Abstract
Objective:
To document the 6-month prevalence of posttraumatic stress syndrome (PTSS) in the older adult population and the validity of a PTSS Scale in an epidemiologic setting.
Method:
Data came from the Enquête sur la santé des aînés et l’utilisation des services de santé (ESA Services Study) conducted during 2012–2013 using a probability sample of older adults seeking medical services in primary health clinics.
Results:
Results showed that a first-order PTSS measurement model consisting of 3 indicators—the number of lifetime traumatic events, the frequency of reactions and symptoms of distress associated with the traumatic events, and the presence of consequences on the social functioning—was plausible. Reliability of the PTSS was 0.82. According to the PTSS, 11.1% of the older adult patients presented with PTSS, but only 21.7% of them reported an impact of their symptoms on their social functioning. The prevalence of older adults meeting the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, criteria for full posttraumatic stress disorder (PTSD) reached 1.8%, and 1.8% of older adults reached criteria for partial PTSD. Our results also showed that women were more at risk to report PTSS than men and that older adults aged 75 years and older were less likely to report these symptoms than those aged between 65 and 74 years.
Conclusions:
PTSS is a common mental health problem among adults aged 65 and older and seeking health services in the general medical sector.
Keywords: posttraumatic stress disorder, mental health, aging, epidemiology, primary care
Abstract
Objectif :
Documenter la validité et la fiabilité du SSPT et la prévalence du syndrome de stress post-traumatique dans la population âgée de 65 ans et plus.
Méthode :
Les données de cette étude proviennent l’étude ESA-services menée en 2012–2013 auprès d’un échantillon probabiliste de personnes âgées de 65 ans et plus en attente de services médicaux dans des cliniques de santé primaires.
Résultats :
Nos résultats ont montré qu’un modèle de mesure du syndrome de stress post-traumatiques (SSPT) composé de trois indicateurs: le nombre d’événements traumatisants au cours de la vie, la fréquence des réactions et symptômes de détresse associée à des événements traumatiques et la présence des conséquences sur le fonctionnement social, était plausible. La fiabilité du SSPT était de 0,82. Selon nos résultats, 1,8 % des patients âgés rencontrait les critères du DSM-IV du trouble de stress post-traumatique durant les 6 derniers mois précédant leur visite médicale et 1,8% rencontrait les critères d’un trouble partiel. Nos résultats ont également montré que les femmes étaient plus à risque de présenter des SSPT que les hommes et que les personnes âgées de 75 ans et plus étaient moins susceptibles de rapporter ces symptômes que ceux âgés de 65 à 74 ans.
Conclusions :
SSPT est un problème de santé mentale fréquent chez les personnes âgées de 65 ans et plus recherchant des services dans le secteur de la médecine générale.
Posttraumatic stress disorder is a condition that follows exposure to an extremely traumatic event related to death, a serious injury, or violence. To be diagnosed with PTSD, according to DSM-IV criteria, a person has to experience at least 1 symptom of intrusion, 3 symptoms of avoidance, and 2 symptoms of hyperarousal for at least 4 weeks and areas of social functioning must be affected substantially. PTSD is considered acute if the symptoms last less than 3 months and chronic if symptoms last 3 months or more. Finally, PTSD is considered as delayed onset if the symptoms occur at least 6 months after the trauma.1 In nonclinical epidemiologic settings, several questionnaires have been developed to help assess PTSD, such as the IES-R,2 the PTSD Checklist,3 the Davidson Trauma Scale,4 the Mississippi PTSD Scale—Civilian Version,5 and the Posttraumatic Diagnostic Scale.6 These screening tools consist of a set of signs that characterize PTSS but do not include all DSM-IV criteria for PTSD.7 Results from these scales must therefore differentiate from results obtained from DSM-IV measures (PTSD).
PTSD in the past was mainly limited to war situations, but has recently been recognized and extended to other circumstances, such as natural disasters, terrorist attacks, hostage situations, assault, and rape.8 The lifetime prevalence of PTSD in older adults has ranged between 2.5% and 3.9%.9 The 1-month prevalence in the older adult population has been estimated between 1.5% and 1.7%,10,11 while the 12-month prevalence has reached 2.1%.12 In populations at risk of experience-specific traumas, the prevalence of PTSD may be higher. In a sample of older adults who survived Hurricane Ike in 2008, the 1-month prevalence of PTSD was 7.6%.13 A prevalence of 22.6% was reported in an elderly sample from China 3 years following the 2008 Wenchuan earthquake.14
Clinical Implications
For the first time, our study provides data on the prevalence of PTSS in the older adult population in Quebec.
PTSS is highly prevalent in the older adult population consulting in the general medical sector.
Our study showed the important impact of PTSS on the functioning of older adults.
Limitations
We used self-reported information from respondents.
Validity of the PTSS regarding clinical PTSD diagnosis may be limited.
Our sample is limited to the Quebec population.
