Figure 2.
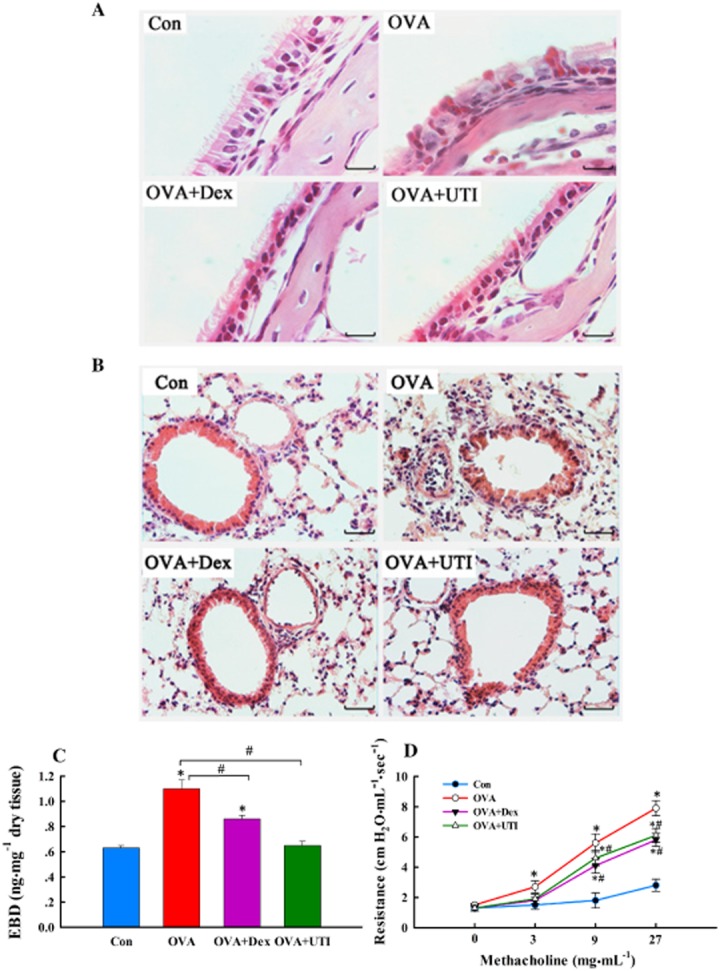
UTI ameliorates OVA sensitization and challenge-induced pathologies and improves lung function. At 24 h after final OVA challenge, paraffin-embedded sections of nasal mucosa and lungs were stained with haematoxylin and eosin (H&E); lung endothelial permeability measured and airway reactivity to methacholine were also assessed. (A) Representative H&E staining images of nasal mucosa sections. Section from sensitized and challenged mice (OVA) exhibited increased inflammatory cell infiltration, epithelial derangement, epithelial deciliation and goblet cell hypertrophy. These histological changes were not obvious in sections from OVA + UTI or OVA + Dex groups of mice. Scale bar = 40 μm. (B) Representative H&E staining images of lung sections. Section from OVA-sensitized and challenged mice displayed inflammatory cell infiltration in bronchial and alveolar walls. These histological changes were ameliorated in sections from OVA + UTI or OVA + Dex groups of mice. Scale bar = 20 μm. (C) UTI reduces OVA sensitization and challenge-induced lung endothelial permeability. Lung endothelial permeability, measured using EBD leakage index as an indicator, increased significantly in OVA alone group, which was prevented in OVA + UTI and OVA + Dex group. Means ± SD of 10 mice per group. *P < 0.05, compared with control group. #P < 0.05, compared with OVA alone group. (D) UTI reduces OVA sensitization and challenge-induced airway hyperactivity. Airway reactivity to aerosolized methacholine increased significantly in OVA alone group, which was prevented in OVA + UTI and OVA + Dex group. Means ± SD of five mice per group. *P < 0.05, compared with control group. #P < 0.05, compared with OVA alone group.
