Abstract
Background
Quitlines and worksite-sponsored cessation programs are effective and highly accessible, but limited by low utilization. Efforts to encourage use of cessation aids have focused almost exclusively on the smoker, overlooking the potential for friends, family, coworkers and others in a tobacco user’s social network to influence quitting and use of effective treatment.
Methods
Longitudinal, observational pilot feasibility study with six-week follow-up survey.
Setting/Participants
Employees of three national corporations, with a combined target audience of 102,100 employees.
Intervention
The Helpers Program offers Web-based brief intervention (BI) training to activate social networks of tobacco users to encourage quitting and use of effective treatment. Helpers was offered from 1/10/08 to 3/31/08, as a treatment engagement strategy, together with Free and Clear’s (F&C) telephone/Web-based cessation services.
Main outcome measures
web-site utilization, training completion, post-training changes in knowledge and self-efficacy with delivery of BIs, referrals to F&C, and use of BI training.
Results
There were 19,109 unique visitors to the Helpers Web-site. Of these, 4727 created user accounts; 1427 registered for Helpers Training; 766 completed training. There were 445 visits to the referral page and 201 e-mail or letter referrals generated. There were 67 requests for technical support. Of follow-up survey respondents (n=289), 78.9% reported offering a BI.
Conclusions
Offering the Helpers Program Web-site to a large, diverse audience as part of an employer-sponsored worksite health promotion program is both feasible and well accepted by employees. Website users will participate in training, encourage quitting, and refer smokers to quitline services.
Introduction
Effective tobacco cessation treatments are more widely available than ever before. The Public Health Service (PHS) Guideline (1), updated in 2008, identifies a number of experimentally validated behavioral and pharmacologic therapies for tobacco cessation including telephone quit line counseling, individual (brief and more intensive), group, and as well as several first line medications (bupropion SR, varenicline, and nicotine replacement therapies: gum, patch, and lozenge (available over the counter) and inhaler, and nasal spray (available by prescription). While tobacco cessation quit lines and worksite-sponsored programs that incorporate guideline-based treatment approaches are both effective and easily accessible, their public health impact is limited by under-utilization. (2)
Background
Tobacco cessation brief interventions (BIs) are a low-intensity treatment strategy comprised of the evidence-based National Cancer Institute/PHS 5 A’s (Ask, Advise, Assess, Assist, Arrange). (1) A meta-analysis conducted for the 2008 PHS guideline update reaffirms earlier conclusions that low-cost, low-intensity BIs are effective for increasing quit rates and notes that maximal efficacy of BIs is achieved when multiple providers intervene. (1;4) Abrams and Orleans, et al. (5) note that more intensive -- and costly -- clinical interventions have higher efficacy, but due to their limited reach, the overall population health impact is smaller than lower-intensity, lower-cost interventions with lower efficacy but broader reach.
However, tobacco cessation BI training has focused almost exclusively on health care professionals, particularly physicians, thus limiting the potential public health reach and impact of BIs. Despite tobacco cessation BIs being the single most effective and cost-effective of all adult clinical preventive services, healthcare providers deliver cessation BIs to less than half of tobacco-using patients. (6) This gap between recommended best practices and provider behavior reveals a limitation of relying solely on health care providers to advise quitting and encourage use of cessation aids. Furthermore, tobacco use is increasingly a problem disproportionately affecting populations with less education, income, and health insurance, and some racial and ethnic minorities (7) – populations also facing multiple barriers to accessing the health care system. (8)
To date, efforts to increase smokers’ use of cessation aids, have focused almost exclusively on the smoker. The tobacco control field has devoted little attention to strategies to drive consumer (tobacco user) demand for cessation through involvement of concerned “health influencers”, e.g. friends, family, coworkers and others in a tobacco user’s social network who want a smoker to quit. More distant members of smoker’s social network can also influence quitting. A recent analysis of more than 30 years of data from the Framingham Heart Study found social networks have an important influence on quitting behavior. Smoking cessation by a spouse decreased the chances of a person smoking by 67%. Smoking cessation by a friend, or coworker in a small firm, decreased chances of smoking by 36% and 34% respectively. Study findings also suggested that whole groups of people were quitting together. (9)
In the treatment of nicotine as well as other drug and alcohol addictions, it has long been recognized that family and friends are an important influence in engaging users in treatment and can also play a vital role in treatment adherence and success. (10, 11, 12, 13) Tobacco cessation BI training programs have been available for more than two decades. (14) With few exceptions BI training has focused on healthcare providers, overlooking the potential of other health influencers to encourage quitting and the use of effective treatment.