Others studies,15,16 assessing the prevalence of PTSS in the general population, have shown 6-month estimates reaching 13.1%. Based on the National Survey of Women Veterans, the prevalence of PTSS among women veterans reached 13%.17
The most often reported risk factors of PTSS in community samples have included female sex,18–20 low income,17,20,21 and being unmarried.18,20,22 Regarding age, some studies have found an association between younger age,17,23 while others have seen an association with older age.24,25 PTSS has also been associated with physical health problems in older adults26 and with an increased use of health care services.17,27
Among the questionnaires developed to assess PTSS, the IES2 is the most largely used.28 The IES was revised in 1997 to be more representative of the PTSD criteria found in the DSM-IV.29,30 A review of 4 studies with diverse trauma experiences suggested a total score of 24 to 25 out of 88 as a cut-off point for the IES-R.31 The internal consistency reliability coefficient for the IES-R ranged from 0.92 to 0.96 for the 4 subscales, respectively.31–33 The IES-R had a correlation of 0.39 to 0.66 with the CAPS.33,34 A study conducted by Beck et al,33 using discriminant function analysis to assess the IES-R subscales in identifying people with and without PTSD, as compared with the CAPS, reported a sensitivity of 74.5% and a specificity of 63.1% for the IES-R.
A potential limit of the IES-R resides in the absence of a weight given to the number of traumatic events experienced by the respondent and in the absence of assessment of the severity of the symptoms reported (Criterion F). In addition, the information on the psychometric properties of the IES-R among community-dwelling older adults is limited.35
Therefore, the objective of our study was to document the internal consistency and construct validity of a PTSS Scale based on the IES-R index but including information on the number of traumatic events, as well on symptom severity in a population aged 65 years and older. Our objective was also to document the 6-month prevalence of PTSS in the older adult population.
Conceptual Framework
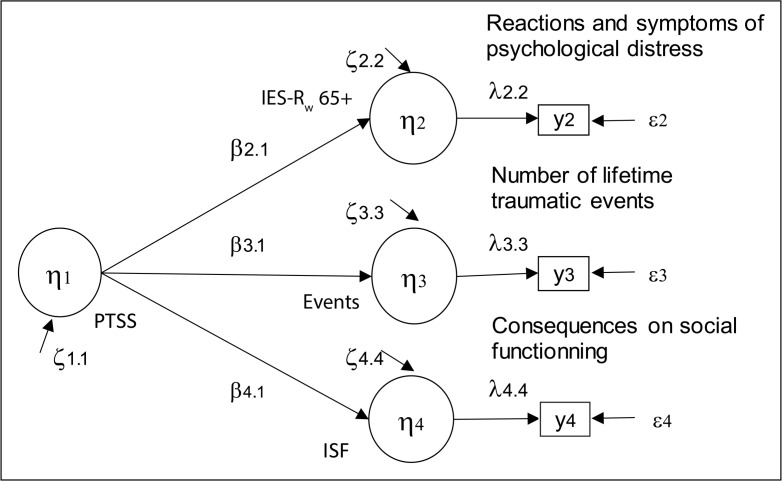
In our study, our hypothesis is that the syndrome of PTSS is a latent, continuous variable measured by 3 indicators: the number of traumatic events in the lifetime, the frequency in the past 6 months of reactions and symptoms of distress associated with the exposure of a traumatic event, and the number of consequences on the social functionality of people who report a traumatic event. Based on this hypothesis, we expect a significant association between the 3 indicators and the latent construct of PTSS in the older adult population. The proposed measurement model can be described using the following structural equations:
These equations are presented in Figure 1, where the 3 indicators of PTSS (yi) (i = 2, 3, 4) are observed variables and where (yi) (i = 3, 4) are considered to be measured without error, as their reliability is unknown. The coefficients of validity of the indicators of PTSS (λi,j [i = 3, 4]) and the error (εi) terms were therefore set to 1 and 0, respectively. Betas (βj,j) are regression coefficients between indicators of PTSS (ηj [j = 2, 3, 4]) and the latent variable (ηj [j = 1]) representing PTSS. Zetas (ζj) (j = 2, 3, 4) represent the variance of the PTSS indicators explained by external causes not measured in the study.
Figure 1.
Measurement model of PTSS among older adults
IES-Rw = Impact of Event Scale—Revised; ISF = impairment in social functioning; PTSS = posttraumatic stress syndrome
Method
Data used in our study came from a cross-sectional survey, the ESA Services Study, conducted during 2011–2013 using a probabilistic sample of older adults aged 65 years and older waiting for medical services in primary health clinics in one of the health regions of Quebec. The health and social services agency taking part in our study is responsible for a population of 1 325 000 inhabitants.
A sample of GPs working full time in the health region was constituted. The sampling plan of the study included stratification according to 4 types of primary medical health services organizations: the family medicine group, local community health services centres, PCs with less than 3 GPs, and PCs with at least 3 GPs. On a list of 744 eligible GPs, 409 agreed to participate in our study, among whom 245 GPs effectively recruited patients (an average of 7.3 voluntary patients per GP).
