Abstract
Background: The increasing use of the transversus abdominis plane (TAP) block, as a form of pain relief after laparoscopic surgery, warrants evaluation of its effectiveness, when compared with other analgesic techniques. Methods: We searched online databases of MEDLINE, EMBASE, Google scholar and The Cochrane Database of Systematic Review. Mean differences (MD) were formulated for continuous data; odds ratios (OR) were calculated for dichotomous data. Results were produced with a random effects model with 95% confidence intervals (CI). Results: 14 trials with a total of 905 patients were included for the analysis, TAP block resulted in significantly less postoperative analgesic consumption at 24 h (MD = -25.46, 95% CI [-32.22, -18.69], P < 0.00001), and less number of patients requiring analgesic postoperatively (OR = 0.16, 95% CI 0.03-0.87, P = 0.03). Meanwhile, pain sores were significantly different at 2 h (MD = -1.55, 95% CI [-2.50, -0.59], P < 0.00001), a borderline difference between the groups seen at 6 hours ( MD = -1.13, 95% CI [-1.69, -0.56], P = 0.05), and there was not affect pain at 24 h (MD = -0.33, 95% CI [-0.08, 0.15], P = 0.14) with TAP block groups compared with the groups without TAP block. There was a significant difference in postoperative nausea and vomiting (random effects model: OR = 2.04, 95% CI [1.19-3.48], P = 0.34). Conclusion: TAP block would result in less analgesic consumption, less requirement of analgesic, and less pain at 2 h and slightly at 6 h but at 24 h after laparoscopic surgery in comparison with usual care alone or placebo block. In addition TAP block can increase the incidence of postoperative nausea and vomiting.
Keywords: TAP block, transversus abdominis plane block, laparoscopic surgery, meta-analysis
Introduction
Nowadays, laparoscopic surgery is a popular method of surgery, with many advantages including reducing analgesic requirement and enhancing patient recovery. Despite the minimally invasive nature, pain can be moderate to severe in the immediate postoperative period [1-4]. The most traditional approach to postoperative pain relief is multimodal using nonsteroidal anti-inflammatory drugs (NSAIDs) and opioids. Nonetheless, there are severe restrictions on the availability of opioids and other essential medications which are used to reduce nausea, vomiting, constipation, urinary retention, respiratory depression and sedation, used for the management of pain [5,6]. Therefore, the use of non-opioid analgesic techniques can lead to an improved quality of recovery for surgical patients [5].
Transversus abdominis plane (TAP) block, a popular analgesic technique since first described by Rafiin in 2001 [7] which may provide up to 24 hours of analgesia, may be an interesting analgesic option for this population after laparoscopic surgery. With the aid of ultrasound (US) or anatomical landmark guidance, local anesthetic is injected into the transversus abdominis fascial plane, where the nerves from T6 to L1 are located [8]. Studies with fresh cadaveric and researches involving healthy volunteers have demonstrated the spread of anaesthetic agent in this plane and the associated block of T8-L1/2 [9].
In the past few years, the use of TAP blocks for pain relief has been increasing for the population after laparoscopic surgery. However, there has been no systematic review evaluating the efficacy of the TAP blocks compared with either placebo or traditional methods of analgesia after laparoscopic surgery. We performed this systematic review and meta-analysis to assess the efficacy of TAP blocks after laparoscopic surgery.
The primary purpose of this meta-analysis is to determine the effect of the TAP block on postoperative opioid consumption and the number requiring opioid after laparoscopic surgery. Secondary aims are to: 1. assess differences in postoperative pain scores at 2 h, 6 h and 24 h by participants having TAP blocks compared with no treatment, placebo and other methods of analgesia; 2. assess differences in the number of nausea or vomiting with TAP blocks after laparoscopic surgery.
Methods
This systematic review and meta-analysis was conducted and reported in agreement with the PRISMA guideline [10].
We searched online databases of MEDLINE (from 1966 to October 2013), EMBASE (from 1982 to October 2013), Google scholar and The Cochrane Database of Systematic Review. Keywords and medical subheadings of “Transversus abdominis plane block OR TAP block” and “laparoscopic surgery or laparoscopic” were used for databases searching. References from relevant articles were reviewed to identify additional studies, and no language restriction was used.
Study selection
Two reviewers (Zhao and Ren) selected eligible RCTs independently. After a primary screening of titles and abstracts, full-text papers of potentially relevant RCTs were retrieved and further evaluated for eligibility. Trials were not relevant based on inclusion and exclusion criteria. Disagreements between two authors were resolved by discussion with a third author (Li).
Inclusion and exclusion criteria
We included trails that met the following criteria: study design is randomized controlled trial (RCT). The populations should have received TAP block undergoing laparoscopic surgery. The outcomes should contain postoperative analgesic use after laparoscopic surgery, the pain scores at different time, the side effects (nausea or vomiting). Excluded were trails reporting administration without an active (placebo or “no treatment” or “TAP block treatment”) control group or not undergoing laparoscopic surgery.