Methods
This was a longitudinal, observational proof-of-concept pilot study with one six-week follow-up survey. The purpose was to test the feasibility and acceptability of the Helpers Program as a worksite community engagement strategy to: encourage peer to peer brief tobacco interventions, promote more quit attempts, and encourage referrals to Quit for Life™ tobacco treatment program by friends, family and co-workers. The Free & Clear Quit for Life™ tobacco treatment program is a national leader in integrated telephone and web-based cognitive behavioral coaching for tobacco cessation. The study was reviewed and approved by the University of Arizona’s Human Subjects Committee.
Sample population
Three large national corporations participated in the Helpers Program pilot study including: a National Retailer (n=84,150 employees), a Transportation and Logistics Corporation (n = 87,450 employees) and a Health Services Corporation (n = 14,850 employees). The target audience for this pilot study (n = 102,100) included all employees in the National Retailer and Health Services corporations, and only a subpopulation of “health coaches” (n=3000) in the Transportation and Logistics Corporation. The three corporations had a combined total of 131,590 employees and 378,550 dependents. Employees and dependents of all three corporations were eligible for Quit for Life™.
Intervention
The Helpers Program (“Helpers”) is a research-based intervention developed at the University of Arizona and funded by the National Cancer Institute (NCI). Helpers teaches health influencers to encourage quitting tobacco with a supportive, non-confrontational, “non-nagging” approach. It is a community-based intervention providing BI training and other community-oriented support to health influencers who want to help a tobacco user quit. Helpers has five components: BI training (in-person and web-based formats), an on-line community resource center, media campaign, quit kits and evaluation instruments. Of these, the following four components were deployed for the pilot study. Helpers Training (web-based only) which addressed: communication skills; assessing motivators and barriers to quitting and readiness to quit; offering support for quitting; cessation medications; referral to cessation services (specifically Quit for Life™). Participants accessed Helpers Training through the on-line Helpers Community Resource Center (Helpers CoRC) website, a virtual gathering place for persons interested in helping someone quit tobacco which also features a browsing library of cessation topics, tobacco-related news and current events and discussion forums where Helpers can share stories and offer each other support and suggestions for helping. For this pilot, the discussion forums were turned off to avoid diverting attention away from the Quit for Life™ discussion boards. Corporations were given the Helpers Outreach Media Campaign (a series of tested ads and messages to activate friends, coworkers and family members to become helpers) to use in program promotion. Helpers Program Evaluation Instruments, a core set of measures developed and tested through the original NCI-funded research, were used for evaluation. The Helpers program components were offered together with the Quit for Life™ tobacco treatment program, which provides individualized, integrated web- and phone-based cognitive behavioral coaching for tobacco dependence treatment.
A custom website portal page was constructed for the study, which served as the “landing page” for all employees accessing the site. The landing page offered information about the Helpers Program, a link to register as a study participant and information regarding the Quit for Life™ Program. The landing page also offered a link to a study specific page on the Quit for Life™ web site where participants could print out a personalized letter or send an email from themselves urging tobacco users to explore the Quit for Life™ Program. The Helpers website banner (appearing on the landing page and all pages within the Helpers website) was customized with the Quit for Life™ logo and a link to the Quit for Life™ referral page.
Employees could navigate to the Helpers Program landing page through a link on their companies’ intranet or by manually entering the URL for the Helpers landing page in their web browser. Employees wishing to enter the Helpers website from the landing page were required to create user accounts by acknowledging acceptance of the research participant disclaimer, completing a site registration form, and creating a username. Creation of a user account enabled tracking of participants’ use of the Helpers web site components. Passwords were sent to the email address provided by the participant to discourage spurious registrations. The site registration form collected only basic demographics required for a federally funded research study. Participants were not required to indicate their employer because of sensitivities related to corporate confidentiality.
