Summary
Carotid body tumour is a rare disease, a slow growing highly vascular tumour of the carotid body tissue and the most common type of the paraganglioma. This article reviews the pathological, clinical and ultrasound features of carotid body tumours and discusses the role of duplex ultrasound in the diagnosis and assessment of this condition. The initial presentation of carotid body tumour is usually a painless palpable neck mass. Some patients may experience local pressure symptoms as well as symptoms from vagal, hypoglossal and cervical sympathetic nerve impingement. Percutaneous needle aspiration or incisional biopsy is contraindicated for the diagnosis of carotid body tumours. Duplex ultrasound, computed tomography scan, magnetic resonance scan and angiography are commonly used diagnostic tools for this condition. Complete surgical excision of carotid body tumour is the treatment of choice as radiation therapy and chemotherapy are unsatisfactory. Based on vascularity and location, duplex ultrasound scan is able to diagnose carotid body tumour and differentiate it from many other masses in the neck. This non-invasive, inexpensive and readily available diagnostic tool can be used as a first-line imaging modality for the diagnosis and assessment of carotid body tumours.
Keywords: Carotid body tumour, ultrasound, literature review
1. Introduction
Carotid body tumour is a rare disease. It is estimated the incidence of carotid body tumour is about 1 in 30,000. Most vascular surgeons will encounter very few during their career (1). Angiography has been the gold standard for the diagnosis and management of carotid body tumours for many years. Duplex ultrasound has been increasingly used in the diagnosis and assessment of carotid body tumours since colour flow imaging was introduced and became a non-invasive alternative imaging modality. This article will review the pathological, clinical and ultrasound features of carotid body tumours and discuss the role of duplex ultrasound in the diagnosis and assessment of this condition.
2. Carotid body
The carotid body was first described by Von Haller in 1743 (2). It is a chemoreceptor located in the adventitia of the carotid bifurcation. The size of a carotid body is approximately 5 mm × 3 mm × 2 mm. When the carotid body detects decreasing levels of oxygen (hypoxia), increasing levels of carbon dioxide (hypercapnia) and decreasing pH (acidosis), it increases respiratory rate, tidal volume, heart rate, and blood pressure together with vasoconstriction, and the production of circulating catecholamines (3).
3. Carotid body tumour
Carotid body tumour is hypertrophy of the carotid body tissue, which is the most common type of the paraganglioma. It also known as a chemodectoma, endothelioma, glomus caroticum, perithelioma, chromaffinoma and nonchromaffin paraganglioma. Carotid body tumours may be familial (10–50%) (4) or non-familial. The incidence of bilateral carotid body tumours is 32% in the familial group (5,6), and 5% in the non-familial group (7–9). Most carotid body tumours are slow growing and benign. Approximately 5–10% of carotid body tumours may progress to malignancy, with local vascular and/or lymph node invasion, and rarely distant metastases (9–12).
3.1. Pathology
Macroscopically, carotid body tumours are well circumscribed, rubbery, and reddish brown. Microscopically, the tumours are highly vascular; between the many capillaries are clusters of cells, including supporting cells and chief cells. Cytochemical techniques usually demonstrate epinephrine, norepinephrine and serotonin in these cells (13). Unlike other neoplasms, malignant carotid body tumour does not have histological transformation (9,13,14). The diagnosis of malignancy is based on vascular/lymph node invasion and metastases.
3.2. Clinical Presentation
The initial presentation of carotid body tumour is usually a painless, palpable neck mass. Some patients may experience local pressure symptoms, such as neck or ear pain, sore throat, local tenderness and odynophagia. Symptoms from vagal, hypoglossal and cervical sympathetic nerve impingement, such as hoarseness, dysphasia, dysarthria, swallowing difficulties and Horner's syndrome may occur (15,16). Other symptoms may include dizziness, headache, flushing, palpitations, tachycardia, arrhythmias, diaphoresis and photophobia (17).
