marker and results for male ears are shown by open triangles to the right of the abscissa marker. Grand means are shown by filled circles.
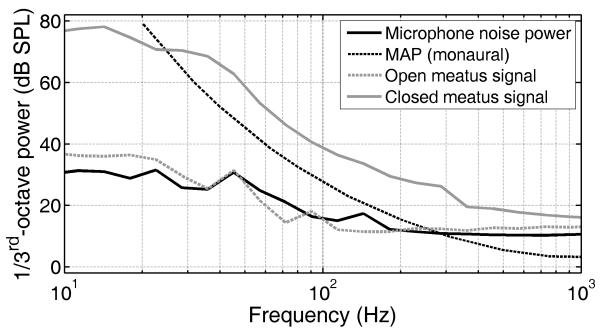
The MAP at 20 Hz is 79 dB SPL (Moore & Glasberg 2007). A mean level of 84 dB SPL for frequencies below 28 Hz was measured in the meatus when it was occluded by the 12-mm rubber tip. Unsurprisingly therefore, the majority of participants reported hearing their own heartbeat when this tip was used. The dark solid line in Figure 4 shows the electrical noise floor from the microphone and the human, repeated from Fig. 1. The dashed and solid grey lines show the 1/3rd-octave signal power for an example pair of open and closed meatus recordings, respectively. The OE increased the signal power so that, between 30 and 300 Hz in the closed-meatus recording, the 1/3rd-octave signal power was above the MAP and would have been audible.
Fig. 4.
1/3rd-octave power levels from an example pair of open meatus (dashed grey line) and closed meatus (solid grey line) recordings when using a highly occluding earplug. The black line shows the microphone electrical noise and the dark dashed line shows MAP. The levels from the closed-meatus signal exceed the MAP for all frequencies above 25 Hz.
To obtain a frequency-dependent measure of the OE, the power spectral density (psd) was calculated for 512-ms-duration segments of the averaged waveform. Each segment was Kaiser-windowed with a β-parameter of 7.6 (Rabiner & Gold 1975, p33ff) to improve sidelobe rejection. Each segment overlapped by 75% with the next segment. Combined with the segment duration, this window ensured that less weighting was given to the very start and end of the average period, so that the psd was based mainly on times when the energy was highest. Less weight would therefore be placed on continuous external noises or noises occurring asynchronously with the heartbeat. The psd was smoothed by grouping frequency bins into 1/3rd-octave bands. The difference between a given 1/3rd-octave level with the meatus open and occluded represents the OE at the center frequency of that band. Since the recordings were influenced to some extent by external extraneous sounds, and since the level of those sounds in the meatus would have been greater for the open than for the occluded meatus, the OE estimated in this way represents a lower bound of the OE, denoted here OE’; the true OE could be larger.
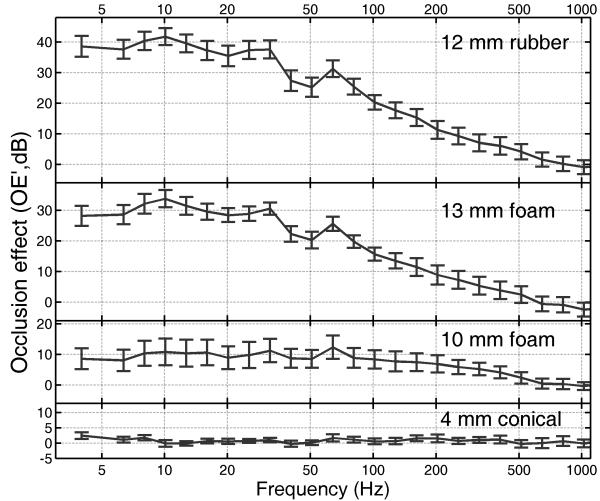
The four panels of Figure 5 show the mean OE’ for each eartip used, plotted as a function of center frequency. Unsurprisingly, the conical tip led to near-zero OE’ across all frequencies (bottom panel). For all tips, OE’ was near zero for frequencies greater than 600 Hz. However, this may reflect the fact that the heartbeat signal recorded in the meatus had little energy for frequencies above about 500 Hz, which probably led to OE’ being much smaller than the true OE at those frequencies. Figure 5 in Stenfelt and Reinfeldt (2007) shows a modeled OE of about 18-22 dB at 600 Hz, for occluder insertion depths between 10 and 5 mm. Even at 200 Hz, Stenfelt and Reinfeldt (2007) show a modeled OE of about 34-38 dB for the insertion depths of 5-10 mm, compared to 12 dB for OE’ reported here. Hence, it is likely that even at 200 Hz, the meatal signal did not have enough energy to give reliable estimates of the OE.