Once registered as study participants, employees were directed to a personalized homepage that greeted the participant by name and offered links to most recent pages visited. Participants who registered for the Helpers Training also were given a direct link to the last page visited in the training. Participants were encouraged to sign up for the Helpers Training and were also free to browse topics of interest and read news items. Participants choosing to take the Helpers Training were required to complete a training registration form and pre-test. To download a training completion certificate, participants were required to complete all six training modules and the post-test.
Implementation
While the content of the Helpers Program site was the same for all participants, each corporation chose to promote the program to employees in ways consistent with their other wellness programs. The three-month pilot study period began on January 10 and ended on March 31, 2008. Due to the nature of the initiative being a “real world” pilot, the program was rolled out at different times as each company worked to list the information on their website, newsletters, and send emails. Consequently, only the employees of the National Retailer had access to the Helpers site for the entire 12-week period. Employees of the Transportation and Logistics Corporation and the Health Services Corporation had access to the site for 10 weeks and 6 weeks respectively.
The National Retailer offers a rewards program permitting employees to earn points redeemable for merchandise and other incentives to promote participation in its corporate wellness programs. To introduce Helpers to its employees, the National Retailer added Helpers Program information to the company intranet and a link to the Helpers Program on the intranet home page; updated the employee rewards program site with information about Helpers and; offered a significant reward point incentive for completion of the Helpers training. Employees were required to fax their Helpers certificate of training to the corporation as proof of training completion.
The Transportation and Logistics Corporation focused their Helpers Program dissemination efforts on an existing cadre of 3000 health and wellness promoters (out of 87450 total employees). This Corporation sent an email about the Helper Program training to onsite health coaches, wellness champions and occupational nurses, and updated the health coach intranet with a link to the Helpers Program website.
The Health Services Corporation, with a target audience of 14,850 employees sent an email to employees informing them of the Helpers training opportunity; updated the company intranet home page with Helper information and a link to the Helper site; and included information about Helpers in company newsletters.
Follow-up survey
Six weeks after the 12-week pilot intervention period ended, an e-mail survey was sent to all study participants to assess use of information and training received from the Helpers Website. As an incentive, all survey respondents were entered in to a drawing for ten $50 cash prizes. Two weeks after the first email, one follow-up reminder email was sent to all valid email addresses, encouraging participants to respond to the follow-up survey. Limited resources, time and scope of the pilot precluded more extensive or multimodal follow-up for non-responders.
Measurements
The principal measures of feasibility and acceptability of the Helpers Program pilot were numbers of: requests for technical support for the Helpers website; unique visitors to the Helpers Program landing page; Helpers website registrations (study participants); Helpers Training registrations; and participants completing Helpers Training (certificates issued).
Secondary measures of outcomes for the Helpers pilot included: post-training changes in knowledge and self-efficacy scores; self-reported BIs and referrals on follow-up survey; and unique visits to the Quit for Life™ referral page from the links on the Helpers landing page and website banner.
Since participants’ employer could not be assessed directly, an effort was made to distinguish company affiliation for visits to the landing page by using unique URL strings. However, variations in company implementation, intranet characteristics, user behavior (e.g. giving a gmail or yahoo email address instead of company email, not using link from intranet page), and access to the site from home computers obscured efforts to track company affiliation with sufficient accuracy.
Analysis
The actual recorded behaviors of web-site users were used to separate the total population of users into three participant categories based upon behaviors using the site. These categories were the basis for subsequent comparative analyses of web-site use. “Browsers” were defined as employees who created user accounts, browsed site topics, but did not register for Helpers training. “Non-completers” are participants who created a user account, registered for Helpers training but did not complete the training. “Completers” created a user account, registered for and completed Helpers training. Since there were difficulties in accurately assigning company affiliation, company-related data was only examined descriptively.
Kruskal-Wallis chi-2 test was used to compare the equality medians across the three user categories (15), and Pearson’s chi-2 test to compare the distribution of characteristics across the three categories. (16) Paired t-tests were used to compare pre- and posttest scores. Statistical analyses were performed with Stata statistical software, Version 9.2 (StataCorp, College Station, TX).
