Abstract
Renal abnormalities have been reported to occur in patients with ankylosing spondylitis (AS). This study examined a patient who suffered from AS for two years. The 24-hour urine protein of the patient was 4.80 g/day. The result of renal biopsy showed minimal change. The patient was treated with infliximab. After two months, nephrotic syndrome was treated successfully.
Keywords: Ankylosing spondylitis, nephrotic syndrome, infliximab
Introduction
Ankylosing spondylitis (AS) is a chronic inflammatory disease of the axial skeleton with variable involvement of peripheral joints and non-articular structures. It mainly affects the joints in the spine and in the pelvis (sacroiliac joint), and can cause eventual fusion of the spine. AS is a systemic disease, which means that its symptoms may occur in other parts of the body aside from the joints. It can be accompanied by extraarticular manifestations in the cardiovascular, pulmonary, neurologic, and renal organs. In recent years, AS-related kidney damage has shown increasing importance. Renal abnormalities have been reported to occur in patients with AS. However, no definite treatment exists for this disease.
Case repor
This study reported a case of a patient with AS and minimal renal change, which was successfully treated with infliximab.
The patient was a 21-year-old male who suffered from severe back pains and stiffness in 2010. The pain was accompanied by bilateral groin pain. The pain was severe in the morning and was relieved after doing an activity. Constant stiffness in the back caused the patient to have difficulty in turning over. He attributed the pain to untreated athletic injuries all the time. The pain gradually became more severe, so he went to the hospital in June 2012. The patient had no medical history.
Laboratory examination showed that the erythrocyte sedimentation rate (ESR) was 70 mm/h, human leukocyte antigen (HLA)-B27 was positive, C-reactive protein was 2.75 mg/dL, IgG was 5.25 g/L, IgA was 4.28 g/L, and ALB was 20.7 g/L. The antinuclear antibodies and rheumatoid factor were all negative. Urinalysis showed the presence of proteinuria (++++) without hematuria. In addition, the 24-hour urine protein was 4.80 g/day, serum creatinine was normal, triglyceride was 2.04 mmol/L, cholesterol was 9.06 mmol/L, and uric acid was 523 umol/L. Hepatitis B/C and HIV serology were all negative. Sacroiliac joint CT showed multiple subchondral erosions and sclerosis. No obvious abnormality was shown in urinary system ultrasound. A renal biopsy was performed on July 6, 2012. Glomeruli showed no changes in light microscopy (Figure 1) or immunofluorescence. As observed under an electron microscope, a characteristic fusion of epithelial foot processes occurred (Figure 2). Minimal renal change was noted. The patient was diagnosed with AS with nephrotic syndrome.
Figure 1.
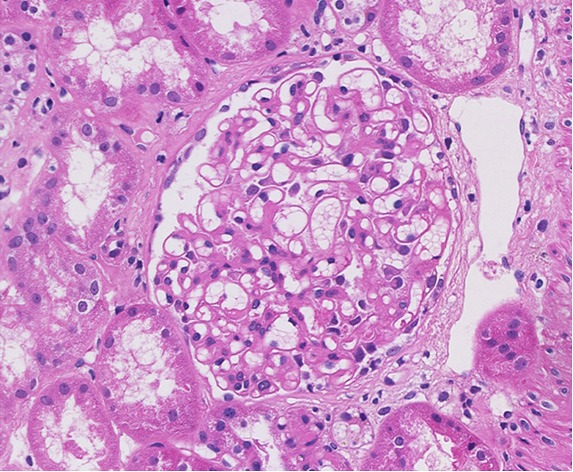
No specific changes observed under a light microscope.
Figure 2.
