Knowledge into Practice.
Identification and reporting of suspected adverse drug reactions, or pharmacovigilance, is an important patient safety activity that is the responsibility of all clinicians, especially pharmacists.
Pharmacovigilance is particularly important for newer drugs, as rare drug-related adverse effects are not always identified in clinical trials and the prescribing of medications in the “real world” often yields new safety concerns.
Pharmacists should be aware that the reporting of suspected adverse drug reactions to Health Canada does not require that a correlation or direct cause-and-effect relationship be established.
When assessing suspected drug-related adverse effects, it is imperative for pharmacists to use a systematic approach involving a standardized clinical tool such as the Naranjo algorithm.
Mise En Pratique Des Connaissances.
La détection et la déclaration des effets indésirables présumés d’un médicament, ou pharmacovigilance, est une activité importante pour la sécurité des patients. Cette responsabilité incombe à tous les cliniciens, et plus particulièrement aux pharmaciens.
La pharmacovigilance est particulièrement importante dans le cas des nouveaux médicaments, car les essais cliniques ne permettent pas toujours d’identifier les effets indésirables rares et que l’usage des médicaments en « situations réelles » met souvent en lumière de nouvelles préoccupations liées à la sécurité des produits.
Il importe que les pharmaciens sachent, que pour déclarer un effet indésirable présumé d’un médicament à Santé Canada, il n’est pas nécessaire d’établir une corrélation ou une relation de cause à effet directe.
Durant l’évaluation d’effets indésirables présumés liés à un médicament, il est impératif que les pharmaciens utilisent une approche systématique fondée sur un outil clinique normalisé, comme l’algorithme de Naranjo.
Introduction
In 2004, the anti-inflammatory drug rofecoxib was voluntarily withdrawn from the market due to cardiovascular safety concerns. Although this case was highly publicized, it was not an isolated example. Between 1997 and 2011, 25 drugs were withdrawn from the Canadian market due to safety concerns identified through postmarketing surveillance or pharmacovigilance. Identification and reporting of suspected adverse drug reactions through pharmacovigilance is an important patient safety activity that is the responsibility of all clinicians, especially pharmacists. It is particularly important for newer drugs, as rare adverse effects are not always identified in clinical trials and the prescribing of medications in the “real world” often yields new drug-related safety concerns. In this article, we aim to explore the ongoing monitoring and assessment of suspected drug-related adverse effects and discuss recent examples of newly identified drug safety concerns.
Rofecoxib
In 1999, one of the world’s most eagerly anticipated drugs was introduced: rofecoxib (brand name Vioxx). This “blockbuster” new anti-inflammatory was destined to revolutionize pain control for millions of patients worldwide. It was a novel agent in a new class of anti-inflammatory drugs known as cyclooxygenase-2 (COX-2) inhibitors, which were touted as being as effective for pain as traditional nonsteroidal anti-inflammatory drugs but with considerably fewer adverse gastrointestinal (GI) effects. A combination of real-word effectiveness and aggressive marketing led rofecoxib to become one of the bestselling prescription drugs of all time. By 2004, it was estimated that over 84 million people worldwide had received a prescription for rofecoxib, with annual sales exceeding $2.5 billion.1 It was glory days for both patients and the drug company, but this prosperity did not last.
On September 30, 2004, rofecoxib was voluntarily withdrawn from the global market due to concern over an increased risk of cardiovascular (CV) events.2 The downfall of rofecoxib actually began in 2000, with the publication of the Vioxx Gastrointestinal Outcomes Research (VIGOR) study, which compared rofecoxib with naproxen in patients with rheumatoid arthritis.3 Both rofecoxib and naproxen demonstrated similar efficacy, but, as predicted, rofecoxib had significantly fewer GI events. There was also a small but statistically significant increase in the rate of myocardial infarction (MI) in the rofecoxib group of 0.3%. In the discussion, the authors attributed this increased risk to the lack of use of low-dose acetylsalicylic acid in high-risk patients. Despite these findings, no safety advisory regarding rofecoxib was issued, and the aggressive marketing campaign continued until 2004, when the safety monitoring board of the Adenomatous Polyp Prevention on Vioxx (APPROVe) study recommended that it be terminated early due to an increased rate of CV events with rofecoxib.4 APPROVe was designed to investigate the effect of rofecoxib versus placebo on the recurrence of neoplastic polyps in patients with a history of colorectal adenomas. The total number of CV events in the rofecoxib group was 1.6% higher than placebo over 2.4 years, for a number needed to harm of 63. Rofecoxib was withdrawn from the worldwide market the same day that the APPROVe study was terminated.
