Abstract
There are many medical conditions like osteoporosis, tumor, or osteonecrosis that weaken the structural strength of the vertebral body and prone it to fracture. Percutaneous vertebral augmentation that is usually applied by polymethylmethacrylate is a relatively safe, effective, and long lasting procedure commonly performed in these situations. In this paper, we updated a review of biomechanics, indications, contraindications, surgical techniques, complications, and overall prognosis of these minimally invasive spinal procedures.
1. Introduction
There are many factors throughout the human life that pathologically weaken the structural strength of the vertebrae and put them at the risk of fracture. Undoubtedly, osteoporosis comprises the most common cause of this weakness and fragility [1]. With an aging population, the prevalence of osteoporotic compression fractures (OCFs) is also increasing.
Since osteoporosis is a contraindication for internal fixation, another solution easily applicable to elderly patients should be employed. The idea of strengthening the weakened vertebral body (VB) was initially raised by Galibert et al. in 1987 [2]. They treated an aggressive vertebral hemangioma at C2 by injecting polymethylmethacrylate (PMMA) into the involved bone. This percutaneous procedure caused almost immediate pain relief. From then onwards, vertebral augmentation is commonly used in the clinical treatment of the patients in need. In this updated review, we briefly discussed the clinical indication, contraindications, surgical techniques, efficacy, and complications of the various methods of vertebral augmentation.
2. Clinical Indications
Clinically any pathologic process that reduces the strength of the VB can inevitably increase the fracture risk. These underlying factors may systemically weaken the bone throughout the body or act locally. Osteoporosis is the most common systemic disease that may present with pathologic vertebral fracture. Osteoporosis may be primary or secondary. Primary osteoporosis mainly occurs in postmenopausal women, but many OCFs happen in the patients with osteoporosis secondary to long-term steroid consumption such as the patients with cancer, collagen vascular diseases, transplant therapy, severe allergy, or asthma [3]. The majority of osteoporotic compression fractures will heal with conservative treatment. The typical indication for vertebral body augmentation (vertebroplasty: VP or kyphoplasty: KP) in OCF is refractory local back pain that is related to the fractured VB and not responding to standard medical treatment for 4 to 12 weeks [4, 5].
Vertebral body augmentation has also been used successfully in surgical treatment of acute unstable thoracolumbar burst fractures in otherwise healthy adults [6]. Perfect reduction can be achieved and maintained by careful prone positioning of the patient, short segment pedicular screw fixation, and transpedicular balloon kyphoplasty with calcium phosphate bone cement. This 360° stabilization leads to low rate of implant failure and loss of correction.
Neoplastic lesions comprise one of the other appropriate applications of cement augmentation. The most common neoplastic osteolytic lesions that may present with impending or pathologic fracture and respond well to vertebral augmentation comprise myeloma, metastatic carcinoma (breast cancer, lung cancer, renal cell carcinoma, thyroid cell carcinoma, etc.), benign aggressive tumors like aggressive hemangioma (Figure 1), and etcetera. If underlying pathology is in doubt, bone biopsy can be carried out prior to or accompany the vertebroplasty. The third and last indication of vertebral augmentation is a painful vertebral fracture associated with osteonecrosis [7].
Figure 1.

A 32-year-old woman presented with chronic unremitting neck pain. Aggressive hemangioma of C6 vertebra was verified on imaging scans. She was treated with anterior percutaneous vertebroplasty.
3. Who Benefits More from Vertebral Augmentation?
Undoubtedly, vertebral augmentation is not the first step in the treatment of OCF. The patient who presented with acute OCF (<5 days) without neurologic deficit but is associated with correlating clinical signs and symptoms should be treated conservatively (calcitonin for 4 weeks) [8]. Current literature is unable to strongly recommend for or against bed rest, the use of opioids/analgesics, brace, exercise program (supervised or unsupervised), or electrical stimulation for these cases [9–11]. Medical treatment with ibandronate and strontium ranelate is an option to prevent additional symptomatic vertebral fracture [12, 13].