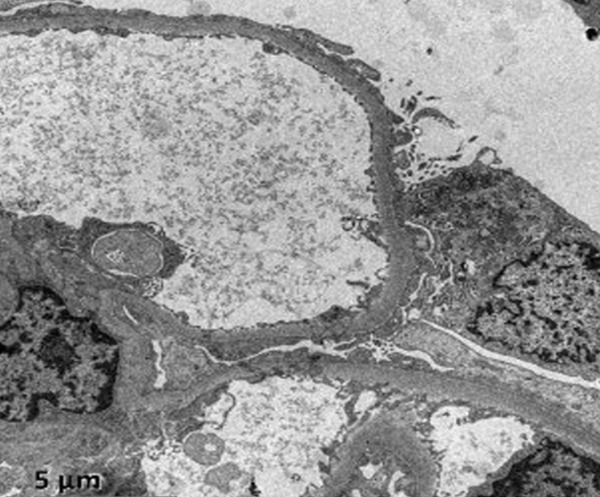
Fusion of epithelial foot processes observed under an electron microscope.
Treatment: the patient was treated initially with infliximab infusions at a dose of 0.2. A dramatic clinical improvement was noted within one week. We wanted to provide the patient with glucocorticoids, but he refused because of concerns about its side effects. We continued the infusions of infliximab (0.2) within two and six weeks.
The follow-up consultation of the patient in September showed that serum albumin returned to normal (30.7 g/L), the 24-hour urine protein was 0.3 g/day, and the ESR was 10 mm/h. These findings indicate a dramatic clinical improvement. Infliximab (0.2) was infused every 8 weeks thereafter. A considerable decline of proteinuria was observed and remission was attained after 18 months.
Discussion
The incidence rate of kidney involvement in AS is approximately 4.3% to 21.4% [1]. Clinical symptoms may include hematuria, proteinuria, tube-type urine, hypertension, and renal insufficiency [2]. In 2012, Samia B retrospectively reviewed the medical records of 32 cases with renal involvement among 212 cases of AS. Results showed the occurrence of microscopic hematuria in 22 patients, proteinuria in 23 patients, nephrotic syndrome in 11 patients, and decreased renal function in 24 patients [3]. In China, Li et al. studied clinical and pathological changes in 18 cases of AS with renal involvement. Results indicated that glomerulonephritis occurred in 9 patients, chronic glomerulonephritis in 5 patients, nephrotic syndrome manifestations in 1 patient, and chronic renal insufficiency in three patients [4].
Pathological changes of AS renal damage may indicate IgA nephropathy, amyloidosis, and drug induced interstitial nephritis. Secondary renal amyloidosis and IgA nephropathy are the most common, whereas mesangial proliferative glomerulonephritis, membranous nephropathy, and focal segmental glomerulosclerosis are relatively rare. In the study conducted by Samia B, the secondary renal amyloidosis in 13 patients correspond to a 6.1% prevalence and the tubulointerstitial nephropathy in 7 patients was the most common cause of renal involvement in AS followed by IgA nephropathy, as exhibited by 4 patients. The pathological condition of the 17 patients evolved to end-stage renal disease after an average period of 29.8 ± 46 months. The pathological type of this case showed minimal change, which had not been reported.
Tumor necrosis factor-alpha (TNF-alpha) is a key in the pathogenesis of AS. A basic study discovered that TNF-alpha is mediated by inflammation and has immunomodulatory effects in the immune response. Infliximab is a chimeric TNF-alpha monoclonal antibody that can combine with TNF-alpha on the cell surface so that TNF-alpha loses its biological activity. Better clinical effect has been attributed to infliximab, which is considered as a significant revolution in the history of AS treatment.
This study revealed that after the patient has been treated with infliximab, his urinary protein was significantly reduced. This finding indicated that anti-TNF-alpha agents were effective. Previous reports have discussed new alternative therapies for renal damage associated with AS. Akdoğan MF [5] reported that a 30-year-old woman was diagnosed with AS. The patient was hospitalized because of massive proteinuria and related symptoms. Nephrotic syndrome was observed and renal biopsy revealed amyloid deposits. After the treatment with infliximab, nephrotic syndrome disappeared.