Rofecoxib was one of the most widely prescribed medications ever to be removed from the market. This example clearly highlights the importance of postapproval monitoring of suspected drug-related adverse events. Although rofecoxib may be the most highly publicized drug withdrawal of our time, it is not an isolated example in the pharmaceutical industry. Between 1997 and 2011, 25 drugs were withdrawn from the Canadian market due to safety concerns, and many more have received warnings about new or suspected adverse effects.2,5 What can we learn from the ill-fated existence of rofecoxib? In this review, we examine the importance of maintaining pharmacovigilance and the role of the pharmacist.
Pharmacovigilance
Pharmacovigilance is defined by the World Health Organization (WHO) as “the science and activities relating to the detection, assessment, understanding and prevention of adverse effects or any other drug-related problem.”6 It is a term often used synonymously with postmarketing surveillance, although, by definition, it does not require the drug to already be approved for use. Maintaining pharmacovigilance is imperative, as new drugs do not undergo an extensive safety review by Health Canada prior to their market release. Often drugs are approved based on 1 or 2 large, randomized controlled trials, which provide evidence regarding efficacy but are often not powered adequately to detect adverse events, especially less common or unknown adverse effects. Mandating that all trials be designed with adequate power to detect adverse events would provide more ideal safety data but would require enrollment of thousands of patients over many years and may be cost prohibitive for the development of new drugs. There is also the risk of publication bias, where negative or harmful trials are not published, although this practice has become less common with the advent of clinical trial registries (such as ClinicalTrials.gov), which increase the transparency of industry-funded research.
Independent organizations dedicated to pharmacovigilance are present worldwide. In 1961, the WHO established the Programme for International Drug Monitoring in response to thalidomide, a drug marketed for nausea gravidarum that caused significant birth defects. Canada followed in 1965 by establishing the Canada Vigilance Program, which collected reports on suspected adverse reactions for all health products. In 2005, this program was rebranded as MedEffect Canada, a comprehensive resource designed to improve access to all adverse drug reaction information, including adverse event reporting, advisories, safety alerts and recalls. A valuable MedEffect resource is the Adverse Reaction Online Database, where one can search for all reported adverse reactions for a given health product, including prescription and nonprescription drugs, biologics and natural health products. In 2012, over 53,000 adverse reactions to health products were reported, with almost 60% related to pharmaceuticals.7 Overall, 79% were deemed to be serious, which was defined as requiring/prolonging hospitalization or causing congenital malformation, disability or death. About one-third of reports were submitted by unspecified health care professionals (type not specified or other than a physician or pharmacist), and about one-quarter were submitted by physicians. Pharmacists submitted only 10% of reports, interestingly, 20% less than consumers or non–health care professionals. Clinicians should note that reporting of a suspected adverse reaction does not require one to demonstrate a correlation or direct cause-and-effect and can be submitted by any health care professional, patient or pharmaceutical company through completion of a standardized information collection form.
An approach to assessing adverse drug reactions
The reporting of suspected adverse reactions is particularly important for newer medications (drugs that have been on the market for 5 years or less), as this can help to identify rare adverse drug effects that are not recognized in clinical trials. When assessing suspected adverse drug reactions, it is imperative for clinicians to use a systematic approach. Although it is important to consider a drug-related cause, too often drugs are blamed for minor or nonspecific adverse events. In doing so, some patients may be deprived of first-line therapy in favour of alternatives with less evidence. Furthermore, when patients are taking multiple drugs, it can be difficult to elucidate which is the culprit, if any. Multiple standardized clinical tools exist to aid clinicians in deciding whether a drug may be the cause of an adverse event, which can then be easily interpreted by other clinicians. The most commonly used tool for assessing adverse events is the Naranjo algorithm, which was published in 1981.8 This scale is often used when reporting suspected adverse drug reactions as case reports in the published literature. The algorithm contains 10 items with 3 possible responses (“yes,” “no” or “do not know or not done”) and points are assigned for each response. The items are based on certain criteria such as temporal relationship, objective evidence (e.g., drug levels), other potential causes and dechallenge/rechallenge observations. One can then conclude whether an adverse event is “definite,” “possible,” “probable” or “doubtful” based on the cumulative score. The simplicity of the score makes it a useful tool for everyday clinical practice when a known or unknown drug-related adverse event is suspected. Another example of an adverse event scoring system is the WHO-Upsalla Monitoring Centre Causality Assessment.9 This scale ranks adverse events as “certain,” “probable/likely,” “possible” or “unlikely” based on criteria such as laboratory parameters and biological plausibility. However, unlike the Naranjo algorithm, it requires that all criteria for a certain causality term be met, which can lead to more ambiguity when assigning a probability.