Data were weighted to ensure that the true proportions of older adult patients in each type of primary medical health services organization were reflected in the analysis. Weight (w) given to each subject represents the inverse of their probability of participation. The mean sampling design effect was 1.004.
Procedure
Patients aged 65 years and older who visited 1 of the participating GPs during the study period received, in the waiting room, a pamphlet describing the objectives and the length of the study and inviting them to participate in a face-to-face interview at home. The volunteers had to leave a phone number where they could be reached and had to complete the K10, a short screening questionnaire about depression36 prior to the consultation with their doctor who was not aware of the patient’s results on the K10. Patients were subsequently reached by phone within 30 days to confirm their continuing interest in participating in an interview at home and to book an appointment. A compensation of $15 was provided to the participants to ensure a sufficient participation rate. This project received approval from the Ethics Committee of the Charles LeMoyne Hospital. In total, 1811 patients agreed to participate in the at-home interview.
The interviewers were health professionals (n = 19). In preparation for the interviews, they received 1 day of training on the administration of the computerized ESA questionnaire. At the beginning of the interview, lasting on average 90 minutes, a written consent was obtained from the respondents to carry out the interview. As memory problems affect the accuracy of the information given and the performance of the questionnaires, patients with a moderate or severe cognitive problem, based on the Mini-Mental State Examination (<22) (n = 46), were excluded at the beginning of the interview. Then, patients without cognitive problems were invited to answer the ESA questionnaire. To avoid desirability and information bias associated with the presence of another family member or friend, the interviews were conducted in the most isolated area of the house.
Measures
The number of lifetime potentially traumatic events was measured using a list of 14 potentially traumatic events, comparable with those suggested in the DSM-IV (online eAppendix A). A continuous variable ranging from 0 to 14 lifetime potentially traumatic events was constructed.
The presence of reactions and symptoms associated with the traumatic events was measured using an adaptation of the IES-R.37 The scale used in the ESA research program included the 22 symptoms of the IES-R judged by the respondent in reference to the most important traumatic event reported in terms of frequency of occurrence during the last 6 months on a Likert scale ranging from 0 to 3 (not at all too often). The score of the IES-R varied from 0 to 66 (online eAppendix A).
Severity of reactions and symptoms reported was determined based on the presence of impact on social functioning in the following 4 areas in the last 6 months: personal self-care (for example, dressing, eating, and taking medicines), the ability to communicate (for example, see, speak, and hear), the ability to move indoors or outdoors (for example, to walk, to use a car, taxicab, or bus); domestic tasks, including preparing meals, grocery shopping, maintaining a home, laundry, and managing personal finances; social activities, including participating in elderly associations or clubs, bingo, and dancing; and relationships with others, including family members, friends, and neighbours. The impact of reactions and symptoms in social functioning was measured using a Likert scale varying from 0 to 4 (not at all to extremely). A variable (ISF) ranging from 0 to 16 was created using the sum of the impact ratings.
The criterion validity of the PTSS was assessed using a measure of probable full and partial PTSD determined based on the following DSM-IV criteria. Subjects who reported at least 1 intrusion symptom, 3 avoidance symptoms, 2 arousal symptoms, and the presence of impairment in their social functioning during the 6-month period preceding their interview were considered having full PTSD. When at least 1 symptom from each of the 3 clusters was endorsed for the last 6 months, with or without the presence of impairment in their social functioning in the last 6 months, the respondents were considered to have partial PTSD according to the National Epidemiologic Survey on Alcohol and Related Conditions methodology.38
Analyses
First, missing data on the variables studied were replaced by estimates calculated based on responses given by respondents having a similar response profile using the maximum likelihood method implemented in PRELIS, a LISREL utility program.39 The final sample included 1765 older adults having completed information on all variables. Then, the construct validity of the PTSS was tested using LISREL 8.80 version.39 As the variables were not normally distributed, the polychoric correlations matrix and the variance and covariance asymptotic matrix were used to estimate the hypothetical model’s parameters (Figure 1). The chi-square maximum likelihood robust statistic and the RMSEA index were used to guide the overall assessment of the models. We also used the chi-square and degrees of freedom ratio proposed by Wheaton et al.40 The chi-square and degrees of freedom ratio indicates how many times the observed value is greater than its expected value. A ratio of less than 3 indicates a satisfactory fit.41 The RMSEA assesses the error of approximation of the model in the population. It varies from 0 to 1. A value lower than 0.05 indicates a close fit to the data. A 95% statistical significance threshold was used for our analyses.41 The H statistic was used to document the internal consistency reliability coefficient of the scale. This measure indicates the average total variance of the items taken into account by the latent construct.42
The ROC analysis was used to test the criterion validity of the PTSS. This methodology is used to describe the relation between the proportions of false positives (1: specificity) to a test and sensitivity (proportion of true positives) for different thresholds of positivity. The AUC and the dʹ delectability index were used to guide the choice of the optimal positivity threshold of the PTSS.43,44 The AUC index reflects the probability that 2 people randomly drawn from each of the 2 groups (PTSD patients and non-PTSD patients) be classified correctly. A value between 0.50 and 0.70 is indicative of low precision, a value between 0.70 and 0.90 indicates good precision, and a value over 0.90 indicates excellent precision.