According to Nieuwenhuijse, the appropriate time for vertebral augmentation in symptomatic OCFs is between two and twelve months after the onset of complaints [14]. In performing vertebral augmentation, it is important to determine that the affected vertebra is the main culprit of the story. Evidence to support this includes local vertebral pain aroused by tapping, high signal intensity on fat suppression magnetic resonance imaging (MRI) scan, and increased uptake in osteoscintigraphy [15]. Increased uptake in osteoscintigraphy is usually observed for two years after the fracture occurs. Due to the difficulty in evaluating images and the considerable costs, it has been recommended that this modality is better to be taken only in lesions that are difficult to identify with MRI [16]. Among these positive predicting factors to VP, concordance of the clinical (localized pain) and imaging findings (bone marrow edema) is the most important [17]. Additionally, a patient with persistent and severe focal back pain related to less than 4 OCFs benefits more from these procedures [18].
4. Contraindications
Vertebral augmentation procedures require needling in a prone posture for about one hour on average. Any patient with acute OCF, improvement of symptoms with conservative treatment, asymptomatic VB fracture, tumor mass with spinal canal involvement, presence of osteoblastic metastasis, pregnancy, concomitant uncorrectable coagulopathy, severe cardiorespiratory disease, cement allergy, flexion-distraction or fracture-dislocation injury, and systemic and especially local infection is not a good surgical candidate [19–21]. It is understandable that some challenging situations such as pedicle or posterior VB fracture, vertebra plana with severe vertebral collapse (more than one-third of the original VB height), spinal cord compression, or osteosclerosis of VB trabeculae may increase the complications or hamper needling [19]. Usually, due to unknown natural history of PMMA, vertebral augmentation is not routinely recommended in the patients less than 40 years old [18].
5. Surgical Technique
5.1. Vertebroplasty
Percutaneous vertebroplasty is the injection of PMMA or bone substitute (like calcium phosphate) into the weakened VB bone. After the local, regional, or general anesthesia was inducted, the patient transferred to the prone position. In this position, a very gentle trunk hyperextension force might be so effective in restoring anterior VB height. However, this maneuver in osteoporotic patients should be performed with caution and with a little force. A high quality biplanar fluoroscopy and proper cement opacification are two most important prerequisites for safe and triumphant VP.
Percutaneous needle insertion can be approached anteriorly (in cervical spine) or posteriorly (in thoracic and lumbar spine). Posterior approaches can be applied unilaterally/bilaterally or transpedicularly/extrapedicularly (Figure 2). In posterior approaches for accurate transpedicular needle placement, the surgeon should check the position of the cannular tip relative to the pedicular ring on anteroposterior fluoroscopic projections. When the cannular tip came into contact with the bone of the posterior vertebral element, the tip should be located at 2 and 10 o'clock in left and right pedicular rings, respectively (Figure 3).
Figure 2.
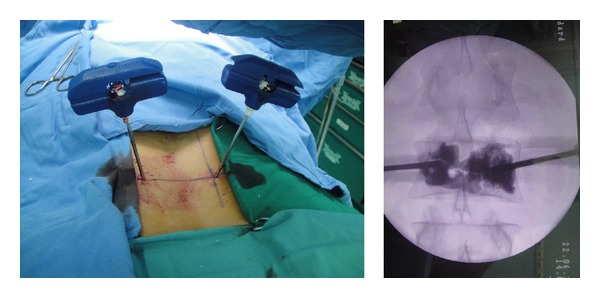
Bipedicular approach in VP. Note the relatively homogenous distribution of the cement through the VB.
Figure 3.
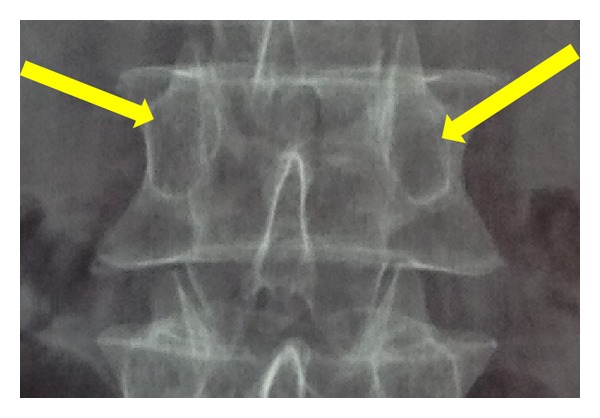
Arrows show the position of the tip of the cannula and also needle trajectory on anteroposterior view, when the cannula came into contact with posterior elements of the vertebra.