Assessment of study quality
Quality of the reviewed trials was assessed independently by two of the authors (Zhao and Ren) using The Cochrane Risk of Bias tool [11], Disagreement was resolved by discussion or by involving a third review author (Li). The scale evaluates the study for the following items: 1. Sequence generation (checking for possible selection bias); 2. Allocation concealment (checking for possible selection bias); 3. Blinding (checking for possible performance bias); 4. Incomplete outcome data (checking for possible attrition bias through withdrawals, dropouts, protocol deviations); 5. Selective reporting bias; 6. Other sources of bias.
Date extraction
Data were abstracted independently by Zhao and Ren by using a standardized data collection form. The data extracted included author name, publication year, journal, type of surgery, comparator, number of TAP group and control group, analgesic consumption during a given time period (such as 24 hours) after surgery, number requiring analgesic during 24 h after surgery, pain scores at rest or on movement or both , and side effects (nausea or vomiting). If any data were reported in a graph, the authors were contacted, and if the authors did not respond, the reviewers extracted the data from the graph. If medians and ranges were reported means and standard deviations were estimated [12]. Any disagreements surrounding data extraction between two authors were resolved by discussion with a third author (Li).
Statistical analysis
For dichotomous outcomes were evaluated based on event rates using a pooled odds ratio (OR). Continuous variables, a mean difference (MD) accounting for different sample sizes across studies was calculated. The heterogeneity of the included studies was considered significant, if P-value of chisquare test was less than 0.10 or I2 greater than 50%, and then a random-effects model was employed, otherwise a fixed-effects model was used. Further analysis was planned a priori to explore relevant heterogeneity. Subgroup analysis was performed comparing pain scores at rest or on movement in studies. Sensitivity analysis was performed by omitting one study each time and investigating the influence of a single study on the overall pooled estimate. Publication bias was assessed by visually inspecting funnel plots if at least ten trails of each intervention were included. However, we were not able to create funnel plots due to the small of trails in our meta-analysis. A P-value of less than 0.05 was considered statistically significant. All statistical analyses were performed using Review Manager Version 5.1 (RevMan5.1, The Cochrane Collaboration, Oxford, United Kingdom).
Results
Results of the search
The comprehensive search yielded a total of 31 records, and 16 studies initially met the inclusion criteria (Figure 1). 2 studies [25,26] were subsequently excluded for reasons demonstrated in Figure 1. Finally, 14 trials with a total of 905 patients were included for the analysis [3,8,13-24].
Figure 1.
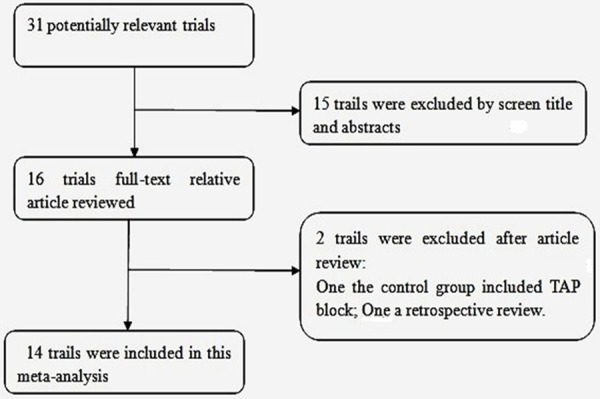
Flow chart outlining retrieved, excluded, and evaluated randomized controlled trials.
Description of studies
The included studies were published between 2009 and 2013, thirteen studies published in English, one in Japanese [24]. Data from 905 patients were analyzed: 488 received TAP blocks or general anesthesia with TAP blocks, 417 received general anesthesia with no treatment, placebo and other methods of analgesia. The characteristics of included studies are listed in Tables 1 and 2. The characteristics included the authors, the year of publication, types of laparoscopic surgery (laparoscopic colorectal resection [13,24], laparoscopic donor nephrectomy [3,15], laparoscopic Gastric-Bypass surgery [16], laparoscopic cholecystectomy [8,17,20,22], laparoscopic hysterectomy [18], laparoscopic appendicectomy [19], outpatient laparoscopy [20]), the total number of control groups versus TAP block groups, postoperative analgesic consumption after laparoscopic surgery, the pain scores at different time (at 2 h, 6 h and 24 h), the side effects (nausea or vomiting) [3,8,13,16,17]. The risk of bias assessment of all included studies is described in Figure 2.
Table 1.