The PTSS was compared with the probable PTSD (full and partial) measure in terms of sensitivity, specificity, as well as correct classification rates. The Connell and Koepsell ratio (%C+)45 was also calculated to assess the gain in certainty.
Results
The study sample included 57.3% women, and 62.5% of the respondents were between 65 and 74 years. The mean age of the respondents was 73.2 years (SD 6.1). These characteristics are similar to those observed in the population of Quebec46,47 (Table 1).
Table 1.
Respondents’ characteristics
| Characteristic | Sample, n = 1765
|
|
|---|---|---|
| n | % | |
| Sex | ||
| Women | 1011 | 57.3 |
| Men | 754 | 42.7 |
| Age, years | ||
| 65–74 | 1103 | 62.5 |
| ≥75 | 662 | 37.5 |
| Posttraumatic stress disorder | ||
| None | 1698 | 96.2 |
| Full | 31 | 1.8 |
| Partial | 32 | 1.8 |
|
| ||
| Mean | SD | |
|
| ||
| Total score of the PTSS (0–60)a | 7.5 | 9.6 |
| Score on the IES-R (0–62)a | 8.0 | 11.8 |
| Number of traumatic events (1–14)a | 2.3 | 1.5 |
| Impact score on social functioning (0–16)a | 0.45 | 1.6 |
Among older adults reporting at least 1 traumatic event (n = 1099)
IES-R = Impact of Event Scale–Revised
PTSS = posttraumatic stress syndrome
Our results showed that 62.3% of the older adults who consulted in the general medical sector reported at least 1 of the 14 potential lifetime traumatic events from the ESA list. They reported, on average, 2.3 traumatic events, and 63% reported 2 or more traumatic events. Among the reported events, exposure to potentially life-threatening disease (12.2% of responses), or the potentially life-threatening illness of a loved one (25.7%), a car accident or other type of accident (14.0%), and exposure to violence in childhood (9.0%) were the most frequently reported.
Our results also showed that 56.6% (n = 622) of patients who consulted in the general medical sector, reported reactions and symptoms associated with a lifetime traumatic event during the last 6 months. However, only 21.7% (n = 135) of older adults reporting posttraumatic stress symptoms also reported an impact of their symptoms on their social functioning during the 6 months preceding their medical visit. Frequencies of people reporting ISF fpr PTSS symptoms are reported in eAppendix B.
The Posttraumatic Stress Syndrome Measurement Model
First, the structure of the IES-R was tested using a confirmatory factorial analysis. The tested model hypothesized a second order measurement model composed of 3 dimensions: intrusion, avoidance, and hyperarousal, as suggested by Brunet et al.37 Our results showed that this model was plausible (χ2 = 2.1, df = 206, P < 0.01; RMSEA = 0.025). In this solution, the validity coefficients of the posttraumatic stress indicators varied from 0.83 to 0.99. The reliability of the IES-R was 0.94. Based on the preceding results, the score of the IES-R was calculated as the sum of the 22 items weighted by their factorial weight (w).
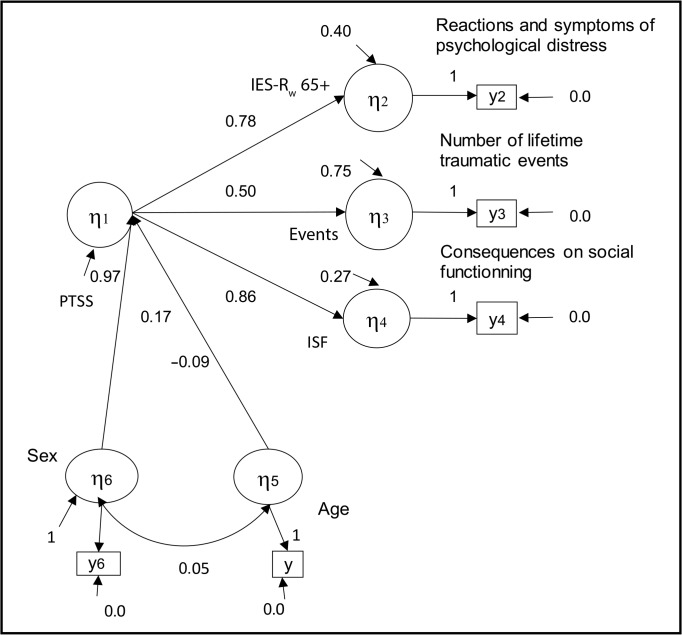
As follows, the factor structure of the PTSS was evaluated. Results showed that a PTSS measurement model consists of 3 indicators—the number of reported traumatic events, the frequency of occurrence of reactions and symptoms of distress associated with the reported events (IES-Rw), and the presence of consequences on social functionality (ISF). In this model, the latent variable PTSS accounted for 60% of the variance of the IES-Rw index and 25% of the observed variance in the number of reported traumatic events. Our results also indicate that the latent variable explains 73% of the variance of the ISF. These results suggest that the impact of reactions and symptoms of distress on ISF is a determinant of the PTSS (1.10 = 0.86/0.78) as important as the frequency of reaction and symptoms of distress associated with the events reported (IES-Rw). The results also show that the number of reported traumatic events is a less important indicator of PTSS. The internal consistency reliability coefficient of the PTSS was 0.82 (Figure 1).