Physical examination reveals a mass which may be pulsatile, located below the angle of the mandible is typically laterally mobile but vertically fixed. The mass is usually nontender, rubbery, firm and noncompressible. A bruit may be audible. Neurologic abnormalities caused by vagal or hypoglossal nerve involvement and Horner's syndrome are unusual but may appear in some patients.
Based on the size and relationship to the carotid arteries, carotid body tumours may be divided into three groups (9) (Table 1).
Table 1. Shamblin classification of carotid body tumours.
| Group | Tumour size | Relationship with carotid arteries | Surgical treatment |
|---|---|---|---|
| Group I | Relatively small | Minimally attach to the carotid arteries | Surgical excision is not difficult |
| Group II | Larger | Moderately attach to the carotid arteries | Often require a carotid shunt |
| Group III | Very large | Encase the carotid arteries | Often require arterial resection and grafting |
3.3. Diagnosis
Medical history and physical examination are essential for the diagnosis of carotid body tumour. Due to the vascular nature of carotid body tumours, percutaneous needle aspiration or incisional biopsy is contraindicated as it may cause massive haemorrhage, pseudoaneurysm formation and carotid thrombosis (14,16). As direct biopsy is not suitable for the diagnosis of carotid body tumour, diagnostic imaging modalities are important in the diagnosis and differential diagnosis of this condition.
Duplex ultrasound is commonly used to evaluate neck masses. Computed tomography (CT) and magnetic resonance (MR) scans, especially MR scans (Figure 1) are better for demonstrating the relationship of the neck mass to adjacent structures (18,19). Angiography (Figure 2) is capable of demonstrating unusual blood supply to the carotid body tumour, such as contributions from the internal carotid artery, vertebral artery and thyrocervical trunk and has played an important role for the surgical management of carotid body tumours (20,21); although it has been not used very often in some vascular units in recent years (1).
Figure 1.
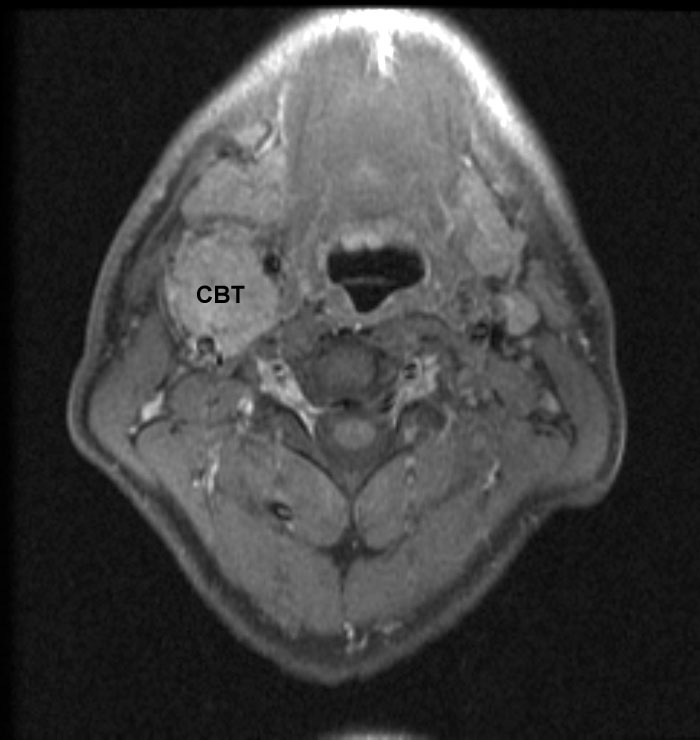
Carotid body tumour (CBT): MRI.
Figure 2.

Carotid body tumour (CBT): angiography.