Characteristics of randomized controlled studies
| Author (published year) | Country | Publication | Surgery | Control/TAP block | Number of Control/TAP | analgesic consumption at 24 h | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Control | TAP | ||||||
| Walter Catherine J (2013) | UK | Surg Endosc | laparoscopic colorectal surgery | Non TAP block VS. TAP block | 35/33 | Morphine (mg): 94.2 ± 9.8 | Morphine (mg): 65.3±11.8 |
| Sinha, A (2013) | India | Obesity surgery | Laparoscopic Bariatric Surgery | Control groups VS. TAP block | 50/50 | The number of patients requiring Tramazac hydrochloride: 34/50 | The number of patients requiring Tramazac hydrochloride: 9/50 |
| Parikh, BK (2013) | India | Saudi journal of anaesthesia | laparoscopic donor nephrectomy | TAP block (saline) VS. TAP block | 31/31 | Tramadol (mg): 235.83 ± 47 | Tramadol (mg): 103.83 ± 32.18 |
| Albrecht E (2013) | Canada | Obes Surg | laparoscopic gastric bypass surgery | Non TAP block VS. TAP block | 30/27 | Morphine control (35.6 mg [95% CI, 28.6-42.5]; P = 0.41) groups | morphine TAP (32.2 mg [95% CI, 27.6-36.7]) |
| Petersen, PL (2012) | Denmark | Anesthesia and analgesia | Laparoscopic Cholecystectomy | Placebo blocks VS. bilateral TAP block | 37/37 | Morphine (mg): 12.6 ± 1.5 | Morphine (mg): 12.8 ± 1.5 |
| Ortiz J (2012) | USA | Reg Anesth Pain Med | Laparoscopic Cholecystectomy | Local anesthetic infiltrate VS. bilateral TAP block | 35/39 | Morphine (mg): 15.4 ± 9.2 | Morphine (mg): 16.1 ± 9.9 |
| Kane SM (2012) | USA | Am J Obstet Gynecol | laparoscopic hysterectomy | Non block VS. TAP block | 28/28 | narcotic medication: 7.4 ± 0.4 | narcotic medication: 7.4 ± 0.4 |
| Hosgood SA (2012) | UK | Transplantation | laparoscopic donor nephrectomy | TAP block (saline) VS. TAP block | 22/24 | Morphine (mg): 12.4 ± 8.4 | Morphine (mg): 21.2 ± 14.0 |
| Sandeman DJ (2011) | Australia | Br J Anaesth | laparoscopic appendicectomy | Control groups VS. TAP block | 45/42 | morphine consumption (subjects): 31/45 | morphine consumption (subject) 29/42 |
| RaYoon Suk (2010) | Korea | Korean J Anesthesiol | Laparoscopic Cholecystectomy | Control groups VS. TAP block (B) VS. TAP block (B) | 18/18/18 | The number of patients injected ketorolac 17/18 | The number of patients injected ketorolac: 4/4/18 |
| Conaghan P (2010) | UK | Surg Endosc | laparoscopic colorectal resections | PCA VS. PCA with TAP block | 34/40 | Morphine (mg): 51.8 ± 9.3 | Morphine (mg): 31.3 ± 3.8 |
| El-Dawlatly AA (2009) | Saudi Arabia | Br J Anaesth | Laparoscopic Cholecystectomy | Not TAP block VS. TAP block | 21/21 | Morphine (mg): 22.8 ± 4.3 | Morphine (mg): 10.5 ± 7.7 |
| De Oliveira GS (2011) | USA | Anesth Analg | outpatient laparoscopy | TAP block (saline) VS. TAP VS. TAP block | 23/23/24 | oral morphine (mg): 145.5 ± 8.9 | oral morphine (mg): 65.1 ± 10.2/44.8 ± 18.1 |
| Fujita N (2011) | Japanese | Masui | laparoscopic abdominal surgery | General anesthesia with epidural anesthesia VS. general anesthesia with TAP block | 8/33 | The number of patients requiring NSAIDs: 1/7 | NR |
TAP, transversus abdominal block; PCA, patient-controlled anesthesia; NR, no reported.
Table 2.
Outcome variables in randomized controlled trials
| Author (published year) | Pain Score, Mean ± SD (numbers) | side effect control number/total numberTAP block number/total number | ||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| 2 h | 6 h | 24 h | ||||||
|
| ||||||||
| control | TAP | control | TAP | control | TAP | |||
| Walter Catherine J (2013) | at rest | 3.5 ± 2.2 (32) | 4 ± 3.1 (31) | 3.6 ± 2.6 (31) | 2.9 ± 2.8 (30) | 2.8 ± 2.3 (33) | 3.0 ± 2.3 (33) | nausea or vomiting placebo: 1/34 TAP block: 9/33 |
| on movement | 4.6 ± 2.5 (32) | 4.4 ± 3.0 (31) | 4.1 ± 2.9 (31) | 3.7 ± 2.8 (30) | 3.6 ± 2.7 (33) | 3.7 ± 2.4 (33) | NR | |
| Sinha A (2013) | at rest and on movement | 1.3 ± 1.5 (50) | 1.5 ± 1.8 (50) | 0.5 ± 0.6 (50) | 1.3 ± 1.5 (50) | 0.5 ± 0.6 (50) | 0.5 ± 0.6 (50) | required BIPAP support control group control: 4/31 TAP: 0/31 |
| Parikh BK (2013) | at rest | 2.4 ± 1.5 (31) | 1.0 ± 0.7 (31) | 3.2 ± 1.09 (31) | 1.8 ± 1.05 (31) | 2.3 ± 0.8 (31) | 1.9 ± 0.8 (31) | NR |
| on movement | 4.03 ± 1.6 (31) | 2.1 ± 0.6 (31) | 4.7 ± 1.4 (31) | 3.2 ± 1.4 (31) | 3.8 ± 1.1 (31) | 3.43 ± 0.9 (31) | ||
| Albrecht E (2013) | at rest and on movement | 4.4 ± 0.8 (31) | 4.8 ± 0.7 (31) | 3.5 ± 0.8 (31) | 4.1 ± 0.7 (31) | nausea or vomiting control: 4/30 TAP: 8/27 | ||
| Petersen PL (2012) | at rest | 3.7 ± 1.9 (37) | 3.1 ± 1.8 (37) | 2.1 ± 1.4 (37) | 1.9 ± 1.5 (37) | 1.6 ± 1.6 (37) | 1.5 ± 1.2 (37) | nausea or vomiting control: 13/37 TAP: 8/37 |
| on movement | 5.1 ± 2.4 (37) | 2.9 ± 2.0 (37) | 3.5 ± 1.9 (37) | 2.6 ± 1.9 (37) | 2.5 ± 2.0 (37) | 2.4 ± 1.6 (37) | NR | |
| Ortiz J (2012) | at rest and on movement | 2.17 ± 0.35 (35) | 3.0 ± 0.43 (39) | 3.53 ± 0.47 (35) | 3.05 ± 0.53 (39) | NR | NR | nausea control: 13/35 TAP: 17/39 |
| Kane SM (2012) | at rest and on movement | 2.4 ± 6.6 (28) | 3.0 ± 2.6 (28) | NR | NR | 3.0 ± 2.6 (28) | 2.4 ± 2.1 (28) | NR |
| Hosgood SA (2012) | NR | NR | NR | NR | NR | NR | NR | Nausea and vomiting control: 9/22 TAP: 10/24 |
| Ra Yoon Suk (2010) | at rest and on movement | 6.9 ± 1.57 (18) | 2.6 ± 1.46 (18) | 6.1 ± 1.98 (18) | 1.9v1.43 (18) | 4.4 ± 1.68 (18) | 1.3 ± 0.97 (18) | NR |
TAP, transversus abdominal block; NR, no reported.