The score of the PTSS was calculated for those who reported at least 1 traumatic event as the sum of the 3 indicators weighted by their factorial loading (βstd) obtained under the constraints of the measurement model. The values of the PTSS varied from 0 to 60 and represent the score that subjects would have, if it was possible to measure directly the PTSS latent construct without error.
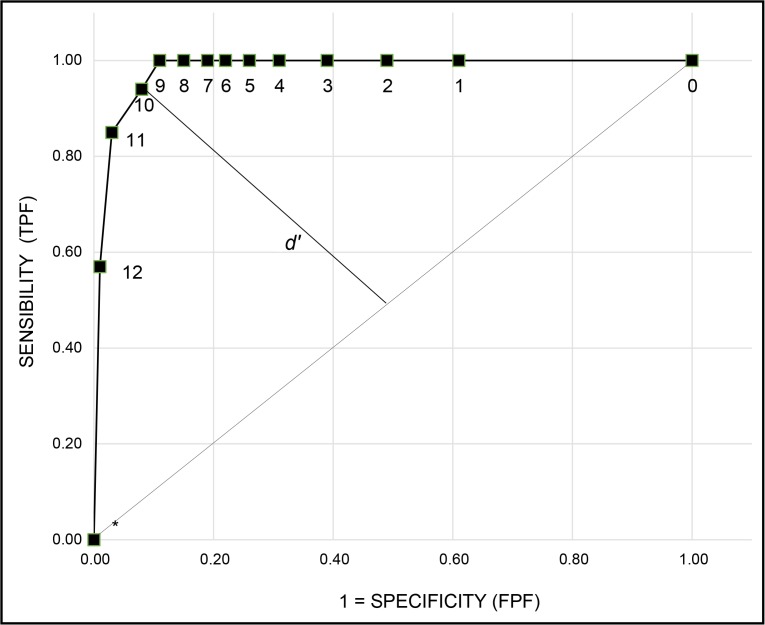
A multivariate analysis (Figure 2) was conducted to test the association between the PTSS and the older adults’ sex and age. Results showed that the explanatory model was plausible (χ2 = 27.12, df = 7, P = 0.003, RMSEA = 0.04). Results showed that women (β = 0.17) were more at risk to report a PTSS than men. In addition, our results indicate that seniors aged 75 years and older were less at risk (β = −0.09) to report a PTSS than those aged between 65 and 75 years. Scores of the PTSS index were grouped into 12 categories to document its sensitivity to detect older adults with probable PTSD. Figure 3 shows the ROC curve observed by plotting the rate of true positive (sensitivity) according to the rate of false positive (1 minus specificity) in detecting subjects with a probable full or partial PTSD for the different values of the PTSS. A value of 0.98 for the AUC index indicates that 98% of the subjects were correctly classified.
Figure 2.
Measurement model of PTSS among older adults
IES-Rw = Impact of Event Scale—Revised; ISF = impairment in social functioning; PTSS = posttraumatic stress syndrome
Figure 3.
ROC curve for several posttraumatic stress syndrome cut-off points
FPF = false-positive fraction; TPF = true-positive fraction
%C+ = (PV+ − P) / P × 100, where P is the prevalence base rate and PV+ is the predictive positive value.
If sn and sp denote sensitivity and specificity, respectively, the distance between the POINT (0.1) and any point on the receiver operating characteristic curve is
The best cut-off point score on the PTSS suggested by the dʹ statistic was 10. The gain in certainty ratio (%C+) obtained for this threshold score was 8.5, which can be interpreted as having a score higher than or equal to 10 on the PTSS scale increases by 8.5 times the certainty of the correct PTSD DSM-IV diagnosis. At the suggested cut-off point, the PTSS showed a sensitivity of 94% in detecting full and partial PTSD and a specificity of 92%. At this threshold, the 6-month prevalence of PTSS was 11.1%. The prevalence of older adults meeting DSM-IV criteria for the full PTSD reached 1.8%, and 1.8% of older adults reached criteria for partial PTSD.