3.4. Treatment
Surgical resection of a carotid body tumour was first attempted by Reigner in 1880, but the patient did not survive the operation (22). Maydl was the first to resect a carotid body tumour on a patient who survived in 1886, although the patient suffered from a postoperative stroke and became aphasic and hemiplegic (23). The first successful carotid body tumour excision was performed by Albert in 1889 (1). Complete surgical excision of carotid body tumour is still the treatment of choice as the tumour has a 5% or greater incidence of metastases; radiation therapy and chemotherapy are unsatisfactory. Surgical removal of small, asymptomatic carotid body tumour is recommended as it has a much lower risk of cranial nerve and carotid artery injuries than excision of a large tumour. If the size of carotid body tumour is more than 5 cm, operative mortality is 1–3% (24).
When the carotid body tumour is large, preoperative embolisation has been used to decrease the vascularity of the tumour and lower operative blood loss thereby reducing technical difficulty (25–27). However, preoperative embolisation is still controversial as it may cause internal carotid or cerebral artery thrombosis (28).
4. Ultrasound assessment of carotid body tumour
4.1. Ultrasound assessment of carotid body tumours
Ultrasound scan is a non-invasive, inexpensive and readily available imaging tool, has been used to diagnose carotid body tumours since the late 1970s (29–32). The development Doppler colour flow image (33) and power Doppler image (34) have enhanced capabilities of ultrasound to assess carotid body tumours.
4.2. Duplex ultrasound features of carotid body tumour
Duplex ultrasound characteristics of a carotid body tumour is of a highly vascularised solid hypoechoic mass in the area of the carotid bifurcation, which usually causes splaying of the bifurcation and separation of the internal and external carotid arteries (Figures 3 and 4).
Figure 3.
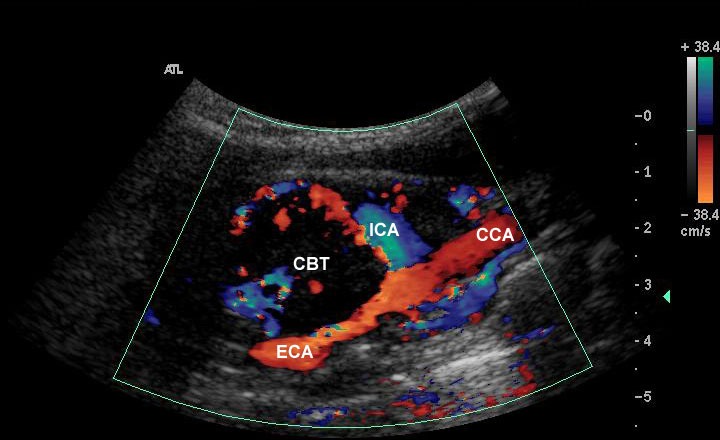
Duplex ultrasound - longitudinal view: carotid body tumour at carotid bifurcation. CCA, common carotid artery; ICA, internal carotid artery; ECA, external carotid artery; CBT, carotid body tumour.
Figure 4.
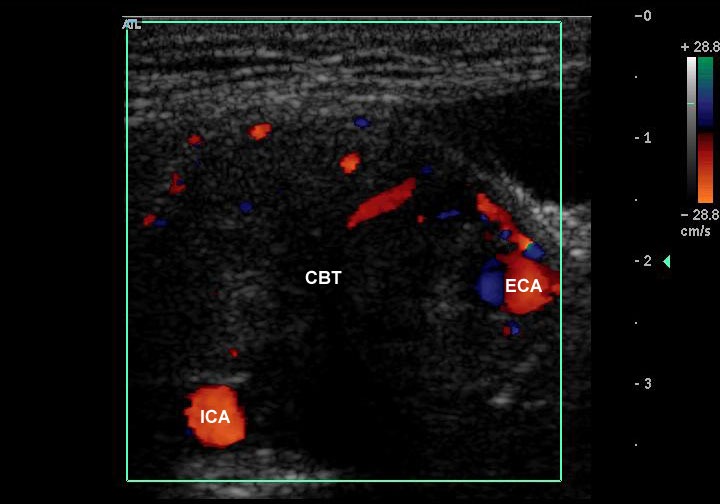
Duplex ultrasound - transverse view: the internal and external carotid arteries are separated by the tumour. ICA, internal carotid artery; ECA, external carotid artery; CBT, carotid body tumour.
