A 41-year-old man with a three-year history of intermittent shortness of breath, productive cough and hemoptysis clinically diagnosed as asthma, presented to the emergency department acutely short of breath. Computed tomography of the chest for pulmonary embolism was negative; however, revealed diffuse nodular thickening of the trachea, main stem, lobar and segmental airways associated with luminal narrowing and calcification (Figure 1). Tracheobronchial amyloidosis was the favoured imaging diagnosis, despite sparing of the membranous trachea, which is usually involved. Bronchoscopy was performed to obtain biopsy samples for definitive diagnosis.
Figure 1).
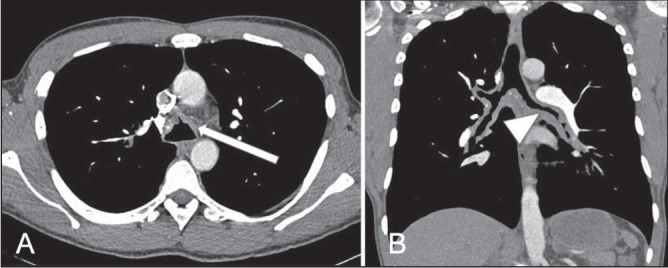
Images from a computed tomography pulmonary embolism study in soft tissue windows showing calcified nodular mural thickening of the trachea and central airways. A Anterolateral trachea (arrow). B Main and lobar bronchi with luminal narrowing, particularly on the left (arrowhead)
Infiltration of the anterior/lateral trachea, main-stem bronchial and segmental airway walls with mucosal cobblestoning and airway narrowing was visualized (Figure 2A). Bronchial biopsies demonstrated extensive subepithelial amorphous eosinophilic material that stained positive with Congo red and showed apple-green birefringence under polarized light (Figure 2B), confirming tracheobronchial amyloidosis (TBA), subtyped by mass spectrometry as lambda-type amyloid. Work-up for plasma cell dyscrasia and multiple myeloma was negative. Treatment included tumour debulking (mechanical and argon plasma coagulation) followed by balloon dilation via rigid bronchoscopy and external beam radiation therapy to prevent recurrence. Further treatment with chemotherapy (melphalan and dexamethasone) was planned; however, the patient was lost to follow-up.
Figure 2).
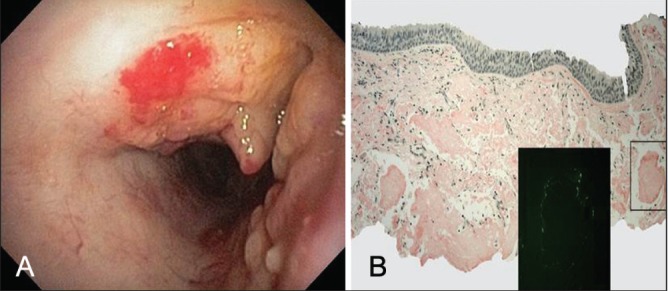
Bronchoscopic view of mid trachea showing nodular thickening with cobblestone appearance and luminal narrowing, relatively sparing the membranous portion (A). Tracheal biopsy showing submucosal amyloid deposits staining positive with Congo red (original magnification ×40) and apple-green birefringence under polarized light (original magnification ×200) (B)
KEY LEARNING POINTS
A targeted airway survey on chest radiographs obtained for investigation of asthma is necessary to avoid missing large airway pathology.
It is important to recognize the specific computed tomography imaging features of TBA including involvement of the membranous trachea and calcification (1–3).
The imaging features of TBA, a rare subtype of respiratory amyloidosis, are not specific and biopsy is required to confirm the diagnosis. Investigations to exclude multiple myeloma and plasma cell dyscrasia should be performed (4–6).
The ‘Images in Respiratory Medicine’ section of the Canadian Respiratory Journal aims to highlight the importance of visual interpretation, whether physiological, radiological, bronchoscopic, surgical/thorascopic or histological, in the diagnosis of chest diseases. Submissions should exemplify a classic, particularly dramatic or intriguing presentation of a disease while offering an important educational message to the reader (insightful diagnostic pearls or differential diagnosis, etc). This section is not intended to be a vehicle for publication of case reports (see the Clinical-Pathologic-Conferences for case-based leaning series).
REFERENCES
- 1.Yamamoto T, Maeda M, Mizuno S, et al. Primary diffuse tracheobronchial amyloidosis: Radiologic findings. J Thorac Imag. 2001;16:177–80. doi: 10.1097/00005382-200107000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Kwong JS, Muller NL, Miller RR. Disease of the trachea and main-stem bronchi: Correlation of CT with pathologic findings. RadioGraphics. 1992;12:645–57. doi: 10.1148/radiographics.12.4.1636031. [DOI] [PubMed] [Google Scholar]
- 3.Webb EM, Grett M, Elicker W, Webb R. Using CT to diagnose nonneoplastic tracheal abnormalities: Appearance of the tracheal wall. Am J Roentgenol. 2000;174:1315–21. doi: 10.2214/ajr.174.5.1741315. [DOI] [PubMed] [Google Scholar]
- 4.Cordier JF, Loire R, Brune J. Amyloidosis of the lower respiratory tract: Clinical and pathologic features in a series of 21 patients. Chest. 1986;90:827–31. doi: 10.1378/chest.90.6.827. [DOI] [PubMed] [Google Scholar]
- 5.Ding L, Li W, Wang K, et al. Primary tracheobronchial amyloidosis in China: Analysis of 64 cases and a review of literature. J Hauzhong Univ Sci Techonol. 2010;30:599–603. doi: 10.1007/s11596-010-0549-7. [DOI] [PubMed] [Google Scholar]
- 6.Shah PL, Gillmore JD, Copley SJ, et al. The importance of complete screening for amyloid fibril type and systemic disease in patients with amyloidosis in the respiratory tract. Sarcoidosis Vasc Diffuse Lung Dis. 2002;19:134–42. [PubMed] [Google Scholar]