Aside from being considered as a cure for AS, infliximab also has a therapeutic effect on kidney damage caused by other rheumatic diseases. A recent report stated that renal amyloid, which is secondary to rheumatoid arthritis, can be alleviated by infliximab. Kuroda et al. reported the case of a 55-year-old Japanese woman with reactive AA amyloidosis associated with rheumatoid arthritis. Nephrotic syndrome was observed and renal biopsy specimens revealed amyloidosis deposits. Treatment with infliximab normalized the serum amyloid A protein level, subsequent nephritic syndrome disappeared, and the creatinine clearance improved [6]. Raveh et al. reported that a 13-year-old boy with refractory nephrotic syndrome (minimal change with mesangial proliferation) failed the standard treatment protocols. Some temporary responses to large steroid doses were observed, but even the Mendoza protocol could not induce remission. This case showed the suppression of the proteinuria with infliximab and tapering of steroids [7].
As infliximab is applied increasingly, its side effects should be given attention. One of the serious side effects of infliximab is infection; thus, several patients discontinued infliximab treatment. Infliximab may also cause renal side effects. Chin et al. reported the emergence of membranous nephropathy with nephrotic syndrome in a patient using infliximab [8].
In conclusion, infliximab may be effective in treating renal damage that accompanies AS. Because of its side effects, patients should be selected carefully for anti-TNF-alpha therapy and should be monitored for the effectiveness of the aforementioned therapy, as well as the occurrence of possible side effects.
Disclosure of conflict of interest
None.
References
- 1.Ben Taarit C, Ajlani H, Ben Moussa F, Ben Abdallah T, Ben Maïz H, Khedher A. Renal involvement in ankylosing spondylitis: concerning 210 cases. Rev Med Interne. 2005;26:966–969. doi: 10.1016/j.revmed.2005.07.017. [DOI] [PubMed] [Google Scholar]
- 2.Gupta R, Sharma A, Arora R, Dinda AK, Gupta A, Tiwari SC. Membranous glomerulonephritis in a patient with ankylosing spondylitis: a rare association. Clin Exp Nephrol. 2009;13:667–670. doi: 10.1007/s10157-009-0217-z. [DOI] [PubMed] [Google Scholar]
- 3.Samia B, Hazgui F, Abdelghani KB, Hamida FB, Goucha R, Hedri H, Taarit CB, Maiz HB, Kheder A. Renal abnormalities in ankylosing spondylitis. Nephrol Ther. 2012;8:220–225. doi: 10.1016/j.nephro.2011.10.005. [DOI] [PubMed] [Google Scholar]
- 4.Li D, Pu YC, Zhang C. Clinical and pathological features of ankylosing spondylitis renal damage. Clinical Nephrology. 2010;4:169–172. [Google Scholar]
- 5.Akdoğan MF, Gücün M, Denizli N, Güney M, Akdag I, Ozcan TB, Duranay M. Complete reversal of nephrotic syndrome secondary to amyloidosis with use of infliximab in a patient with inflammatory bowel disease and ankylosing spondylitis. Ren Fail. 2011;33:531–533. doi: 10.3109/0886022X.2011.577543. [DOI] [PubMed] [Google Scholar]
- 6.Kuroda T, Otaki Y, Sato H, Nakatsue T, Murakami S, Sakatsume M, Nakano M, Gejyo F. A case of AA amyloidosis associated with rheumatoid arthritis effectively treated with infliximab. Rheumatol Int. 2008;28:1155–9. doi: 10.1007/s00296-008-0590-z. [DOI] [PubMed] [Google Scholar]
- 7.Raveh D, Shemesh O, Ashkenazi YJ, Winkler R, Barak V. Tumor necrosis factor-alpha blocking agent as a treatment for nephritic syndrome. Pediatr Nephrol. 2004;19:1281–4. doi: 10.1007/s00467-004-1573-2. [DOI] [PubMed] [Google Scholar]
- 8.Chin G, Luxton G, Harvey JM. Infliximab and nephrotic syndrome. Nephrol Dial Transplant. 2005;20:2824–6. doi: 10.1093/ndt/gfi180. [DOI] [PubMed] [Google Scholar]