When the tip of the cannula passed the junction of middle and anterior third of the VB, 1–4 cc runny cement per side (in bilateral cases) under a relatively high pressure is injected into the weakened VB. This is in contrast with KP that high viscosity cement is injected under less pressure. This difference could explain the higher probability of cement leak in VP versus KP. In VP, high-viscosity PMMA-based cement injection is attempted to be associated with less severe forms of extravasations [22, 23].
On lateral fluoroscopic view, if cement reached the posterior third of the VB, the injection should be stopped to avoid overfilling [24]. It is important to obtain a fairly uniform distribution of cement inside the VB. In some instances this goal could be achieved by only a unilateral approach. Both extrapedicular and transpedicular approaches can be useful in increasing VB strength and stiffness of the involved vertebra but the latter is more capable of restoring VB height due to its easier access to the fracture site [25].
Literature could not find a strong correlation between the injected cement volume and the amount of VB strength and stiffness restoration, and the degree of clinical improvement [26]. It has been reported that as little as 2 mL cement volume injected into the involved vertebra may restore the initial stiffness [27]. Vertebral augmentation aims to inject the minimum amount of cement required to obtain spinal stability; a good central distribution of cement inside the VB with a vertebral body fraction of 24% was proposed as the optimal fraction to be cemented (Figure 4) [28–30].
Figure 4.

An 80-year-old woman with OCF of L2 (vertebra plana). She was treated with bilateral transpedicular VP.
5.2. Kyphoplasty
Usually KP for thoracolumbar vertebra is carried out by bilateral transpedicular approach. Like VP, initial attempt for vertebral closed reduction is carried out by positioning and traction. Vertebral needling is similar to VP but needles should be replaced with larger cannulae to insert bone tamps through them. In KP, the surgeon aims to centrally place one or two bone tamps inside the VB under biplanar fluoroscopic control.
First, bone tamps are inflated under manometric control with radio-contrast medium (for visualization of VB expansion). Usually a balloon pressure of 150 to 300 psi is necessary to reduce OCF. If the procedure is carried out within 3 months of the OCF, usually it is possible to restore 30 to 50% of the primary VB height. Then, balloons are deflated and 3.5 to 8.5 cc of high viscosity cement (with a tooth-paste-like viscosity) under direct image control is injected into the volume previously created by bone tamps (Figure 5) [31]. It should be noted that some authors use a dilator device instead of balloon to expand the collapsed vertebra [32].
Figure 5.
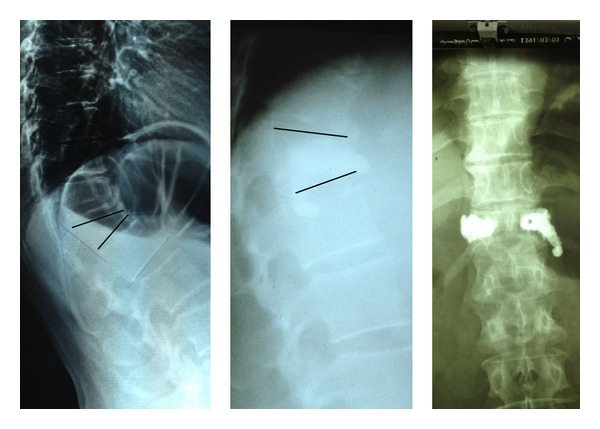
Percutaneous kyphoplasty in a 50-year-old female. Note that cement extravasated into the paravertebral space.
6. Complications
Like any other surgical procedure, VB augmentations do have some complications. Perhaps, cement leakage constitutes the most common complication of these minimally invasive procedures (27 to 75%) [23, 33, 34]. Fortunately, most of the cement extravasation phenomena are clinically asymptomatic. Cement may leak into the intervertebral disc space (most common), anterior paravertebral area, throughout the needle tract, venous system, intervertebral foramen, or even epidural space (spinal canal) [35–38]. The presence of intravertebral cleft increases the prevalence of complications related to cement extravasation [39]. In the patients with osteolytic tumoral fractures, due to increased possibility of posterior vertebral body fracture, augmentation may be associated with an increased rate of leakage and less predictable pain relief [38]. Central pulmonary cement embolism has also been reported [40]. Factors that have been cited to reduce the possibility of cement leakage during VP include precise needling, sufficient cement visibility, low pressure cement injection, and continuous fluoroscopic monitoring during cement injection [41].