Results
Website visits and Technical assistance
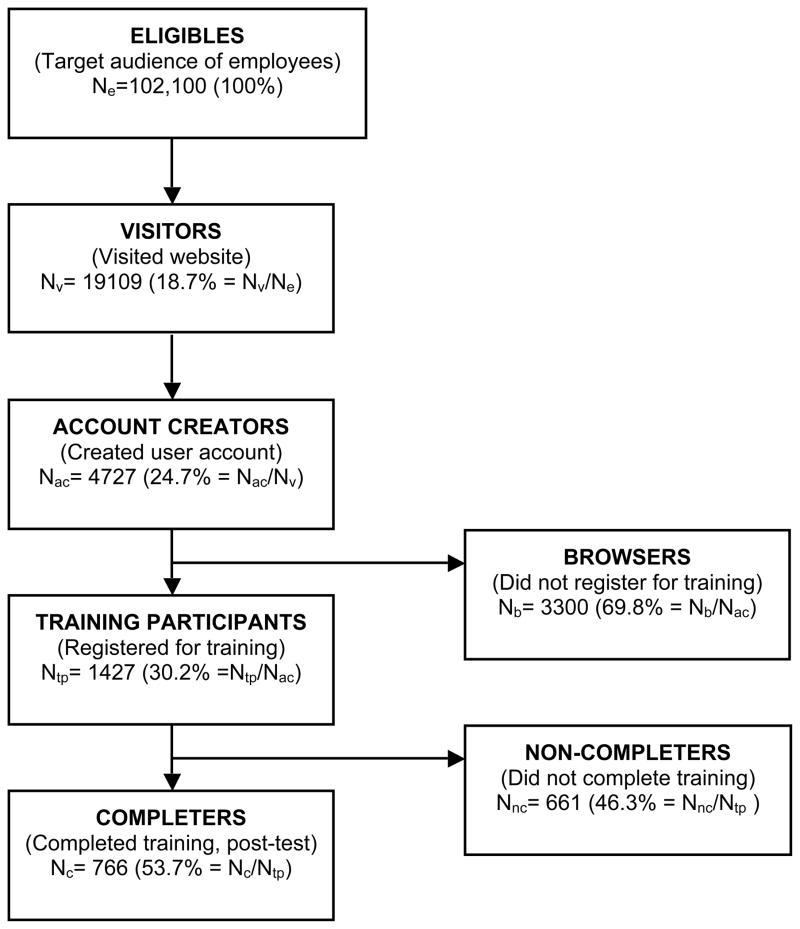
There were 19,109 unique visitors to the Helper’s home page during the 12-week study period. See Figure 1. Participants could submit a web form, accessible form any page on the site, requesting technical support. Overall, visitors and participants reported very few technical difficulties with the website. There were a total of 67 (1.4% of account creators) requests for technical support for the following issues: problems with printing or faxing certificates of training (not site-related) (n=34); Training navigation (completion of training activities) (n=13); Study registration (n=9); Lost password (did not use automatic recovery feature) (n=5); Request for additional information or handouts (n=4); Change in email address (n=1); and Access to Quit for Life referral page (n=1).
Figure 1.
Breakdown of target audience and study participants by user category
Website use and training participation
Figure 1 shows distribution of participants by category. Of the site visitors, 4,727 created user accounts (registered as study participants). Nearly one third of account creators (n = 1427) registered for Helpers Training (Trainees). These participants were divided into two categories; training Completers (n = 766) and Non-completers (n = 661). The remaining participants were able to browse topics in the website information center, participate in learning activities and read news items (Browsers, n = 3300). Table 1 gives demographic characteristics for each of the three participant categories. Overall, more women than men created user accounts on the Helpers website. The majority of participants were Caucasian. More than half of participants did not have a college degree.
Table 1.
