MMWR in Brief summarizes key points from “Outbreaks of Acute Gastroenteritis Transmitted by Person-to-Person Contact—United States, 2009–2010.” MMWR 2012;61(No. SS-9). Available at http://www.cdc.gov/mmwr/pdf/ss/ss6109.pdf. Certain text might not have appeared in the original publication. Reprinted from: http://www.cdc.gov/mmwr/pdf/ss/ss6109_brief.pdf. For more information about MMWR in Brief reprints, see: http://ajph.aphapublications.org/doi/pdf/10.2105/AJPH.2014.302321.
NEW INFORMATION
This is the first report to describe the available national surveillance data on acute gastroenteritis (AGE) outbreaks spread primarily from person-to-person and the frequency of this mode of transmission.
ANALYSIS
Frequencies of outbreaks and outbreak-associated illnesses by etiology, setting, and month of first illness onset are presented. Outbreak incidence in each reporting site was calculated using US Census Bureau data and expressed per 1 million population per year.
SUMMARY FINDINGS
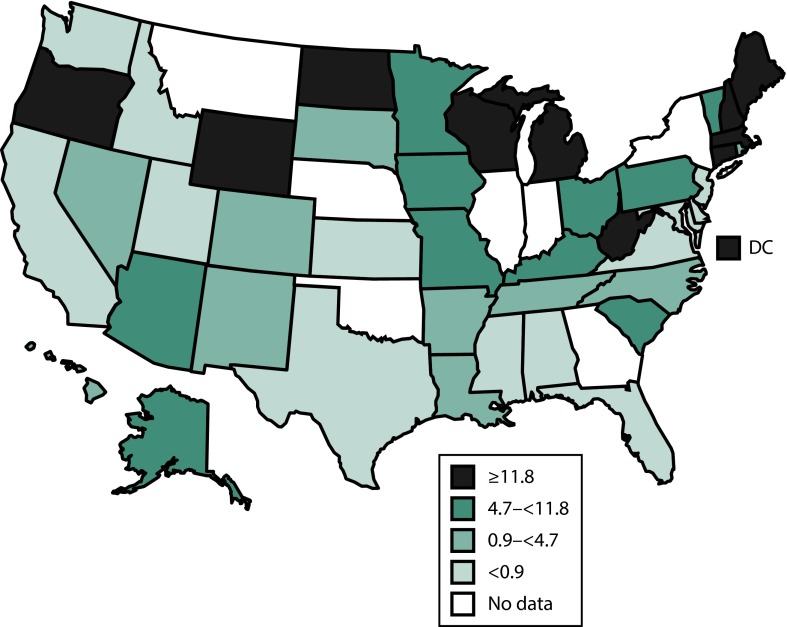
During 2009–2010, the rate of reported outbreaks of AGE transmitted by person-to-person varied by state, ranging from 0.03 to 41.90 per 1 million population per year (Figure 1). Person-to-person AGE outbreaks were most often suspected or confirmed to be caused by norovirus and occurred most often in winter months (Figure 2) and in nursing homes and other long-term–care facilities.
FIGURE 1—
Rate of outbreaks of acute gastroenteritis transmitted by person-to-person contact, by state: National Outbreak Reporting System, United States, 2009–2010.
Note. Incidence of outbreaks per state, per million population, on the basis of US Census Bureau population estimates. For states reporting outbreaks in both 2009 and 2010, the average number of outbreaks per year was used to calculate the incidence. For states reporting outbreaks for 1 y, the incidence per 1 million population for that single year was used. The sample size was n = 2259.
FIGURE 2—
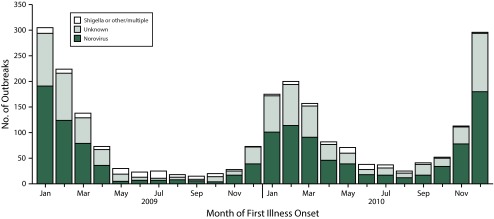
Number of outbreaks of acute gastroenteritis transmitted by person-to-person contact, by month of first illness onset and etiology: National Outbreak Reporting System, United States, 2009–2010.
Note. The sample size was n = 2259. The “other/multiple” category includes Salmonella spp., rotavirus, Shiga toxin-producing E. coli (STEC), Giardia lamblia, Cryptosporidium spp., Clostridium difficile, sapovirus, Campylobacter jejuni, and outbreaks with multiple etiologies.