Figure 2.
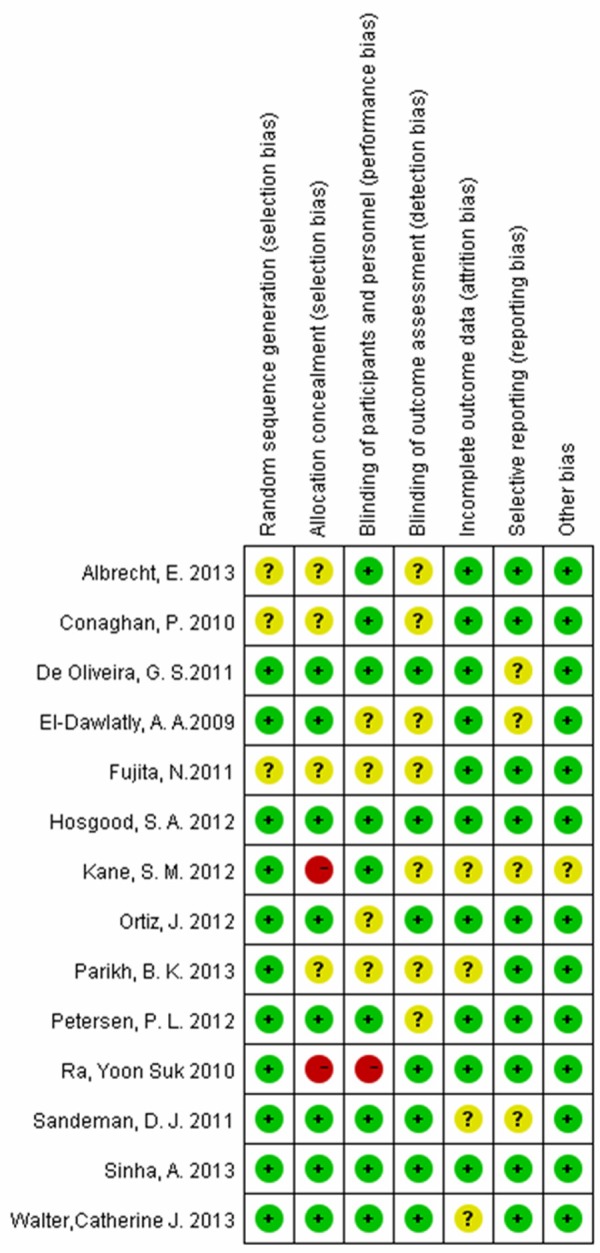
Methodological quality summary: review authors’ judgements about each methodological quality item for each included study.
Primary outcome
Postoperative analgesic consumption
Data on primary outcomes were available in 9 trials [3,8,13,17,18,21,22,23] including 527 patients (271 TAP block; 256 control or placebo), Patients with TAP block required less morphine consumption during 24 hours than those who did not have the block (random effects model: MD = -25.46, 95% CI [-32.22, -18.69], P < 0.00001) (Figure 3). Sensitivity analysis was performed by omitting one study each time, the pooled result was still significant (P < 0.05). Number of patients requiring analgesic postoperatively from 4 trials [14,19,20,24] with TAP block less than those who did not have the block (random effects model: OR = 0.16, 95% CI 0.03-0.87, P = 0.03) (Figure 4).
Figure 3.