Characteristics of Helpers Web-site participants (N=4727) (% unless otherwise indicated)
| Characteristic | Browsers (n=3300) | Non-Completers (n=661) | Completers (n=766) |
|---|---|---|---|
| Gender (% female) | 58.0 | 59.4 | 56.3 |
| Age median (range) | 31 (18, 73) | 33 (18, 70) | 32 (18, 66) |
| Race/Ethnicity | |||
| Hispanic | 8.1 | 7.3 | 7.2 |
| African-American** | 9.7 | 7.6 | 5.6 |
| Asian | 1.2 | 0.8 | 1.2 |
| Caucasian/White** | 78.1 | 82.2 | 83.9 |
| Native Hawaiian/Other Pacific Islander** | 0.7 | 1.5 | 0.1 |
| Native American** | 4.6 | 2.1 | 3.9 |
| Other | 4.8 | 3.5 | 3.8 |
| Education** | |||
| Less than high school | 1.0 | 0.8 | 0.3 |
| High school/GED | 30.2 | 21.8 | 24.0 |
| Some College | 43.6 | 46.2 | 40.3 |
| College Degree or higher | 25.2 | 31.2 | 35.4 |
| Occupation** | |||
| Health/Behavioral Health | 2.3 | 2.0 | 6.6 |
| Education | 0.9 | 1.5 | 0.4 |
| Administrator/Manager | 15.4 | 22.7 | 16.9 |
| Sales/Marketing | 52.8 | 41.9 | 47.1 |
| Clerical/Secretarial | 9.3 | 10.4 | 11.5 |
| Not Employed a | 4.6 | 3.1 | 3.1 |
| Other | 14.7 | 17.3 | 14.4 |
Includes retired persons, homemakers/caretakers and students.
Kruskal-Wallis χ2 tests, p<=.05
Pearson’s χ2 tests, p<=.05
Changes in knowledge, self efficacy and opinions
There were significant increases in training completers’ mean knowledge scores (% correct answers) from pre-test (M=67.5 %, SD = 17.8) to post test (M= 77.3%, SD = 11.0), p < 0.001. As shown in Table 2, completers also had significant increases in scores for self-efficacy with BI skills. There were also significant changes in participant opinions in the direction of more support for use evidence-based cessation aids. Participants were asked to indicate agreement with statements about use of various cessation aids where “Never Agree”=0; “Sometimes Agree”=1; “Often Agree” =2; and “Always Agree”=3. From pre-test to post-test, mean agreement score for “Tobacco users should first try to quit on their own, before getting professional help from a quitline, quit smoking class or other professional help” decreased from 1.04 (SD 0.88) to 1.35 (SD 0.87) (p<0.001). Scores for “Tobacco users should first try to quit on their own, before trying approved medications to help quitting” decreased from 1.62 (SD 0.89) to 1.24 (SD 0.89) (p<0.001). Agreement with “Tobacco users should seek help professional help every time they want to quit - for example, calling a quit line or going to a quit smoking class” increased from 1.24 (SD 0.79) to 1.54 (SD 0.90) (p<0.001). Agreement with “Tobacco users should use approved medications to help themselves every time they want to quit.” increased from 1.08 (SD 0.76) to 1.34 (SD 0.86) (p<0.001).
Table 2.
Changes in training participant self-efficacy with brief intervention skills (n=766)
| Self efficacy question | Pre a M (SD) |
Post a M (SD) |
Sig p |
|---|---|---|---|
| I am confident that I can: | |||
| accurately assess a tobacco user’s motivation to quit | 1.55 (0.70) | 2.02 (0.72) | p<.001 |
| explore issues related to quitting smoking, even with someone not interested in quitting | 1.49 (0.73) | 1.88 (0.78) | p<.001 |
| personalize the benefits of quitting with each individual tobacco user | 1.78 (0.76) | 2.13 (0.75) | p<.001 |
| provide simple instructions about nicotine medications to help quitting that can be bought without a prescription | 1.50 (0.87) | 2.09 (0.79) | p<.001 |
| tell a tobacco user about prescription medications to help quitting | 1.48 (0.93) | 2.00 (0.86) | p<.001 |
| help a tobacco user develop a personalized plan for quitting | 1.58 (0.90) | 2.18 (0.77) | p<.001 |
| help a tobacco user see the difference between current behavior and long-term goals | 1.80 (0.81) | 2.23 (0.74) | p<.001 |
| negotiate an agreement with an individual for change in tobacco use behavior | 1.59 (0.82) | 2.10 (0.76) | p<.001 |
| arrange for appropriate follow-up with a tobacco user | 1.66 (0.85) | 2.19 (0.77) | p<.001 |
Opinion question answers were scored: “Never Agree”=0; “Sometimes Agree”=1; “Often Agree” =2; “Always Agree”=3
Referrals to Quit for Life Program
The “Want to Help a Loved One” page loaded 445 times, and recorded 201 clicks on referral links, which generated 97 emails and 104 letters. Due to the way the link was constructed, we could not systematically measure enrollments into the Quit for Life Program generated by the pilot nor attribute the referral clicks to a particular category of user (e.g. Browser versus Completer). Referrals made without using the website could not be tracked. Persons enrolling into Quit for Life are asked how they heard about the program. “Friends and Family” is one of the categories. Monitoring the Friends and Family category revealed no significant increase over pre-study levels. However, it must be noted that since none of these corporations had offered the Quit for Life program during the same time period in the previous year, there was no baseline numbers with which to compare the Friends and Family metric.