Discussion
The objective of our study was to document the validity and reliability of the PTSS measure used in the ESA Services Study and to report the 6-month prevalence of PTSD in the older adult population. Results showed that a measurement model of PTSS comprising 3 dimensions—the frequency of traumatic events, the presence of psychological distress symptoms associated with the reported events, and the presence of consequences on the social functioning of people who report a traumatic event—was plausible in the older adult population. The reliability of the PTSS was 0.82.
Our results showed that, when the impact on social functioning was considered, 11.1% of the older adults had a probable PTSS according to the PTSS Scale and that 3.6% of older adults reported symptoms meeting DSM-IV criteria for full or partial PTSD during the past 6 months. This result is lower than the 6-month prevalence of full (0.9%) and partial (13.1%) PTSD reported in other studies.15,16
Further, our results showed that women were more at risk to report PTSS than men. This finding is consistent with other community studies,19,20 which have suggested that the sex difference may be due to the type of trauma experienced.48,49 In addition, results showed that older adults aged 75 years and older were less at risk than those aged between 65 and 74 years to report PTSS. This finding is similar to results reported by Pietrzak et al.21 However, results are not consistent with those reported by Chen et al14 which suggested that older age was a risk factor of PTSS.
Our results should be interpreted while considering certain limitations. First, our results are limited to a noninstitutionalized population who were able to participate in an interview at home, and to volunteer to answer a questionnaire on mental health, and who had consulted a doctor in the general medical sector. According to the ESA Services Study, 90% of the population aged 65 years and older in Quebec consulted in the general medical sector at least once during the year. Despite these limitations, our results were based on data obtained from a large sample of older adults and were obtained through a face-to-face interview conducted by trained interviewers using a standardized interview process aiming to minimize the social desirability bias.
Conclusions
The PTSS Scale is a valid scale that also considers the impact of social functioning on the prevalence of this syndrome. Our results lead us to conclude that PTSS is a common mental health problem among older adults seeking health services in the general medical sector.
Abbreviations
- AUC
area under the curve
- CAPS
Clinician-Administrated PTSD Scale
- DSM
Diagnostic and Statistical Manual of Mental Disorders
- ESA
Enquête sur la santé des aînés
- GP
general practitioner
- IES
Impact of Event Scale
- IES-R
IES—Revised
- ISF
impairment in social functioning
- K10
Kessler 10-Item Psychological Distress Scale
- PC
private clinic
- PTSD
posttraumatic stress disorder
- PTSS
posttraumatic stress syndrome
- RMSEA
root mean square error of approximation
- ROC
receiver operating characteristic
References
- 1.American Psychiatric Association (APA) Diagnostic and statistical manual of mental disorders. 4th ed. Washington (DC): APA; 1994. [Google Scholar]
- 2.Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosom Med. 1979;41(3):209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Weathers FW, Litz BT, Herman DS, et al. The PTSD (PCL): reliability, validity and diagnostic utility. Paper presented at the meeting of the International Society for Traumatic Stress Studies; November 25, 1993; San Antonio (TX). [Google Scholar]
- 4.Davidson JRT, Book SW, Colket JT, et al. Assessment of a new self-rating scale for posttraumatic stress disorder. Psychol Med. 1997;27(1):153–160. doi: 10.1017/s0033291796004229. [DOI] [PubMed] [Google Scholar]
- 5.Vreven DL, Gudanowski DM, King LA, et al. The civilian version of the Mississippi PTSD Scale: a psychometric evaluation. J Trauma Stress. 1995;8(1):91–109. doi: 10.1007/BF02105409. [DOI] [PubMed] [Google Scholar]
- 6.Foa EB. Posttraumatic Stress Diagnostic Scale. Minneapolis (MN): National Computer Systems; 1995. [Google Scholar]
- 7.National Collaborating Centre for Mental Health, National Institute for Clinical Excellence . Predictors of PTSD and screening for the disorder. In: Taylor C, editor. Post-traumatic stress disorder: the management of PTSD in adults and children in primary and secondary care. Leicester (GB): Gaskell and the British Psychological Society; 2005. p. 93. [Google Scholar]
- 8.Charles E, Garand L, Ducrocq F, et al. État de stress post-traumatique chez le sujet âgé. Psychol Neuropsychiatr Vieil. 2005;3(4):291–300. [PubMed] [Google Scholar]