On colour flow imaging, hypervascularity of the tumour is seen as irregular colour signals with flow direction being predominantly cephalad (35,36). Typical pulsed Doppler flow patterns from carotid body tumour have a low resistance character with a high diastolic component (37). Power Doppler imaging shows abundant flow, characterized as intense blush, throughout the tumours (34).
4.3. Role of duplex ultrasound in the diagnosis and assessment of carotid body tumour
Based on the above described ultrasound features, carotid body tumour is not difficult to diagnose by a duplex ultrasound scan. Since duplex ultrasound is a non-invasive, inexpensive and readily available diagnostic modality, it has been recommended for screening familial carotid body tumour (38).
Vascularity and location are the two key factors used by ultrasound to differentiate carotid body tumours from other neck mass, such as lymphomas, metastatic tumours, thyroid lesions, submandibular salivary gland tumours, and branchial cleft cysts. However, it can be difficult for ultrasound scan to distinguish carotid body tumour from other types of paraganglioma, such as glomus vagale tumour when it is located at the carotid bifurcation, as they have a similar ultrasound appearance (39).
In addition to the diagnosis and differential diagnosis of carotid body tumours, duplex ultrasound can provide information on carotid body tumour dimensions, blood supply of the tumour and coexistent carotid artery disease, which is useful in forming a treatment plan and assessing the risk of surgery.
4.4. Limitations of ultrasound in the assessment of carotid body tumour
Despite the usefulness of duplex ultrasound in the assessment of carotid body tumour, the limitations of ultrasound include the inability to differentiate carotid body tumour from other type of paraganglioma in the region (39) and limited ability to identify complex blood supply to a large carotid body tumour (33). CT and/or MRI are better in differentiating of carotid body tumour from other paraganglioma, and angiography is better for the identification of blood supply to the carotid body tumour.
5. Conclusion
Duplex ultrasound is a noninvasive, inexpensive and readily available diagnostic tool, capable of diagnosing carotid body tumour based on its vascularity and location, and can be used as a first-line imaging modality for the diagnosis and assessment of carotid body tumours.
Acknowledgements
The author would like to thank Mr G Fell, Director of Vascular Surgery Unit, Austin Hospital for his comments and suggestions.
References
- 1. Sajid MS, Hamilton G, Baker DM; Joint Vascular Research Group. A multicenter review of carotid body tumour management. Eur J Vasc Endovasc Surg. 2007; 34:127-130 [DOI] [PubMed] [Google Scholar]
- 2. Von Haller: Cited by Gratiot JH. Carotid tumors: A collective review. Abstr Surg. 1943; 7:117-186 [Google Scholar]
- 3. Frey CF, Karoll RP. Management of chemodectomas. Am J Surg. 1966; 111:536-542 [DOI] [PubMed] [Google Scholar]
- 4. Pellitteri PK, Rinaldo A, Myssiorek D, Gary Jackson C, Bradley PJ, Devaney KO, Shaha AR, Netterville JL, Manni JJ, Ferlito A. Paragangliomas of the head and neck. Oral Oncol. 2004; 40:563-575 [DOI] [PubMed] [Google Scholar]