Follow-up survey of self-reported BIs
The survey had a very limited response (n=289, 6%). Nevertheless, results are presented in the spirit of sharing lessons learned that are relevant for designing future studies. Of note, an estimated five hundred e-mail surveys were undeliverable because of an invalid e-mail address. Also, 42.2% (n=1,997) participants gave email addresses often used for convenience (e.g. yahoo, gmail, hotmail).
More than half of the survey respondents had completed training, and 91.0% reported offering a BI since registering on the Helpers Web-site. Characteristics of self-reported BIs are shown in Table 3. Family members, friends, and co-workers/colleagues were the most frequently reported recipients of Helpers’ BIs. Personally knowing the tobacco user and having the tobacco user indicate a desire to quit were the most frequently reported motivations for offering a BI to a tobacco user. The majority of respondents reported that they discussed tobacco user’s reasons for quitting, assessed the user’s readiness to quit, and offered assistance with quitting. Nearly a third discussed use of cessation medications.
Table 3.
Self-reported brief intervention (BI) behavior since registering on website
| Characteristic/behavior | Browsers N = 52 | Non-Completers N = 45 | Completers N = 131 |
|---|---|---|---|
| Mean number of BIs (SD) | 3.65 (2.98) | 2.96 (1.68) | 4.97 (9.99) |
| Recipient of BI | % | % | % |
| Family member | 69.2 | 62.2 | 61.8 |
| Friend | 55.8 | 60.0 | 58.8 |
| Acquaintance | 3.9 | 6.7 | 11.5 |
| Co-worker/colleague | 44.2 | 42.2 | 44.3 |
| Supervisor/boss | 3.9 | 0.0 | 3.3 |
| Employee/subordinate | 11.5 | 15.6 | 5.3 |
| Client/Patient/Student | 1.9 | 2.2 | 11.5 |
| Stranger | 0.0 | 6.7 | 4.6 |
| Motivation for BI | % | % | % |
| Knew tobacco user | 82.7 | 84.4 | 82.4 |
| User wanted to quit | 55.8 | 37.8 | 55.7 |
| Tobacco use at home/car/work | 19.2 | 15.6 | 31.3 |
| Violation of a no-tobacco rule | 5.8) | 2.2 | 5.3 |
| Cigarette smoke bothersome | 32.7 | 24.4 | 32.8 |
| Cigarette smoke bothering a child, pet, etc. | 13.5 | 11.1 | 13.7 |
| User had tobacco-related health problems | 28.9 | 26.7 | 29.8 |
| Wanted to practice skills | 13.5 | 8.9 | 28.2 |
| Part of job responsibilities | 5.8 | 11.1 | 18.3 |
| User was referred for assistance | 3.9 | 0.0 | 2.3 |
| Other | 5.8 | 0.0 | 1.5 |
| Discussed in typical BI | % | % | % |
| Reasons to quit | 96.1 | 88.9 | 88.6 |
| Readiness to quit | 57.7 | 62.2 | 63.4 |
| Assistance with quitting | 50.0 | 51.1 | 52.7 |
| Offered handouts or materials | 11.5 | 6.7 | 17.6 |
| Medication options | 44.2 | 24.4 | 45.0 |
| Referral to Quit for Life | 26.9 | 22.2 | 32.8 |
Discussion
This pilot feasibility study has a number of strengths. First, the Helpers Program is unique in being a research-based program that specifically targets social networks of smokers with training to activate network members to encourage quitting and use of evidence-based treatment. A second strength is that this is a study of a real-world implementation of a research-based program. The study was conducted with three large national corporations representing widely differing areas of business across the country with correspondingly diverse corporate structures, intranet infrastructures, employee wellness programs, employee job-types, employment experience, education levels and internet access. A strength of the intervention is the ability to track use of “click to refer” links, which documented actual action taken by a health influencer to encourage someone to quit and to use evidence-based treatment. This “click stream” data provided additional evidence of health influencer activation beyond participants’ self-reports of BIs and treatment referrals.