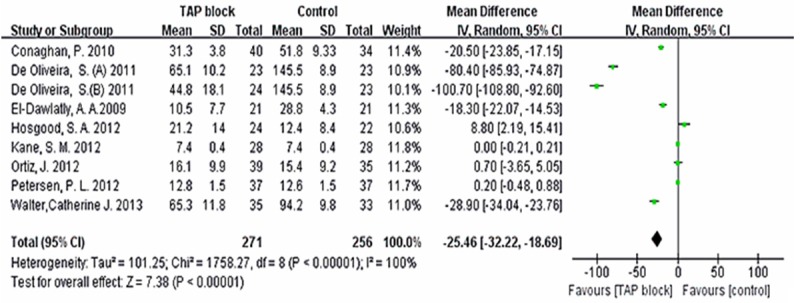
Random effects meta-analysis of mean analgesic consumption at 24 h with and without TAP block after laparoscopic surgery.
Figure 4.
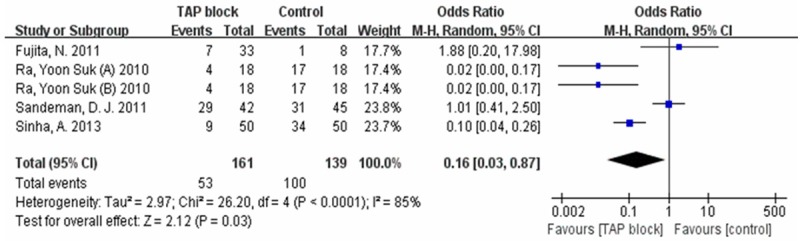
Random effects meta-analysis of the number using analgesic drugs at 24 h with and without TAP block after laparoscopic surgery.
Secondary outcomes
Six studies [8,13-16,18,20] including 647 patients (321 TAP block; 326 control or placebo) reported the pain scores following laparoscopic surgery, however the reporting of pain scores was highly variable, We abstracted the data at 2 h, 6 h, and 24 h with at rest or on movement or both. Postoperative pain scores were significantly reduced with TAP at 2 hour than compared with the group without TAP block (random effects model: MD = -1.55, 95% CI [-2.50, -0.59], P < 0.00001) (Table 3), and a borderline difference between the groups were seen at 6 hours (random effects model: MD = -1.13, 95% CI [-1.69, -0.56], P = 0.05) (Table 3), but was not affect the incidence at 24 h (random effects model: MD = -0.33, 95% CI [-0.08, 0.15], P = 0.14) (Table 3). Subgroup analyses were performed, pain scores at rest or on movement or both at 2 h, 6 h, and 24 h were reported in three, three, and four studies, respectively. Pain scores on movement at 2 h and 6 h were different from pain scores at rest or at rest or on movement (Table 3), and there was no difference at 24 h.
Table 3.
Pooled mean difference and 95% CI for pain scores at difference times
| Pain score | 2 h | 6 h | 24 h | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| Study or subgroup | mean difference | 95%CI | study or subgroup | mean difference | 95% CI | study or subgroup | mean difference | 95% CI | |
| at rest | Parikh BK (R) (2013) | -1.4 | [-1.98, 0.82] | Parikh BK (R) (2013) | -1.4 | [-1.93, -0.87] | Parikh BK (R) (2013) | -0.4 | [-0.8, -0.00] |
| Petersen PL (R) (2012) | -0.6 | [-1.44, 0.24] | Petersen PL (R) (2012) | -0.2 | [-0.86, 0.46] | Petersen PL (R) (2012) | -0.1 | [-0.74, 0.54] | |
| Walter Catherine J (R) (2013) | 0.5 | [-0.83, 1.83] | Walter Catherine J (R) (2013) | -0.7 | [-2.06, 0.66] | Walter Catherine J (R) (2013) | 0.2 | [-0.91, 1.31] | |
| subtotal | -0.64 | [-1.62, 0.34] | subtotal | -0.8 | [-1.68, 0.08] | subtotal | -0.27 | [-0.60, 0.05] | |
| On movement | Parikh BK (M) (2014) | -1.93 | [-2.53, -1.33] | Parikh BK (M) (2014) | -1.5 | [-2.20, -0.80] | Parikh BK (M) (2014) | -0.37 | [-0.87, 0.13] |
| Petersen PL (M) (2013) | -2.2 | [-3.21, -1.19] | Petersen PL (M) (2013) | -0.9 | [-1.77, -0.03] | Petersen PL (M) (2013) | -0.1 | [-0.93, 0.73] | |
| Walter Catherine J (M) (2014) | -0.3 | [-1.67, 1.07] | Walter, Catherine J (M) (2014) | -0.4 | [-1.83, 1.03] | Walter Catherine J (M) (2014) | 0.1 | [-1.13, 1.33] | |
| subtotal | -1.62 | [-2.53, -0.71] | subtotal | -1.13 | [-1.69, -0.56] | subtotal | -0.25 | [-0.66, 0.15] | |
| at rest and on movement | Kane SM (2012) | -4 | [-5.42, -2.58] | Albrecht E (2013) | 0.4 | [0.01, 0.79] | Albrecht E (2013) | 0.6 | [0.21, 0.99] |
| Ra Yoon Suk (2010) | -4.3 | [-5.29, -3.31] | Ra Yoon Suk (2010) | -4.2 | [-5.33, -3.07] | Kane SM (2012) | -0.5 | [-1.92, 0.92] | |
| Sinha A (2013) | 0.2 | [-0.45, 0.85] | Sinha, A (2013) | 0.8 | [0.35, 1.25] | Ra, Yoon Suk (2010) | -3.1 | [-4.0, -2.20] | |
| Sinha A (2013) | 0 | [-0.24, 0.24] | |||||||
| subtotal | -2.67 | [-5.98, 0.64] | subtotal | -0.89 | [-2.71, 0.93] | -0.68 | [-1.79, 0.43] | ||
| total | -1.55 | [-2.50, -0.59] | total | -0.86 | [-1.70, -0.01] | -0.33 | [-0.80, 0.14] | ||
Postoperative nausea and vomiting
There were five trials [3,8,13,16,17] reported the incidence of postoperative nausea and vomiting after laparoscopic surgery including 351 patients (150 TAP block; 151 control or placebo). There was no significant heterogeneityamongst the studies (I2 = 24%, P = 0.26). There were significant differences in postoperative nausea or vomiting between the TAP block groups and without TAP block patients (random effects model: OR = 2.04, 95% CI [1.19-3.48], P = 0.34, Figure 5).