- 5. Grufferman S, Gillman MW, Pasternak LR, Peterson CL, Young WG, Jr. Familial carotid body tumors: Case reports and epidemiologic review. Cancer. 1980; 46:2116-2122 [DOI] [PubMed] [Google Scholar]
- 6. Hallett JW, Jr, Nora JD, Hollier LH, Cherry KJ, Jr, Pairolero PC. Trends in neurovascular complications of surgical management for carotid body and cervical paragangliomas: A fifty-year experience with 153 tumors. J Vasc Surg. 1988; 7:284-291 [PubMed] [Google Scholar]
- 7. Javid H, Chawla SK, Dye WS, Hunter JA, Najafi H, Goldin MD, Serry C. Carotid body tumors: Resection or reflection. Arch Surg. 1976; 111:344-347 [DOI] [PubMed] [Google Scholar]
- 8. Mciirath DC, Remine WH. Carotid-body tumors. Surg Clin North Am. 1963; 43:1135-1144 [DOI] [PubMed] [Google Scholar]
- 9. Shamblin WR, ReMine WH, Sheps SG, Harrison EG, Jr. Carotid body tumor (chemodectoma): Clinicopathologic analysis of ninety cases. Am J Surg. 1971; 122:732-739 [DOI] [PubMed] [Google Scholar]
- 10. Irons GB, Weiland LH, Brown WL. Paragangliomas of the neck: Clinical and pathological analysis of 116 cases. Surg Clin North Am. 1977; 57:575-583 [DOI] [PubMed] [Google Scholar]
- 11. Lees CD, Levine HL, Beven EG, Tucker HM. Tumors of the carotid body: Experience with 41 operative cases. Am J Surg. 1981; 142:362-365 [DOI] [PubMed] [Google Scholar]
- 12. Romanski R. Chemodectoma (non-chromaffinic paraganglioma) of the carotid body with distant metastases with illustrative case. Am J Pathol. 1954; 30:1-13 [PMC free article] [PubMed] [Google Scholar]
- 13. Grimley PM, Glenner GG. Histology and ultra-structure of carotid body paragangliomas: Comparison with a normal gland. Cancer. 1967; 20:1473-1488 [DOI] [PubMed] [Google Scholar]
- 14. Staats EF, Brown RL, Smith RR. Carotid body rumors, benign and malignant. Laryngoscope. 1966; 76:907-916 [DOI] [PubMed] [Google Scholar]
- 15. Davidge-Pitts KJ, Pantanowitz D. Carotid body tumors. Surg Annu. 1984; 16:203-227 [PubMed] [Google Scholar]
- 16. Padberg FT, Jr, Cady B, Persson AV. Carotid body tumor: The Lahey Clinic experience. Am J Surg. 1983; 145:526-528 [DOI] [PubMed] [Google Scholar]
- 17. Wright DJ, Pandya A, Noel F. Anesthesia for carotid body tumour resection. Anaesthesia. 1979; 34:806-808 [DOI] [PubMed] [Google Scholar]
- 18. Olsen WL, Dillon WP, Kelly WM, Norman D, Brant-Zawadzki M, Newton TH. MR imaging of paragangliomas. AJR Am J Roentgenol. 1987; 148:201-204 [DOI] [PubMed] [Google Scholar]
- 19. Vogl T, Brüning R, Schedel H, Kang K, Grevers G, Hahn D, Lissner J. Paragangliomas of the jugular bulb and carotid body: MR imaging with short sequences and Gd-DTPA enhancement. AJR Am J Roentgenol. 1989; 153:583-587 [DOI] [PubMed] [Google Scholar]
- 20. Chambers RG, Mahoney WD. Carotid body tumors. Am J Surg. 1968; 116:554-558 [DOI] [PubMed] [Google Scholar]
- 21. Yaghami I, Shariat S, Shamloo M. Carotid body rumors. Radiology. 1970; 97:559-563 [DOI] [PubMed] [Google Scholar]
- 22. Reigner: Cited by Lahey FH, Warren KW. A long-term appraisal of carotid tumors with remarks on their removal. Surg Gynecol Obstet. 1951; 92:481-491 [PubMed] [Google Scholar]
- 23. Maydl: Cited by Byme JJ. Carotid body and allied tumors. Am J Surg. 1958; 95:371-384 [DOI] [PubMed] [Google Scholar]