DATA SOURCE AND METHODS
Implemented in 2009, the National Outbreak Reporting System (NORS) is a voluntary national surveillance system for waterborne and foodborne disease outbreaks as well as AGE outbreaks from person-to-person contact, animal contact, environmental contamination, and unknown modes of transmission. These outbreaks are primarily detected and investigated by state and local public health agencies in the United States and its territories, and reported to CDC via NORS.
Data are reported using standardized methods on general outbreak characteristics (e.g., dates, number of illnesses, geography, and settings), demographic characteristics of patients (e.g., age and sex), symptoms, case outcomes, and laboratory testing information and results. A reported etiology was considered confirmed if 2 or more laboratory-confirmed cases were reported, consistent with CDC guidelines. If a reported etiology was not associated with 2 or more laboratory-confirmed cases, but had supporting epidemiologic or clinical data, it was classified as a suspected etiology. Only outbreaks reported in NORS with a primary mode of transmission of person-to-person contact are included in this report.
MAIN RESULTS
During 2009–2010, a total of 2259 person-to-person AGE outbreaks were reported in NORS from 42 states and the District of Columbia (Figure 1). No etiology was reported in approximately 40% (n = 840) of outbreaks. Of the remaining 1419 outbreaks with a reported etiology, 1270 (89%) were either suspected or confirmed to be caused solely by norovirus. Other reported etiologies included Shigella (n = 86), Salmonella (n = 16), Shiga toxin-producing Escherichia coli (STEC) (n = 11), and rotavirus (n = 10). Most (82%; n = 1723) of the 2110 outbreaks caused by norovirus or an unknown etiology occurred during the winter months, and outbreaks caused by Shigella or another suspected or confirmed etiology most often occurred during the spring or summer months (62% [n = 53] and 60% [n = 38], respectively; Figure 2).
These outbreaks resulted in 81 491 reported illnesses, 1339 hospitalizations, and 136 deaths. The mean number of cases per outbreak was significantly higher in norovirus outbreaks (44 cases per outbreak) than in outbreaks attributable to Shigella (15 cases), multiple or other etiology (22 cases), or an unknown etiology (27 cases). Of the 136 reported deaths, 118 (87%) occurred in norovirus outbreaks. Persons described in outbreaks caused by Shigella were significantly more likely to seek health care (i.e., outpatient health-care provider visits, emergency department visits, and hospitalizations combined) than were those associated with norovirus outbreaks (odds ratio = 10.2; 95% confidence interval = 9.3,11.2); however, norovirus outbreaks accounted for the largest number of deaths (118) and health-care visits (2931).
A setting was reported for 1187 (53%) outbreaks. Among these reported settings, nursing homes and other long-term–care facilities were most common (80%), followed by childcare centers (6%), hospitals (5%), and schools (5%).
LIMITATIONS
NORS, a new reporting system with variable adoption and use, is subject to underreporting. Only 4 reporting variables (primary transmission mode, date of first illness, reporting site, and total ill) are required to submit an outbreak report via NORS, resulting in varying levels of completeness of other variables collected (e.g., age, sex, etiology, and setting).
PUBLIC HEALTH IMPLICATIONS
During 2009–2010, norovirus was the most commonly reported cause of AGE outbreaks spread through person-to-person contact, accounted for the majority of deaths and health-care visits associated with these outbreaks, and on the basis of epidemiologic characteristics, likely accounted for a substantial portion of the reported outbreaks of unknown etiology. Prevention and control of person-to-person AGE outbreaks depend primarily on appropriate hand hygiene and isolation of ill persons.
NORS surveillance data can help identify the etiologic agents, settings, and populations most often involved in AGE outbreaks resulting primarily from person-to-person transmission and guide development of targeted interventions to avert these outbreaks or mitigate the spread of infection. Surveillance for person-to-person AGE outbreaks via NORS also might be important in clarifying the relative role of person-to-person transmission for certain pathogens (e.g., STEC) that have been traditionally considered foodborne. As ongoing improvements and enhancements to NORS are introduced, use of NORS has the potential to increase, allowing for improved estimation of epidemic person-to-person AGE and its relative importance among other modes of transmission.