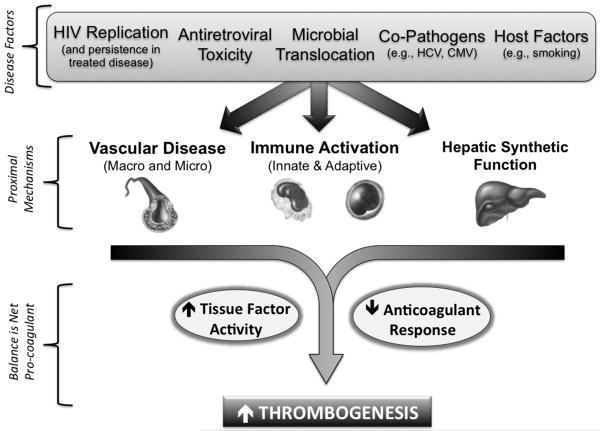
Figure 1. Pro-Coagulant Mechanisms During Chronic HIV Disease.
Presented is a conceptual model whereby factors specific to HIV itself, antiretroviral therapy, and lifestyle contribute to a pro-coagulant state. In addition, permanent damage to the immune system during chronic HIV disease despite effective ART treatment also contributes, including: a) decreased integrity of the mucosal lymphatic barrier, with corresponding endotoxemia, and b) a loss of T-cell regulatory function combined with excess antigen stimulus from co-pathogens. This contributes to a state of persistent immune activation (characterized by both T-cell and monocyte abnormalities), injury to endothelial surfaces with micro-vascular dysfunction, premature atherosclerosis, and potentially, impaired hepatic synthesis of coagulation factors. The end-result may increased thrombogenesis due to both an up-regulation of tissue factor activity, as well as alterations in extrinsic pathway factor levels with notable declines in the anticoagulant response (e.g., antithrombin and protein C).