VB augmentation changes the density and loading behavior of the vertebrae and this may cause an increased risk of adjacent vertebral fracture. Many of these osteoporotic patients do fracture more even without any augmentation procedures. Will VB augmentation procedures increase the incidence of subsequent vertebral fracture? It is not proven, currently. Theoretically, excessive filling and augmentation of the VB increase the stress applied to the adjacent osteoporotic vertebra and may cause a following fracture [42]. The majority of the following fractures occur at the adjacent vertebrae and within the first three months of augmentation [43]. It is observed that adjacent vertebral fractures more commonly occur in the patients with previous cement leakage into the disc space. Meanwhile, the effects of supplementary antiosteoporotic drugs on the future fracture risk should not be ignored. Other complications sometimes reported include infection and rib fractures. In KP, rupture of the bone tamp also rarely occurs and usually does not carry any adverse effect.
7. Surgical Outcome
It has been verified by numerous studies that VB augmentation procedures in the treatment of chronic OVFs are associated with an immediate, significant, and long acting (>6 months) improvement in back pain and quality of life [16, 44, 45]. In a literature review on efficacy of vertebral augmentation that was carried out by Garfin and Reilley, they also confirmed that both VP and KP have significant effect on pain and function improvement [46]. In comparing VP with KP in the patients with OCF, the results showed that both modalities offer comparable therapeutic effects on pain reduction and disability improvement, although cement leakage prevention and VB height restoration are more pleasant in KP patients [47–49].
In treatment of OCFs, both VP and KP can be effective in restoring anterior VB height [50]. The prone positioning itself has an important role in height restoration. VP also has a safe and beneficial effect on pain and functional status in the patients with spinal tumors or tumor induced VB fractures [51–53].
8. Alternatives to Bone Cement in Vertebral Augmentation
Serious complications of cement augmentation including extravasation with its potential neurovascular disastrous effects and uncertain fate of PMMA in the body have led the researchers to consider alternative materials. For example, a transpedicle body augmenter that is a porous titanium spacer has been invented as an internal support to reconstruct the VB [54].
Various materials have been introduced to substitute bone cement in vertebral augmentation procedures. These materials have some degrees of cement properties including good biocompatibility, radio-opacity, and biomechanical strength and stiffness. Some of these materials like composite resin materials, calcium sulfate, or calcium phosphate have passed their experimental stages and are now available clinically [55, 56]. Biomechanically, it has been tested that VB augmentation with calcium phosphate can be effective clinically as well as PMMA in the treatment of OCFs. Due to the fear of uncertain fate of PMMA especially in the young patients, this substance can be an acceptable alternative [57].
9. Conclusion
Procedures involving percutaneous vertebral body augmentation are minimally invasive, effective, and long lasting procedures that should be used in properly indicated and selected patients and by experienced and well-educated physicians. Numerous complications are possible but clinically asymptomatic in most patients. Serious neurologic complications are rare but probable; therefore these procedures should be only performed in those well-equipped spinal centers in which emergent neurological decompression is accessible.
Acknowledgment
The author thanks Dr. Hasankhani EG for reviewing the text and providing useful annotations.
Conflict of Interests
The author declares that there is no conflict of interests regarding the publication of this paper.