Figure 5.
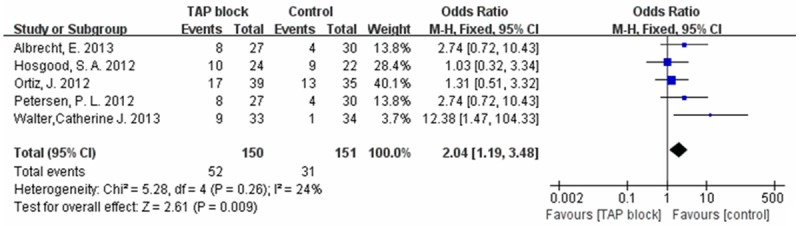
Fixed effects meta-analysis of the incidence of postoperative nausea and vomiting with and without TAP block at 24 h after laparoscopic surgery.
Discussion
Our meta-analysis included fourteen fresh studies published in recent years [3,8,13-24]. The data showed a significant reduction in analgesic consumption during 24 h after laparoscopic surgery with TAP block or general anesthesia with TAP block compared with general anesthesia or no TAP block or placebo treatment, the analgesic consumption number also was reduced at 24 h. The pain was reduced at 2 h after surgery, although by 24 h the difference was no longer significant. Furthermore TAP blocks can increase postoperative nausea or vomiting. The identified studies and the risk of bias were appraised using the widely accepted Cochrane risk of bias tool, and there was no significance risk of bias. Considerable heterogeneity occurred among studies in our meta- analysis, likely due to differences in study protocols, types of surgery, and scales used to assess postoperative pain, nausea and vomiting, Heterogeneity between the studies was addressed by using a random effects model during analysis, the pooled result was still significant. In the subgroup analyses, we noted that there was no statistically significant decrease pain at rest or at rest and on movement but on movement at 2 h and 6 h. The different observations may be explained at least in part, by the variations of analgesic consumption or multimodal analgesic regimen among different countries.
Since laparoscopic surgery is considered to be a minimally invasive procedure, acute surgical pain is common in the clinical, especially in the first postoperative day. Traditionally, analgesic drugs were used for pain relief, however drug efficacy is not the only prerequisite for a positive acute surgical analgesic trial [27], in recent years, TAP blocks has demonstrated effectiveness in reducing postoperative pain when used as part of a multimodal analgesic regimen [28]. Our meta-analysis suggested that the technique of TAP block can reduce analgesic consumption and decrease the number of using analgesic.
With the increasing number of TAP block studies appearing in the literature, many meta-analyses have been published, Rita Champaneria et al. published a small meta-analysis of five RCTs showed evidence exists for the short-term efficacy (within 24 h) of transversus abdominis plane blocks during hysterectomy in terms of reported pain and morphine consumption, which may not be sustained at 48 h [29]. Two analysis indicated that TAP blocks improve pain relief after abdominal surgery [30,31], Mishriky BM et al. reported that significantly improved postoperative analgesia in women undergoing Cesarean delivery [32], However, there has been no systematic review evaluating the efficacy of the TAP block undergoing laparoscopic surgery, the effect of TAP block has not been clearly defined, We think a systematic review on this topic is timely.
Our meta-analysis showed a new problem that deserves attention. Traditionally, nausea and vomiting was thought one of opioid-related side effects, our meta-analysis showed that TAP blocks can effectively increase the incidence of postoperative nausea and vomiting after laparoscopic surgery in spite of the decreased analgesic consumption. This adverse effect needs more clinical trials to confirm due to the small number of participants.
Limitations
Our meta-analysis has several limitations. There is a significant heterogeneity in reporting the primary and secondary outcomes in our meta-analysis, which may be related to the differences in type of surgery performed, differencesin TAP block technique and doses of local anesthetics used. As this meta-analysis of published studies in English or in Japanese, we are exposed to publication bias, although the included studies were researched from differentcountries. In addition, five trials in our meta-analysis reported the incidence of postoperative nausea and vomiting after laparoscopic surgery, but the exact incidence of other side effects is not reported in our included studies, likely due to extremely small case.
Conclusion
In summary, TAP block, as a part of multimodal analgesic regimen, would result in less analgesic consumption, less requirement of analgesic, and less pain at 2 h and slightly at 6 h but at 24 h after laparoscopic surgery in comparison with usual care alone or placebo block. In addition TAP block can increase the incidence of postoperative nausea and vomiting. Because of the limited number of studies, more prospective studies with large sample size and carefully control for TAP block are needed.