This pilot study is limited by its observational design. The difficulties with accurately attributing all participating employees to one of the three corporations preclude meaningful assessment of differential effects of the three different dissemination strategies. Another limitation is the heterogeneity of the target audience, e.g. all employees for two corporations versus a preselected sub-population of health coaches for the third corporation. The ability to draw conclusions from the follow-up survey data is severely limited by the low response rate, underscoring the need for more extensive and potentially multi-modal follow-up efforts in future studies. Outcomes measures of brief intervention behaviors post-web-site exposure are self-reported. Clicks to referral tools were documented, but not actual referrals. Consequently it is unknown if enrollments into Quit for Life™ were a result of referrals by persons who participated in the Helpers Program website.
Conclusions
This pilot study demonstrated that the Helpers Program can be successfully offered to a large, diverse, and geographically dispersed audience as part of an employer-sponsored worksite health promotion program. Despite users accessing the program through diverse internet and intranet infrastructures, users reported few technical support issues. Overall, written comments and feedback from users was very positive. Results indicate that when offered through worksites, employees will use the Helpers Program website, participate in Helpers training, and will also encourage their co-workers to quit and use quitline services.
Although the present study has limitations, the results have some intriguing implications for employer-sponsored tobacco treatment programs and for further research on interventions to activate social networks to promote cessation. Although a cost-effectiveness analysis was beyond the scope of this pilot, similar to other web-based interventions, cost of disseminating this existing web-intervention were minimal and the reach broad. Findings suggest the Helpers Program has potential to be a relatively low-cost, easily disseminated strategy for employers to increase employee engagement in smoking cessation services. These findings should be explored further in a larger scale, experimental design, efficacy trial, that is sufficiently resourced to allow more extensive methods of subject and referral tracking and follow-up. In future studies, lessons learned from this pilot will facilitate more accurate affiliation of participants’ with their employer, such that effects from different dissemination and implementation strategies could be compared. Furthermore, the Helpers Program can be directed to all employees, not just tobacco users. Thus, the employer has the opportunity to promote a wellness program with relevance to a much larger group of employees, including non-smokers with dependents who smoke. The Helpers Program can be used as a tobacco treatment engagement strategy with potential to reach beyond the workplace and engage both tobacco using employees and their dependents.
The present study’s findings also indicate the need for further research to address such questions as: What is the impact of incentives or other promotional strategies to increase employee participation in Helpers? Do trained Helpers recruit others to become Helpers? What are the characteristics of the content, context and target recipients of Helpers’ brief interventions, e.g. when, where, and with whom are cessation medications discussed or referrals made to professional cessation services? How does Helper intervention behavior evolve over time and with experience? Finally, research is needed on the impact of Helpers’ interventions on smokers’ behaviors such as use of evidence-based cessation aids, quit attempts and quits; and the effect on their relationships with Helpers.
Acknowledgments
This work was supported by National Cancer Institute, Research in State and Community Tobacco Control Interventions RO1CA093957. Participant incentive prizes for e-mail follow-up survey were provided by Free and Clear, Inc.