References
- 1.Romagnoli E, de Geronimo S, Pepe J, et al. Clinical aspects of osteoporosis. Recenti Progressi in Medicina. 2002;93(9):484–488. [PubMed] [Google Scholar]
- 2.Galibert P, Deramond H, Rosat P, le Gars D. Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neurochirurgie. 1987;33(2):166–168. [PubMed] [Google Scholar]
- 3.Kirchgatterer A, Aschl G, Knoflach P. Steroid-induzierte osteoporose: pathogenese und therapeutische konsequenzen. Acta Medica Austriaca. 2000;27(1):23–26. doi: 10.1046/j.1563-2571.2000.200105.x. [DOI] [PubMed] [Google Scholar]
- 4.McGirt MJ, Parker SL, Wolinsky J-P, Witham TF, Bydon A, Gokaslan ZL. Vertebroplasty and kyphoplasty for the treatment of vertebral compression fractures: an evidenced-based review of the literature. Spine Journal. 2009;9(6):501–508. doi: 10.1016/j.spinee.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 5.Rousing R, Hansen KL, Andersen MO, Jespersen SM, Thomsen K, Lauritsen JM. Twelve-months follow-up in forty-nine patients with acute/semiacute osteoporotic vertebral fractures treated conservatively or with percutaneous vertebroplasty: a clinical randomized study. Spine. 2010;35(5):478–482. doi: 10.1097/BRS.0b013e3181b71bd1. [DOI] [PubMed] [Google Scholar]
- 6.Marco RAW, Kushwaha VP. Thoracolumbar burst fractures treated with posterior decompression and pedicle screw instrumentation supplemented with balloon-assisted vertebroplasty and calcium phosphate reconstruction. The Journal of Bone and Joint Surgery. American. 2009;91(1):20–28. doi: 10.2106/JBJS.G.01668. [DOI] [PubMed] [Google Scholar]
- 7.McGraw JK, Cardella J, Barr JD, et al. Society of interventional radiology quality improvement guidelines for percutaneous vertebroplasty. Journal of Vascular and Interventional Radiology. 2003;14(7):827–831. doi: 10.1016/s1051-0443(07)60242-5. [DOI] [PubMed] [Google Scholar]
- 8.Papadokostakis G, Damilakis J, Mantzouranis E, Katonis P, Hadjipavlou A. The effectiveness of calcitonin on chronic back pain and daily activities in postmenopausal women with osteoporosis. European Spine Journal. 2006;15(3):356–362. doi: 10.1007/s00586-005-0916-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pfeifer M, Begerow B, Minne HW. Effects of a new spinal orthosis on posture, trunk strength, and quality of life in women with postmenopausal osteoporosis: a randomized trial. American Journal of Physical Medicine and Rehabilitation. 2004;83(3):177–186. doi: 10.1097/01.phm.0000113403.16617.93. [DOI] [PubMed] [Google Scholar]
- 10.Papaioannou A, Adachi JD, Winegard K, et al. Efficacy of home-based exercise for improving quality of life among elderly women with symptomatic osteoporosis-related vertebral fractures. Osteoporosis International. 2003;14(8):677–682. doi: 10.1007/s00198-003-1423-2. [DOI] [PubMed] [Google Scholar]
- 11.Rossini M, Viapiana O, Gatti D, de Terlizzi F, Adami S. Capacitively coupled electric field for pain relief in patients with vertebral fractures and chronic pain. Clinical Orthopaedics and Related Research. 2010;468(3):735–740. doi: 10.1007/s11999-009-1088-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chesnut CH, III, Skag A, Christiansen C, et al. Effects of oral ibandronate administered daily or intermittently on fracture risk in postmenopausal osteoporosis. Journal of Bone and Mineral Research. 2004;19(8):1241–1249. doi: 10.1359/JBMR.040325. [DOI] [PubMed] [Google Scholar]
- 13.Meunier PJ, Roux C, Seeman E, et al. The effects of strontium ranelate on the risk of vertebral fracture in women with postmenopausal osteoporosis. The New England Journal of Medicine. 2004;350(5):459–468. doi: 10.1056/NEJMoa022436. [DOI] [PubMed] [Google Scholar]
- 14.Nieuwenhuijse MJ, van Erkel AR, Dijkstra PD. Percutaneous vertebroplasty for subacute and chronic painful osteoporotic vertebral compression fractures can safely be undertaken in the first year after the onset of symptoms. The Journal of Bone and Joint Surgery. British. 2012;94(6):815–820. doi: 10.1302/0301-620X.94B6.28368. [DOI] [PubMed] [Google Scholar]