Acknowledgements
We are grateful for the support from The National Natural Science Foundation. We also thank all authors of the publications included in this study for contributing information as required.
Disclosure of conflict of interest
None.
References
- 1.Bisgaard T, Klarskov B, Kehlet H, Rosenberg J. Preoperative dexamethasone improves surgical outcome after laparoscopic cholecystectomy: a randomized double-blind placebo-controlled trial. Ann Surg. 2003;238:651–60. doi: 10.1097/01.sla.0000094390.82352.cb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bisgaard T, Schulze S, Christian Hjortsø N, Rosenberg J, Bjerregaard Kristiansen V. Randomized clinical trial comparing oral prednisone (50 mg) with placebo before laparoscopic cholecystectomy. Surg Endosc. 2008;22:566–72. doi: 10.1007/s00464-007-9713-y. [DOI] [PubMed] [Google Scholar]
- 3.Hosgood SA, Thiyagarajan UM, Nicholson HF, Jeyapalan I, Nicholson ML. Randomized clinical trial of transversus abdominis plane block versus placebo control in live-donor nephrectomy. Transplantation. 2012;94:520–525. doi: 10.1097/TP.0b013e31825c1697. [DOI] [PubMed] [Google Scholar]
- 4.Gousheh SM, Nesioonpour S, Javaher Foroosh F, Akhondzadeh R, Sahafi SA, Alizadeh Z. Intravenous paracetamol for postoperative analgesia in laparoscopic cholecystectomy. Anesth Pain Med. 2013;3:214–8. doi: 10.5812/aapm.9880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.White PF. The changing role of non-opioid analgesic techniques inthe management of postoperative pain. Anesth Analg. 2005;101:S5–22. doi: 10.1213/01.ANE.0000177099.28914.A7. [DOI] [PubMed] [Google Scholar]
- 6.Cousins MJ, Lynch ME. The Declaration Montreal: access to pain management is a fundamental human right. Pain. 2011;152:2673–4. doi: 10.1016/j.pain.2011.09.012. [DOI] [PubMed] [Google Scholar]
- 7.Rafi AN. Abdominal field block: a new approach via the lumbar triangle. Anaesthesia. 2001;56:1024–1026. doi: 10.1046/j.1365-2044.2001.02279-40.x. [DOI] [PubMed] [Google Scholar]
- 8.Petersen PL, Stjernholm P, Kristiansen VB, Torup H, Hansen EG, Mitchell AU. The beneficial effect of transversus abdominis plane block after laparoscopic cholecystectomy in day-case surgery: a randomized clinical trial. Anesth Analg. 2012;115:527–33. doi: 10.1213/ANE.0b013e318261f16e. [DOI] [PubMed] [Google Scholar]
- 9.McDonnell JG, O’Donnell BD, Tuite D, Farrell T, Power C. The regional abdominal field infiltration (RAFI) technique computerised tomographic and anatomical identification of a novel approach to the transverses abdominis neuro-vascular fascial plain. Anaesthesiology. 2004;101:A899. [Google Scholar]
- 10.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:1–34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 11.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hozo SP, Djulbego B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Walter CJ, Maxwell-Armstrong C, Pinkney TD, Conaghan PJ, Bedforth N, Gornall CB, Acheson AG. A randomised controlled trial of the efficacy of ultrasound-guided transversus abdominis plane (TAP) block in laparoscopic colorectal surgery. Surg Endosc. 2013;27:2366–72. doi: 10.1007/s00464-013-2791-0. [DOI] [PubMed] [Google Scholar]
- 14.Sinha A, Jayaraman L, Punhani D. Efficacy of ultrasound-guided transversus abdominis plane block after laparoscopic bariatric surgery: a double blind, randomized, controlled study. Obes Surg. 2013;23:548–53. doi: 10.1007/s11695-012-0819-5. [DOI] [PubMed] [Google Scholar]
- 15.Parikh BK, Waghmare VT, Shah VR, Mehta T, Butala BP, Parikh GP, Vora KS. The analgesic efficacy of ultrasound-guided transversus abdominis plane block for retroperitoneoscopic donor nephrectomy: A randomized controlled study. Saudi J Anaesth. 2013;7:43–7. doi: 10.4103/1658-354X.109808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Albrecht E, Kirkham KR, Endersby RV, Chan VW, Jackson T, Okrainec A, Penner T, Jin R, Brull R. Ultrasound-guided transversus abdominis plane (TAP) block for laparoscopic gastric-bypass surgery: a prospective randomized controlled double-blinded trial. Obes Surg. 2013;23:1309–14. doi: 10.1007/s11695-013-0958-3. [DOI] [PubMed] [Google Scholar]
- 17.Ortiz J, Suliburk JW, Wu K, Bailard NS, Mason C, Minard CG, Palvadi RR. Bilateral transversus abdominis plane block does not decrease postoperative pain after laparoscopic cholecystectomy when compared with local anesthetic infiltration of trocar insertion sites. Reg Anesth Pain Med. 2012;37:188–92. doi: 10.1097/AAP.0b013e318244851b. [DOI] [PubMed] [Google Scholar]