Fig. 5.
OE’ estimates calculated as the ratio between the 1/3rd-octave power recorded in the meatus with the meatus open and with it occluded with a non-custom eartip. Error bars denote ±1 standard error.
For frequencies of 100 Hz or below, the meatal signal probably did have sufficient energy for OE’ to approach the true OE. Fig. 5 shows that, especially for the 13-mm foam and 12-mm rubber tips, OE’ was consistently high for frequencies below 100 Hz. The “dip” in OE’ between 40 and 50 Hz results from artifacts, such as externally sourced ventilation and electrical-mains noise, whose level in the meatus was higher for the open-meatus recordings than for the occluded-meatus recordings. This prompted the extra precautions taken in the second set of recordings, such as the temporary turning off of ventilation during recordings.
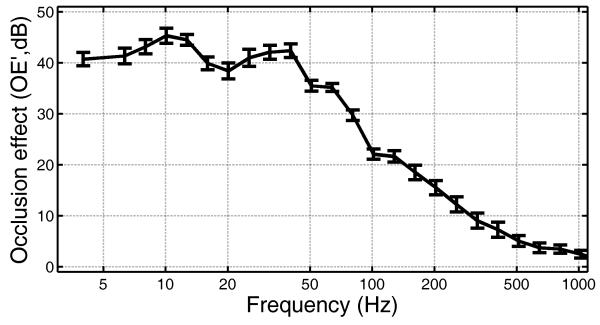
Figure 6 shows the OE’ estimated using the data obtained with the custom ear impressions. For most frequencies between 4 and 1000 Hz, the OE’ was about 2-3 dB higher than obtained for the 12-mm rubber tip (top panel of Fig. 5). Again, there is evidence for electric mains-related noise centered on 50 and 100 Hz, as well as occasional 20-Hz building-related noise contributing to dips in OE’ around these frequencies. Nevertheless, it is clear that the OE can be substantial for frequencies below 100 Hz.
Fig. 6.
As Fig. 4, but showing OE’ estimates obtained using the custom eartips.
DISCUSSION
The method described here leads to a lower bound of the magnitude of the OE. The values of OE’ probably underestimate the true OE because the results are influenced by extraneous sounds, whose level decreases when the meatus is occluded (Hansen & Stinson 1998). The accuracy of the estimates of the OE could be improved by reducing the effects of extraneous sounds. This could be achieved by sealing closed acoustically damped containers against the side of the head, such as cylindrical tubes (von Békésy 1949; Pörschmann 2000), boxes (Hansen & Stinson 1998) or both (Watson & Gales 1943). These containers have to be large enough so that, on their own, they produce negligible occlusion. This requires large volumes (several liters for a frequency of 128 Hz), which would make such procedures cumbersome and inconvenient in clinical practice.
Our method assumes that, due to the multiplicity of arrival paths, no (major) changes of sound level in the meatus occurred in either open or closed-meatus recordings due to constructive or destructive interference of the bone-conducted sound radiated into the meatus via vibrations of its wall and air-conducted sound leaking into the meatus. This assumption seems reasonable for two reasons. First, the level of airborne sound produced by the heart beat and blood flow is very low and generated remotely from the recording point. Second, the pulse wave velocity in arteries, 4-10 m/s (Bramwell & Hill 1922), is much slower than the speed of sound in air or solids. Consequently, heartbeat and blood flow sounds in the meatus are essentially decorrelated for air-conducted and bone-conducted sound.
Our results show that complete occlusion of the meatus using a rubber plug (top panel of Fig. 5) or a custom ear impression (Fig. 6) leads to an OE of at least 40 dB at low frequencies (below about 40 Hz) and at least 20 dB at 100 Hz. Hence, the OE at low frequencies can be very substantial when a closed fitting is used.