- 15.Maynard AS, Jensen ME, Schweickert PA, Marx WF, Short JG, Kallmes DF. Value of bone scan imaging in predicting pain relief percutaneous vertebroplasty in osteoporotic vertebral fractures. American Journal of Neuroradiology. 2000;21(10):1807–1812. [PMC free article] [PubMed] [Google Scholar]
- 16.Kawanishi M, Morimoto A, Okuda Y, et al. Percutaneous vertebroplasty for vertebral compression fracture: indication, technique, and review of the literature. Neurosurgery Quarterly. 2005;15(3):172–177. [Google Scholar]
- 17.Caudana R, Renzi Brivio L, Ventura L, Aitini E, Rozzanigo U, Barai G. CT-guided percutaneous vertebroplasty: personal experience in the treatment of osteoporotic fractures and dorsolumbar metastases. Radiologia Medica. 2008;113(1):114–133. doi: 10.1007/s11547-008-0230-1. [DOI] [PubMed] [Google Scholar]
- 18.Linville DA., II Vertebroplasty and kyphoplasty. Southern Medical Journal. 2002;95(6):583–587. [PubMed] [Google Scholar]
- 19.Serra L, Kermani FM, Panagiotopoulos K, de Rosa V, Vizioli L. Vertebroplasty in the treatment of osteoporotic vertebral fractures: results and functional outcome in a series of 175 consecutive patients. Minimally Invasive Neurosurgery. 2007;50(1):12–17. doi: 10.1055/s-2006-947994. [DOI] [PubMed] [Google Scholar]
- 20.Denaro L, Longo UG, Denaro V. Vertebroplasty and kyphoplasty: reasons for concern? Orthopedic Clinics of North America. 2009;40(4):465–471. doi: 10.1016/j.ocl.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 21.McGuire R. AAOS clinical practice guideline: the treatment of symptomatic osteoporotic spinal compression fractures. Journal of the American Academy of Orthopaedic Surgeons. 2011;19(3):183–184. doi: 10.5435/00124635-201103000-00008. [DOI] [PubMed] [Google Scholar]
- 22.Lador R, Liberman S, Ben-Galim P, Dreiangel N, Reitman CA, Hipp JA. A cadaver study to compare vertebral augmentation with a high-viscosity cement to augmentation with conventional lower-viscosity cement. Journal of Spinal Disorders and Techniques. 2013;26(2):68–73. doi: 10.1097/BSD.0b013e3182337d69. [DOI] [PubMed] [Google Scholar]
- 23.Georgy BA. Clinical experience with high-viscosity cements for percutaneous vertebral body augmentation: occurrence, degree, and location of cement leakage compared with kyphoplasty. American Journal of Neuroradiology. 2010;31(3):504–508. doi: 10.3174/ajnr.A1861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mehbod A, Aunoble S, le Huec JC. Vertebroplasty for osteoporotic spine fracture: prevention and treatment. European Spine Journal. 2003;12(supplement 2):S155–S162. doi: 10.1007/s00586-003-0607-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Erkan S, Wu C, Mehbod AA, Cho W, Transfeldt EE. Biomechanical comparison of transpedicular versus extrapedicular vertebroplasty using polymethylmethacrylate. Journal of Spinal Disorders and Techniques. 2010;23(3):180–185. doi: 10.1097/BSD.0b013e31819c48a4. [DOI] [PubMed] [Google Scholar]
- 26.Kim AK, Jensen ME, Dion JE, Schweickert PA, Kaufmann TJ, Kallmes DF. Unilateral transpedicular percutaneous vertebroplasty: initial experience. Radiology. 2002;222(3):737–741. doi: 10.1148/radiol.2223010718. [DOI] [PubMed] [Google Scholar]
- 27.Molloy S, Mathis JM, Belkoff SM. The effect of vertebral body percentage fill on mechanical behavior during percutaneous vertebroplasty. Spine. 2003;28(14):1549–1554. [PubMed] [Google Scholar]
- 28.Nieuwenhuijse MJ, Bollen L, van Erkel AR, Dijkstra PDS. The optimal intravertebral cement volume in percutaneous vertebroplasty for painful osteoporotic vertebral compression fractures. Spine. 2012;37(20):1747–1755. doi: 10.1097/BRS.0b013e318254871c. [DOI] [PubMed] [Google Scholar]