Reference List
- 1.Fiore MC, Jaen CR, Baker TB, et al. Treating Tobacco Use and Dependence: 2008 Update. Rockville, MD: U.S. Department of Health and Human Services. Public Health Service. Clinical Practice Guideline; May 1, 2008. [Google Scholar]
- 2.Moher M, Hey K, Lancaster T. Workplace interventions for smoking cessation (Review) Cochrane Database of Systematic Reviews. 2005;(2):Art. No: CD003440. doi: 10.1002/14651858.CD003443.pub2. [DOI] [PubMed] [Google Scholar]
- 3.Cokkinides VE, Ward E, Jemal A, Thun MJ. Under-use of smoking-cessation treatments: results from the National Health Interview Survey, 2000. American Journal of Preventive Medicine. 2005;28(1):119–22. doi: 10.1016/j.amepre.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 4.Fiore MC, Bailey WC, Cohen SJ, Dorfman SF, Goldstein MG, Gritz ER, et al. Smoking cessation. Rockville, MD: United States Department of Health and Human Services (USDHHS), Public Health Service, Agency for Health Care Policy and Research; 1996. [Google Scholar]
- 5.Abrams DB, Orleans CT, Niaura RS, Prochaska JO, Velicer WF. Integrating individual and public health perspectives for treatment of tobacco dependence under managed health care: A combined stepped-care and matching model. Ann Behav Med. 1996;18(4):290–304. doi: 10.1007/BF02895291. [DOI] [PubMed] [Google Scholar]
- 6.Coffield AB, Maciosek MV, McGinnis JM, Harris JR, Caldwell MB, Teutsch SM, et al. Priorities among recommended clinical preventive services.[see comment] American Journal of Preventive Medicine. 2001;21(1):1–9. doi: 10.1016/s0749-3797(01)00308-7. [DOI] [PubMed] [Google Scholar]
- 7.CDC. Adult Cigarette Smoking in the United States: Current Estimates. Centers for Disease Control and Prevention; Feb 28, 2007. [Google Scholar]
- 8.Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: The National Academic Press; 2003. [PubMed] [Google Scholar]
- 9.Christakis NA, Fowler JH. The Collective Dynamics of Smoking in a Large Social Network. N Engl J Med. 2008;358(21):2249–2258. doi: 10.1056/NEJMsa0706154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Landau J, Stanton MD, Brinkman-Sull D, Ikle D, McCormick D, Garrett J, et al. Outcomes with the ARISE approach to engaging reluctant drug- and alcohol-dependent individuals in treatment. Am J Drug Alcohol Abuse. 2004;30(4):711–748. doi: 10.1081/ada-200037533. [DOI] [PubMed] [Google Scholar]
- 11.Marlowe DB, Merikle EP, Kirby KC, Festinger DS, McLellan AT. Multidimensional assessment of perceived treatment-entry pressures among substance abusers. Psychol Addict Behav. 2001;15(2):97–108. doi: 10.1037//0893-164x.15.2.97. [DOI] [PubMed] [Google Scholar]
- 12.De Civita M, Dobkin PL, Robertson E. A study of barriers to the engagement of significant others in adult addiction treatment. J Subst Abuse Treat. 2000;19(2):135–144. doi: 10.1016/s0740-5472(00)00095-7. [DOI] [PubMed] [Google Scholar]
- 13.Stanton MD. Getting reluctant substance abusers to engage in treatment/self-help: A review of outcomes and clinical options. J Marital Fam Ther. 2007;30(2):165–182. doi: 10.1111/j.1752-0606.2004.tb01232.x. [DOI] [PubMed] [Google Scholar]
- 14.Lancaster T, Silagy C, Fowler G. Training health professionals in smoking cessation. Cochrane Datab Syst Rev. 2000;(3):CD000214. doi: 10.1002/14651858.CD000214. [DOI] [PubMed] [Google Scholar]
- 15.Kruskal WH, Wallis A. Use of ranks in one-criterion variance analysis. J Amer Statistical Assoc. 1952;47(260):583–621. [Google Scholar]
- 16.Chernoff H, Lehmann EL. The use of maximum likelihood estimates in χ2 tests for goodness-of-fit. Annals of Mathematical Statistics. 1954;25:579–586. [Google Scholar]