- 9.Böttche M, Kuwert P, Knaevelsrud C. Posttraumatic stress disorder in older adults: an overview of characteristics and treatment approaches. Int J Geriatr Psychiatry. 2012;27(3):230–239. doi: 10.1002/gps.2725. [DOI] [PubMed] [Google Scholar]
- 10.Spitzer C, Barnow S, Völzke H, et al. Trauma and posttraumatic stress disorder in the elderly: findings from a German community study. J Clin Psychiatry. 2008;69(5):693–700. doi: 10.4088/jcp.v69n0501. [DOI] [PubMed] [Google Scholar]
- 11.Volkert J, Schulz H, Härter M, et al. The prevalence of mental disorders in older people in Western countries—a meta-analysis. Ageing Res Rev. 2013;12(1):339–353. doi: 10.1016/j.arr.2012.09.004. [DOI] [PubMed] [Google Scholar]
- 12.Byers AL, Yaffe K, Covinsky KE, et al. High occurrence of mood and anxiety disorders among older adults: the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2010;67(5):489–496. doi: 10.1001/archgenpsychiatry.2010.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pietrzak RH, Southwick SM, Tracy M, et al. Posttraumatic stress disorder, depression, and perceived needs for psychological care in older persons affected by Hurricane Ike. J Affect Disord. 2012;138(1–2):96–103. doi: 10.1016/j.jad.2011.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen G, Shen H, Chen G. A cross-sectional study on posttraumatic stress disorder among elderly Qiang citizens 3 years after the Wenchuan earthquake in China. Can J Psychiatry. 2012;57(9):547–553. doi: 10.1177/070674371205700905. [DOI] [PubMed] [Google Scholar]
- 15.van Zelst WH, de Beurs E, Beekman AT, et al. Prevalence and risk factors of posttraumatic stress disorder in older adults. Psychother Psychosom. 2003;72(6):333–342. doi: 10.1159/000073030. [DOI] [PubMed] [Google Scholar]
- 16.van Zelst WH, de Beurs E, Beekman AT, et al. Well-being, physical functioning, and use of health services in the elderly with PTSD and subthreshold PTSD. Int J Geriatr Psychiatry. 2006;21(2):180–188. doi: 10.1002/gps.1448. [DOI] [PubMed] [Google Scholar]
- 17.Washington DL, Davis TD, Der-Martirosian C, et al. PTSD risk and mental health care engagement in a multi-war era community sample of women veterans. J Gen Interm Med. 2013;28(7):894–900. doi: 10.1007/s11606-012-2303-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van Ameringen MV, Mancini C, Patterson B, et al. Post-traumatic stress disorder in Canada. CNS Neurosci Ther. 2008;14(3):171–181. doi: 10.1111/j.1755-5949.2008.00049.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Breslau N, Kessler RC, Chilcoat HD, et al. Trauma and posttraumatic stress disorder in the community. Arch Gen Psychiatry. 1998;55(7):626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- 20.Frissa S, Hatch SL, Gazard B, et al. Trauma and current symptoms of PTSD in a south east London community. Soc Psychiatry Psychiatr Epidemiol. 2013;48(8):1199–1209. doi: 10.1007/s00127-013-0689-8. [DOI] [PubMed] [Google Scholar]
- 21.Pietrzak RH, Goldstein RB, Southwick SM, et al. Psychiatric comorbidity of full and partial posttraumatic stress disorder among older adults in the United States: results from wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Am J Geriatr Psychiatry. 2012;20(5):380–390. doi: 10.1097/JGP.0b013e31820d92e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 23.Sareen J, Cox BJ, Stein MB, et al. Physical and mental comorbidity, disability, and suicidal behavior associated with posttraumatic stress disorder in a large community sample. Psychosom Med. 2007;69(3):242–248. doi: 10.1097/PSY.0b013e31803146d8. [DOI] [PubMed] [Google Scholar]
- 24.Kun P, Tong X, Liu Y, et al. What are the determinants of post-traumatic stress disorder: age, gender, ethnicity or other? Evidence from 2008 Wenchuan earthquake. Public Health. 2013;127(7):644–652. doi: 10.1016/j.puhe.2013.04.018. [DOI] [PubMed] [Google Scholar]
- 25.Zhou X, Kang L, Sun X, et al. Prevalence and risk factors of post-traumatic stress disorder among adult survivors six months after the Wenchuan earthquake. Compr Psychiatry. 2013;54(5):493–499. doi: 10.1016/j.comppsych.2012.12.010. [DOI] [PubMed] [Google Scholar]
- 26.Pietrzak RH, Goldstein RB, Southwick SM, et al. Physical health conditions associated with posttraumatic stress disorder in US older adults: results from wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. J Am Geriatr Soc. 2012;60(2):296–303. doi: 10.1111/j.1532-5415.2011.03788.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Eytan A, Toscani L, Loutan L, et al. Posttraumatic stress disorder and the use of general health services in postwar Kosovo. J Trauma Stress. 2006;19(1):57–67. doi: 10.1002/jts.20098. [DOI] [PubMed] [Google Scholar]