- 18.Kane SM, Garcia-Tomas V, Alejandro-Rodriguez M, Astley B, Pollard RR. Randomized trial of transversus abdominis plane block at total laparoscopic hysterectomy: effect of regional analgesia on quality of recovery. Am J Obstet Gynecol. 2012;207:419, e1–5. doi: 10.1016/j.ajog.2012.06.052. [DOI] [PubMed] [Google Scholar]
- 19.Sandeman DJ, Bennett M, Dilley AV, Perczuk A, Lim S, Kelly KJ. Ultrasound-guided transversus abdominis plane blocks for laparoscopic appendicectomy in children: a prospective randomized trial. Br J Anaesth. 2012;106:882–6. doi: 10.1093/bja/aer069. [DOI] [PubMed] [Google Scholar]
- 20.Ra YS, Kim CH, Lee GY, Han JI. The analgesic effect of the ultrasound-guided transverse abdominis plane block after laparoscopic cholecystectomy. Korean J Anesthesiol. 2010;58:362–8. doi: 10.4097/kjae.2010.58.4.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Conaghan P, Maxwell-Armstrong C, Bedforth N, Gornall C, Baxendale B, Hong LL, Carty HM, Acheson AG. Efficacy of transversus abdominis plane blocks in laparoscopic colorectal resections. Surg Endosc. 2010;24:2480–4. doi: 10.1007/s00464-010-0989-y. [DOI] [PubMed] [Google Scholar]
- 22.El-Dawlatly AA, Turkistani A, Kettner SC, Machata AM, Delvi MB, Thallaj A, Kapral S, Marhofer P. Ultrasound-guided transversus abdominis plane block: description of a new technique and comparison with conventional systemic analgesia during laparoscopic cholecystectomy. Br J Anaesth. 2009;102:763–7. doi: 10.1093/bja/aep067. [DOI] [PubMed] [Google Scholar]
- 23.De Oliveira GS Jr, Fitzgerald PC, Marcus RJ, Ahmad S, McCarthy RJ. A dose-ranging study of the effect of transversus abdominis block on postoperative quality of recovery and analgesia after outpatient laparoscopy. Anesth Analg. 2011;113:1218–25. doi: 10.1213/ANE.0b013e3182303a1a. [DOI] [PubMed] [Google Scholar]
- 24.Fujita N, Shimizu T, Kita T, Sasaki S. Safety and economics of fondaparinux administration in the laparoscopic surgery. Masui. 2011;60:1164–8. [PubMed] [Google Scholar]
- 25.Gash KJ, Goede AC, Chambers W, Greenslade GL, Dixon AR. Laparoendoscopic single-site surgery is feasible in complex colorectal resections and could enable day case colectomy. Surg Endosc. 2011;25:835–40. doi: 10.1007/s00464-010-1275-8. [DOI] [PubMed] [Google Scholar]
- 26.Dudderidge TJ, Doyle P, Mayer EK, Taylor J, Agrawal S, Stolzenburg JU, Winkler MH. Evolution of care pathway for laparoscopic radical prostatectomy. J Endourol. 2012;26:660–5. doi: 10.1089/end.2011.0427. [DOI] [PubMed] [Google Scholar]
- 27.Singla NK, Desjardins PJ, Chang PD. A comparison of the clinical and experimental characteristics of four acute surgical pain models: dental extraction, bunionectomy, joint replacement, and soft tissue surgery. Pain. 2014;155:441–56. doi: 10.1016/j.pain.2013.09.002. [DOI] [PubMed] [Google Scholar]
- 28.Petersen PL, Mathiesen O, Torup H, Dahl JB. The transverses abdominis plane block: a valuable option for postoperative analgesia? A topical review. Acta Anaesthesiol Scand. 2010;5:529–35. doi: 10.1111/j.1399-6576.2010.02215.x. [DOI] [PubMed] [Google Scholar]
- 29.Champaneria R, Shah L, Geoghegan J, Gupta JK, Daniels JP. Analgesic effectiveness of transversus abdominis plane blocks after hysterectomy: a meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2013;166:1–9. doi: 10.1016/j.ejogrb.2012.09.012. [DOI] [PubMed] [Google Scholar]
- 30.Charlton S, Cyna AM, Middleton P, Griffiths JD. Perioperative transversus abdominis plane (TAP) blocks for analgesia after abdominal surgery. Cochrane Database Syst Rev. 2010:CD007705. doi: 10.1002/14651858.CD007705.pub2. [DOI] [PubMed] [Google Scholar]
- 31.Johns N, O’Neill S, Ventham NT, Barron F, Brady RR, Daniel T. Clinical effectiveness of transversus abdominis plane (TAP) block in abdominal surgery: a systematic review and meta-analysis. Colorectal Dis. 2012;14:e635–42. doi: 10.1111/j.1463-1318.2012.03104.x. [DOI] [PubMed] [Google Scholar]
- 32.Mishriky BM, George RB, Habib AS. Transversus abdominis plane block for analgesia after Cesarean delivery: a systematic review and meta-analysis. Can J Anaesth. 2012;59:766–78. doi: 10.1007/s12630-012-9729-1. [DOI] [PubMed] [Google Scholar]