- 29.Mousavi P, Roth S, Finkelstein J, Cheung G, Whyne CM. Volumetric quantification of cement leakage following percutaneous vertebroplasty in metastatic and osteoporotic vertebrae. Journal of Neurosurgery. 2003;99(1, supplement):56–59. doi: 10.3171/spi.2003.99.1.0056. [DOI] [PubMed] [Google Scholar]
- 30.Pizzoli AL, Brivio LR, Caudana R, Vittorini E. Percutaneous CT-guided vertebroplasty in the management of osteoporotic fractures and dorsolumbar metastases. Orthopedic Clinics of North America. 2009;40(4):449–458. doi: 10.1016/j.ocl.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 31.Robinson Y, Heyde CE, Försth P, Olerud C. Kyphoplasty in osteoporotic vertebral compression fractures—guidelines and technical considerations. Journal of Orthopaedic Surgery and Research. 2011;6(1, article 43) doi: 10.1186/1749-799X-6-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shen GW, Wu NQ, Zhang NP, Jin ZS, Xu J, Yin GY. A prospective comparative study of kyphoplasty using the Jack vertebral dilator and balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures. The Journal of Bone and Joint Surgery. British. 2010;92(9):1282–1288. doi: 10.1302/0301-620X.92B9.23739. [DOI] [PubMed] [Google Scholar]
- 33.la Maida GA, Giarratana LS, Acerbi A, Ferrari V, Mineo GV, Misaggi B. Cement leakage: safety of minimally invasive surgical techniques in the treatment of multiple myeloma vertebral lesions. European Spine Journal. 2012;21(supplement 1):S61–S68. doi: 10.1007/s00586-012-2221-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nieuwenhuijse MJ, van Erkel AR, Dijkstra PDS. Cement leakage in percutaneous vertebroplasty for osteoporotic vertebral compression fractures: identification of risk factors. Spine Journal. 2011;11(9):839–848. doi: 10.1016/j.spinee.2011.07.027. [DOI] [PubMed] [Google Scholar]
- 35.Lotfinia I, Sayyahmelli S. Complications of percutaneous vertebroplasty: a clinical study and literature review. Neurosurgery Quarterly. 2010;20(4):241–246. [Google Scholar]
- 36.Kao F-C, Tu Y-K, Lai P-L, Yu S-W, Yen C-Y, Chou M-C. Inferior vena cava syndrome following percutaneous vertebroplasty with polymethylmethacrylate. Spine. 2008;33(10):E329–E333. doi: 10.1097/BRS.0b013e31816f6a10. [DOI] [PubMed] [Google Scholar]
- 37.Harrington KD. Major neurological complications following percutaneous vertebroplasty with polymethylmethacrylate: a case report. The Journal of Bone and Joint Surgery. American. 2001;83(7):1070–1073. doi: 10.2106/00004623-200107000-00014. [DOI] [PubMed] [Google Scholar]
- 38.Omidi-Kashani F, Ebrahimzadeh M, Peivandy M. Late onset sciatalgia as a rare complication of percutaneous vertebroplasty; a case report. Cases Journal. 2009;2(8, article 7960) doi: 10.4076/1757-1626-2-7960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ha K-Y, Lee J-S, Kim K-W, Chon J-S. Percutaneous vertebroplasty for vertebral compression fractures with and without intravertebral clefts. The Journal of Bone and Joint Surgery. British. 2006;88(5):629–633. doi: 10.1302/0301-620X.88B5.17345. [DOI] [PubMed] [Google Scholar]
- 40.François K, Taeymans Y, Poffyn B, van Nooten G. Successful management of a large pulmonary cement embolus after percutaneous vertebroplasty: a case report. Spine. 2003;28(20):E424–E425. doi: 10.1097/01.BRS.0000092345.00563.E0. [DOI] [PubMed] [Google Scholar]
- 41.Gilula L. Is insufficient use of polymethylmethacrylate a cause for vertebroplasty failure necessitating repeat vertebroplasty? American Journal of Neuroradiology. 2003;24(10):2120–2122. [PMC free article] [PubMed] [Google Scholar]
- 42.Ahn Y, Lee JH, Lee H-Y, Lee S-H, Keem S-H. Predictive factors for subsequent vertebral fracture after percutaneous vertebroplasty. Journal of Neurosurgery: Spine. 2008;9(2):129–136. doi: 10.3171/SPI/2008/9/8/129. [DOI] [PubMed] [Google Scholar]
- 43.Li Y-A, Lin C-L, Chang M-C, Liu C-L, Chen T-H, Lai S-C. Subsequent vertebral fracture after vertebroplasty: incidence and analysis of risk factors. Spine. 2012;37(3):179–183. doi: 10.1097/BRS.0b013e3181f72b05. [DOI] [PubMed] [Google Scholar]