- 24. Luna-Ortiz K, Rascon-Ortiz M, Villavicencio-Valencia V, Herrera-Gomez A. Does Shamblin's classification predict postoperative morbidity in carotid body tumors? A proposal to modify Shamblin's classification? Eur Arch Otorhinolaryngol. 2006; 263:171-175 [DOI] [PubMed] [Google Scholar]
- 25. LaMuraglia GM, Fabian RL, Brewster DC, Pile-Spellman J, Darling RC, Cambria RP, Abbott WM. The current surgical management of carotid body paragangliomas. J Vasc Surg. 1992; 15:1038-1044 [DOI] [PubMed] [Google Scholar]
- 26. Robison JG, Shagets FW, Beckett WC, Jr, Spies JB. A multidiscipiinary approach to reducing morbidity and operative blood loss during rcsection of carotid body tumor. Surg Gynecol Obstet. 1989; 168:166-170 [PubMed] [Google Scholar]
- 27. Smith RF, Shetty PC, Reddy DJ. Surgical treatment of carotid paragangliomas presenting unusual technical difficulties: The value of preoperative embolization. J Vasc Surg. 1988; 7:631-637 [PubMed] [Google Scholar]
- 28. Pandya SK, Nagpal RD, Desai AP, Purohit AT. Death following extemal carotid arterial embolization for a functioning glomus jugular chemodectoma. J Neurosurg. 1978; 48:1030-1034 [DOI] [PubMed] [Google Scholar]
- 29. Gooding GAW. Gray-scale ultrasound detection of carotid body tumors. Radiology 1979; 132:409-410 [DOI] [PubMed] [Google Scholar]
- 30. Lewis RR, Beasley MG, Coghlan BA, Yates AK, Gosling RG. Demonstration of a carotid body tumour by ultrasound. Br J Radiol. 1980; 53:368-371 [DOI] [PubMed] [Google Scholar]
- 31. Mäkäräinen H, Päivänsalo M, Hyrynkangas K, Leinonen A, Siniluoto T. Sonographic patterns of carotid body tumors. J Clin Ultrasound. 1986; 14:373-375 [DOI] [PubMed] [Google Scholar]
- 32. Gritzmann N, Herold C, Haller J, Karnel F, Schwaighofer B. Duplex sonography of tumors of the carotid body. Cardiovasc Intervent Radiol. 1987; 10:280-284 [DOI] [PubMed] [Google Scholar]
- 33. Steinke W, Hennerici M, Aulich A. Doppler color flow imaging of carotid body tumors. Stroke. 1989; 20:1574-1577 [DOI] [PubMed] [Google Scholar]
- 34. Arslan H, Ünal Ö, Kutluhan A, Sakarya ME. Power Doppler scanning in the diagnosis of carotid body tumors. J Ultrasound Med. 2000; 19:367-370 [DOI] [PubMed] [Google Scholar]
- 35. Stoeckli SJ, Schuknecht B, Alkadhi H, Fisch U. Evaluation of paragangliomas presenting as a cervical mass on color-coded Doppler sonography. Laryngoscope. 2002; 112:143-146 [DOI] [PubMed] [Google Scholar]
- 36. Boedeker CC, Ridder GJ, Schipper J. Paragangliomas of the head and neck: Diagnosis and treatment. Fam Cancer. 2005; 4:55-59 [DOI] [PubMed] [Google Scholar]
- 37. Derchi LE, Serafini G, Rabbia C, De Albertis P, Solbiati L, Candiani F, Musante F, Bertoglio C, Rizzatto G. Carotid body tumors: US evaluation. Radiology. 1992; 182:457-459 [DOI] [PubMed] [Google Scholar]
- 38. Worsey MJ, Laborde AL, Bower T, Miller E, Kresowik TF, Sharp WJ, Corson JD. An evaluation of color duplex scanning in the primary diagnosis and management of carotid body tumors. Ann Vasc Surg. 1992; 6:90-94 [DOI] [PubMed] [Google Scholar]
- 39. White G, Forbes M, Busch K, Harris JP, Makeham V. Carotid body tumour or not. Ultrasound diagnostic features. In: Vascular 2007 Conference Handbook & Book of Abstracts. Melbourne, Australia, 2007: p. 72 [Google Scholar]