We pointed out in the introduction that an extended low-frequency response is required for music to be perceived as high in quality for both normal-hearing and hearing-impaired listeners. For a hearing-impaired person with near-normal hearing at low frequencies and a hearing loss that is not too severe at high frequencies, an open fitting (non-occluded meatus) will allow the low frequencies to be heard naturally. However, if high gain is required at any frequency, an open fitting may lead to problems with acoustic feedback, even if digital feedback cancellation is activated. In such cases it may be necessary to use a closed fitting. Our results show that this can lead to a substantial OE at low frequencies, possibly producing adverse effects such as the user hearing their own heartbeat or being disturbed by the sound of their own footsteps. Such effects would be especially noticeable for people with near-normal hearing at low frequencies, but they might occur to some extent even for people with mild hearing loss at low frequencies. A possible solution for people with normal or mild hearing loss at low frequencies is to use a dome or earmold that fits deeply in the meatus where the wall is boney and there is less transmission of bone-conducted sound into the meatus (Zwislocki 1953; Killion et al. 1988).
CONCLUSIONS
A new method for estimating a lower bound for the occlusion effect (OE) at low frequencies has been developed. This method uses the energy from the heart beat to provide an excitatory source to generate the bone-conducted sounds that reach the meatus. Averaging synchronous with the heartbeat signal (picked up by a vibrometer placed on the neck) and several other procedures were used to reduce the effects of extraneous noise. The results show that the magnitude of the OE at low frequencies increases with increasing degree of occlusion, as expected. For some occluders, the magnitude of the OE varied markedly across participants. For rubber plug or custom-fitted occluders, the OE magnitude was 40 dB or more at very low frequencies (40 Hz and below), and exceeded 20 dB at 100 Hz.
As a result of the OE, many body-generated sounds, such as heartbeats, became clearly audible to participants with normal hearing. If a closed-fitting hearing aid is used for a person with normal hearing or mild hearing loss at low frequencies, for example to prevent acoustic feedback or to allow amplification of low-frequency sounds, the OE could be very disturbing. To reduce the effects of the OE, the seal should be made deep in the meatus.
ACKNOWLEDGMENTS
This work was supported by two UK-based organizations: (1) the Medical Research Council (grant number G0701870, authors MAS and BCJM) and (2) the National Health Service (authors AMP and PA). We thank Marina Salorio-Corbetto for assistance with the custom impressions and for producing the illustrations in Fig. 2.
Source of Funding:
This work received funding from the UK Medical Research Council (grant number G0701870, MAS and BCJM) and the UK National Health Service (AMP and PA).
Footnotes
Conflicts of Interest None declared for any author.
REFERENCES
- Bramwell JC, Hill AV. The velocity of the pulse wave in man. Phil Trans R Soc B. 1922;93:298–306. [Google Scholar]
- Ching TY, Incerti P, Hill M. Binaural benefits for adults who use hearing aids and cochlear implants in opposite ears. Ear Hear. 2004;25:9–21. doi: 10.1097/01.AUD.0000111261.84611.C8. [DOI] [PubMed] [Google Scholar]
- Dillon H. Hearing Aids. 2nd Ed. Boomerang Press; Turramurra, Australia: 2012. [Google Scholar]
- Dorman MF, Gifford RH, Spahr AJ, et al. The benefits of combining acoustic and electric stimulation for the recognition of speech, voice and melodies. Audiol Neurotol. 2008;13:105–112. doi: 10.1159/000111782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagelson MA, Martin FN. The occlusion effect and ear canal sound pressure level. J Am Acad Audiol. 1998;7:50–54. doi: 10.1044/1059-0889(1998/010). [DOI] [PubMed] [Google Scholar]
- Franks JR. Judgments of hearing aid processed music. Ear Hear. 1982;3:18–23. doi: 10.1097/00003446-198201000-00004. [DOI] [PubMed] [Google Scholar]