- 28.Brewin CR. Systematic review of screening instruments for adults at risk of PTSD. J Trauma Stress. 2005;18(1):53–62. doi: 10.1002/jts.20007. [DOI] [PubMed] [Google Scholar]
- 29.Weiss DS, Marmar CR. The Impact of Event Scale—Revised. In: Wilson JP, Keane TM, editors. Assessing psychological trauma and PTSD. New York (NY): Guilford Press; 1997. pp. 399–411. [Google Scholar]
- 30.Christianson S, Marren J. The Impact of Event Scale—Revised (IES-R) Medsurg Nurs. 2012;21(5):321–322. [PubMed] [Google Scholar]
- 31.Asukay N, Kato H, Kawamura N, et al. Reliability and validity of the Japanese-language version of the Impact of Event Scale—Revised (IES-R-J): four studies of different traumatic events. J Nerv Ment Dis. 2002;190(3):175–182. doi: 10.1097/00005053-200203000-00006. [DOI] [PubMed] [Google Scholar]
- 32.Creamer M, Bell R, Failla S. Psychometric properties of the Impact of Event Scale—Revised. Behav Res Ther. 2003;41(12):1489–1496. doi: 10.1016/j.brat.2003.07.010. [DOI] [PubMed] [Google Scholar]
- 33.Beck JG, Grant DM, Read JP, et al. The Impact of Event Scale—Revised: psychometric properties in a sample of motor vehicle accident survivors. J Anxiety Disord. 2008;22(2):187–198. doi: 10.1016/j.janxdis.2007.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Blake DD, Weathers FW, Nagy LM, et al. The development of a Clinician-Administered PTSD Scale. J Trauma Stess. 1995;8(1):75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- 35.Sorocco KH, Lauderdale S. Cognitive behavior therapy with older adults: innovations across care settings. New York (NY): Springer Publishing Company; 2011. [Google Scholar]
- 36.Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32(6):959–956. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- 37.Brunet A, St-Hilaire A, Jehel L, et al. Validation of a French version of the Impact of Event Scale—Revised. Can J Psychiatry. 2003;48(1):56–61. doi: 10.1177/070674370304800111. [DOI] [PubMed] [Google Scholar]
- 38.Pietrzak RH, Goldstein RB, Southwick SM, et al. Medical comorbidity of full and partial posttraumatic stress disorder in US adults: results from wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Psychosom Med. 2011;73(8):697–707. doi: 10.1097/PSY.0b013e3182303775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jöreskog KG, Sörbom D. LISREL 880 for Windows [software] Lincolnwood (IL): Scientific Software International, Inc; 2006. [Google Scholar]
- 40.Wheaton B, Muthen B, Alwin DF, et al. Assessing reliability and stability in panel models. In: Heise DR, editor. Sociological methodology. San Francisco (CA): Jossey-Bass; 1977. [Google Scholar]
- 41.Bollen KA. Structural equations with latent variables. New York (NY): John Wiley & Sons; 1989. [Google Scholar]
- 42.Hancock GR, Mueller RO. Rethinking construct reliability within latent variable systems. In: Cudeck R, Du Toit S, Sörbom D, editors. Structural equation modeling: present and future A Festschrift in honor of Karl Jöreskog. Lincolnwood (IL): Scientific Software International, Inc; 2001. [Google Scholar]
- 43.Hanley JA, McNeil BJ. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology. 1983;148(3):839–843. doi: 10.1148/radiology.148.3.6878708. [DOI] [PubMed] [Google Scholar]
- 44.Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143(1):29–36. doi: 10.1148/radiology.143.1.7063747. [DOI] [PubMed] [Google Scholar]
- 45.Connell FA, Koepsell TD. Measures of gain in certainty from a diagnostic test. Am J Epidemiol. 1985;121(5):744–753. doi: 10.1093/aje/121.5.744. [DOI] [PubMed] [Google Scholar]
- 46.Institut de la statistique du Québec . Population selon le groupe d’âge, hommes, régions administratives et ensemble du Québec, 2011 [Internet] Quebec (QC): Institut de la statistique du Québec; 2012. [cited 2013 Aug 14]. Available from: http://www.stat.gouv.qc.ca/regions/recens2011_reg/population/popmasc_reg.htm. [Google Scholar]
- 47.Institut de la statistique du Québec . Population selon le groupe d’âge, femmes, régions administratives et ensemble du Québec, 2011 [Internet] Quebec (QC): Institut de la statistique du Québec; 2012. [cited 2013 Aug 14]. Available from: http://www.stat.gouv.qc.ca/regions/recens2011_reg/population/popfem_reg.htm. [Google Scholar]
- 48.Baker CK, Norris FH, Diaz DMV, et al. Violence and PTSD in Mexico: gender and regional differences. Soc Psychiatry Psychiatr Epidemiol. 2005;40(7):519–528. doi: 10.1007/s00127-005-0921-2. [DOI] [PubMed] [Google Scholar]
- 49.Breslau N, Chilcoat HD, Kessler RC, et al. Vulnerability to assaultive violence: further specification of the sex difference in post-traumatic stress disorder. Psychol Med. 1999;29(4):813–821. doi: 10.1017/s0033291799008612. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.