- 44.Muijs SPJ, Nieuwenhuijse MJ, van Erkel AR, Dijkstra PDS. Percutaneous vertebroplasty for the treatment of osteoporotic vertebral compression fractures: evaluation after 36 months. The Journal of Bone and Joint Surgery. British. 2009;91(3):379–384. doi: 10.1302/0301-620X.91B3.20970. [DOI] [PubMed] [Google Scholar]
- 45.McKiernan F, Faciszewski T, Jensen R. Quality of life following vertebroplasty. The Journal of Bone and Joint Surgery. American. 2004;86(12):2600–2606. doi: 10.2106/00004623-200412000-00003. [DOI] [PubMed] [Google Scholar]
- 46.Garfin SR, Reilley MA. Minimally invasive treatment of osteoporotic vertebral body compression fractures. Spine Journal. 2002;2(1):76–80. doi: 10.1016/s1529-9430(01)00166-8. [DOI] [PubMed] [Google Scholar]
- 47.de Negri P, Tirri T, Paternoster G, Modano P. Treatment of painful osteoporotic or traumatic vertebral compression fractures by percutaneous vertebral augmentation procedures: a nonrandomized comparison between vertebroplasty and kyphoplasty. Clinical Journal of Pain. 2007;23(5):425–430. doi: 10.1097/AJP.0b013e31805593be. [DOI] [PubMed] [Google Scholar]
- 48.Omidi-Kashani F, Samini F, Hasankhani EG, Kachooei AR, Toosi KZ, Golhasani-Keshtan F. Does percutaneous kyphoplasty have better functional outcome than vertebroplasty in single level osteoporotic compression fractures? A comparative prospective study. Journal of Osteoporosis. 2013;2013:5 pages. doi: 10.1155/2013/690329.690329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kim K-H, Kuh S-U, Chin D-K, et al. Kyphoplasty versus vertebroplasty: restoration of vertebral body height and correction of kyphotic deformity with special attention to the shape of the fractured vertebrae. Journal of Spinal Disorders & Techniques. 2012;25(6):338–344. doi: 10.1097/BSD.0b013e318224a6e6. [DOI] [PubMed] [Google Scholar]
- 50.Teng MMH, Wei C-J, Wei L-C, et al. Kyphosis correction and height restoration effects of percutaneous vertebroplasty. American Journal of Neuroradiology. 2003;24(9):1893–1900. [PMC free article] [PubMed] [Google Scholar]
- 51.Alvarez L, Pérez-Higueras A, Quiñones D, Calvo E, Rossi RE. Vertebroplasty in the treatment of vertebral tumors: postprocedural outcome and quality of life. European Spine Journal. 2003;12(4):356–360. doi: 10.1007/s00586-003-0525-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fourney DR, Schomer DF, Nader R, et al. Percutaneous vertebroplasty and kyphoplasty for painful vertebral body fractures in cancer patients. Journal of Neurosurgery. 2003;98(1):21–30. doi: 10.3171/spi.2003.98.1.0021. [DOI] [PubMed] [Google Scholar]
- 53.Omidi-Kashani F, Hasankhani EG, Akhlaghi S, Golhasani-Keshtan F, Toosi KZ. Percutaneous vertebroplasty in symptomatic hemangioma versus osteoporotic compression fracture. Indian Journal of Orthopaedics. 2013;47(3):234–237. doi: 10.4103/0019-5413.111498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Li K-C, Li AF-Y, Hsieh C-H, Chen H-H. Transpedicle body augmenter in painful osteoporotic compression fractures. European Spine Journal. 2007;16(5):589–598. doi: 10.1007/s00586-006-0197-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lieberman IH, Togawa D, Kayanja MM. Vertebroplasty and kyphoplasty: filler materials. Spine Journal. 2005;5(6, supplement):305S–316S. doi: 10.1016/j.spinee.2005.02.020. [DOI] [PubMed] [Google Scholar]
- 56.Wu X-T, Jiang X-J, Zhang S-D, Yang H-L. Biomechanical evaluation of vertebroplasty using calcium sulfate cement for thoracolumbar burst fractures. Chinese Journal of Traumatology. 2007;10(6):327–333. [PubMed] [Google Scholar]
- 57.Tomita S, Kin A, Yazu M, Abe M. Biomechanical evaluation of kyphoplasty and vertebroplasty with calcium phosphate cement in a simulated osteoporotic compression fracture. Journal of Orthopaedic Science. 2003;8(2):192–197. doi: 10.1007/s007760300032. [DOI] [PubMed] [Google Scholar]