- Füllgrabe C, Moore BCJ, van Tasell DJ, et al. Effects of bandwidth on sound-quality preferences for hearing aids. Bulletin of the American Auditory Society. 2007;32:45. [Google Scholar]
- Hansen MØ, Stinson MR. Air conducted and body conducted sound produced by own voice. Canad Acoust. 1998;26:11–19. [Google Scholar]
- Howell P, Williams M. The contribution of the excitatory source to the perception of neutral vowels in stuttered speech. J Acoust Soc Am. 1988;84:80–89. doi: 10.1121/1.396877. [DOI] [PubMed] [Google Scholar]
- Howell P, Williams M, Dix H. Assessment of sound in the ear canal caused by movement of the jaw relative to the skull. Scand Audiol. 1988;17:93–98. doi: 10.3109/01050398809070697. [DOI] [PubMed] [Google Scholar]
- Kates JM. Digital Hearing Aids. Plural; San Diego: 2008. [Google Scholar]
- Killion MC, Wilber LA, Gudmundsen GI. Zwislocki was right: A potential solution to the “hollow voice” problem (the amplified occlusion effect) with deeply sealed earmolds. Hear Inst. 1988;39:14–18. [Google Scholar]
- Kong YY, Stickney GS, Zeng FG. Speech and melody recognition in binaurally combined acoustic and electric hearing. J Acoust Soc Am. 2005;117:1351–1361. doi: 10.1121/1.1857526. [DOI] [PubMed] [Google Scholar]
- Moore BCJ. Effects of bandwidth, compression speed, and gain at high frequencies on preferences for amplified music. Trends Amplif. 2012;16:159–172. doi: 10.1177/1084713812465494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore BCJ, Glasberg BR. Modeling binaural loudness. J Acoust Soc Am. 2007;121:1604–1612. doi: 10.1121/1.2431331. [DOI] [PubMed] [Google Scholar]
- Moore BCJ, Tan CT. Perceived naturalness of spectrally distorted speech and music. J Acoust Soc Am. 2003;114:408–419. doi: 10.1121/1.1577552. [DOI] [PubMed] [Google Scholar]
- Pörschmann C. Influences of bone conduction and air conduction on the sound of one’s own voice. Acta Acust - Acust. 2000;86:1038–1045. [Google Scholar]
- Pumplin J. Low-noise noise. J Acoust Soc Am. 1985;78:100–104. [Google Scholar]
- Puria S, Rosowski JJ, Peake WT. Sound-pressure measurements in the cochlear vestibule of human-cadaver ears. J Acoust Soc Am. 1997;101:2754–2770. doi: 10.1121/1.418563. [DOI] [PubMed] [Google Scholar]
- Rabiner LR, Gold B. Theory and Application of Digital Signal Processing. Prentice-Hall; New Jersey: 1975. [Google Scholar]
- Small SA, Hu N. Maturation of the occlusion effect: a bone conduction auditory steady state response study in infants and adults with normal hearing. Ear Hear. 2011;32:708–719. doi: 10.1097/AUD.0b013e31821de1b0. [DOI] [PubMed] [Google Scholar]
- Stenfelt S, Reinfeldt S. A model of the occlusion effect with bone-conducted stimulation. Int J Audiol. 2007;46:595–608. doi: 10.1080/14992020701545880. [DOI] [PubMed] [Google Scholar]
- Tonndorf J. Bone conduction. In: Tobias JV, editor. Foundations of Modern Auditory Theory. II. Academic; New York: 1972. pp. 203–254. [Google Scholar]
- Turner CW, Gantz BJ, Vidal C, et al. Speech recognition in noise for cochlear implant listeners: benefits of residual acoustic hearing. J Acoust Soc Am. 2004;115:1729–1735. doi: 10.1121/1.1687425. [DOI] [PubMed] [Google Scholar]
- Vasil-Dilaj KA, Cienkowski KM. The influence of receiver size on magnitude of acoustic and perceived measures of occlusion. Am J Audiol. 2011;20:61–68. doi: 10.1044/1059-0889(2010/09-0031). [DOI] [PubMed] [Google Scholar]
- von Békésy G. Vibration of the head in a sound field and its role in hearing by bone conduction. J Acoust Soc Am. 1948;20:749–760. [Google Scholar]
- von Békésy G. The structure of the middle ear and the hearing of one’s own voice by bone conduction. J Acoust Soc Am. 1949;21:217–232. [Google Scholar]
- von Békésy G. In: Experiments in Hearing. Wever EG, translator. McGraw-Hill; New York: 1960. [Google Scholar]
- Watson NA, Gales RS. Bone conduction threshold measurements: Effects of occlusion, enclosures, and masking devices. J Acoust Soc Am. 1943;14:207–215. [Google Scholar]
- Zwislocki J. Acoustic attenuation between the ears. J Acoust Soc Am. 1953;25:752–759. [Google Scholar]