Recent examples of pharmacovigilance
Health Canada continues to release advisories of suspected adverse drug reactions that have been discovered through pharmacovigilance. These include the risk of bladder cancer with pioglitazone, Clostridium difficile–associated diarrhea and bone fractures with proton pump inhibitors, diabetes with statins, cancer with prolonged use of calcitonin, liver damage with tolvaptan, intraoperative floppy iris syndrome with risperidone and paliperidone, and cardiac dysrhythmias with domperidone, citalopram and azithromycin.2 Additionally, the following are examples of safety warnings for 3 relatively new medications (Notices of Compliance from Health Canada issued between 2007 and 2009) that have been the subject of multiple postmarketing advisories regarding safety.
Dronedarone
Dronedarone, a novel antiarrhythmic agent released in 2009, has received a number of advisories regarding safety concerns both prior and subsequent to its introduction to the Canadian market. In 2003, the Antiarrhythmic Trial with Dronedarone in Moderate to Severe CHF Evaluating Morbidity Decrease (ANDROMEDA) study, which compared dronedarone with placebo in patients admitted to the hospital with new or worsening heart failure (HF), was discontinued early secondary to a 2-fold increase in death from any cause in patients receiving dronedarone.10 In March 2011, a Health Canada warning of potential dronedarone-induced liver injury was issued after 155 postmarketing cases of hepatobiliary adverse events were reported, of which 87 were deemed to be serious.2 In August 2011, another Health Canada safety warning was issued regarding an increased risk of CV events with dronedarone when used in patients with permanent atrial fibrillation (AF).2 This warning was based on the Permanent Atrial Fibrillation Outcome Study Using Dronedarone on Top of Standard Therapy (PALLAS) study, which was terminated prematurely due to a 2-fold increase in death from CV causes in patients receiving dronedarone, as compared with placebo.11 Finally, there are emerging case reports of serious lung-related toxicity associated with dronedarone use.2 In December 2011, Health Canada recommended dronedarone not be used in patients with permanent AF or any history of HF or left ventricular dysfunction and should be avoided in patients with a history of amiodarone-associated hepatic or pulmonary toxicity.2
Varenicline
In January 2012, Health Canada issued a review of the CV safety of varenicline, a partial nicotine receptor agonist indicated for smoking cessation.2 This review was based on a study of varenicline in patients with CV disease, which demonstrated a higher rate of adverse CV events with varenicline compared with placebo, though it did not reach statistical significance.12 From this, Health Canada concluded, “the possibility of an increased risk of heart attack or stroke [with varenicline] in patients with cardiovascular disease can neither be confirmed nor ruled out at this time.” Around the same time, a meta-analysis of 14 trials demonstrated a statistically significant increase in the rate of CV events with varenicline in all-comers, although the absolute risk was small compared with placebo (1.06% vs. 0.82%; odds ratio [OR], 1.72; 95% confidence interval [CI], 1.09-2.71).13 Two subsequent meta-analyses of 22 and 18 trials, respectively, also identified a higher number CV events with varenicline compared with placebo, although it did not reach statistical significance in either study.14,15 Overall, the evidence does not clearly demonstrate a link between varenicline and increased CV events; however, it may be advisable for clinicians to try other therapies (e.g., nicotine replacement therapy) before varenicline until more data are available regarding its CV safety. This was communicated in another Health Canada release in May 2013.2
Dabigatran
There is ongoing debate regarding the safety of dabigatran, a novel oral anticoagulant indicated for AF and prevention of venous thromboembolism. The primary safety concern with dabigatran is the risk of bleeding. A safety alert from the American Institute for Safe Medication Practices in January 2012 stated that 932 serious adverse events, 54% of which were hemorrhagic, and 120 deaths had been linked to dabigatran, which exceeded all other medications, including warfarin.16 However, this must be interpreted cautiously, as hemorrhagic events with warfarin are not often reported anymore. Nonetheless, Health Canada issued a safety warning in March 2012 reminding clinicians to evaluate patients’ renal function prior to initiating dabigatran, as it is cleared primarily by the kidneys, and that ongoing monitoring of renal function is imperative to minimize the risk of bleeding. Another important consideration with dabigatran is CV safety. A recent meta-analysis of 7 trials demonstrated a 33% relative increase in CV events with dabigatran compared with control, although a safety warning regarding these data has never been issued by Health Canada.17 Finally, although not related to an adverse event, another important safety issue with dabigatran involves its former brand name Pradax—Health Canada released an advisory in November 2011 reminding clinicians of the potential confusion with Plavix, the brand name for clopidogrel.2 Subsequently, the manufacturer has changed its brand name to Pradaxa to avoid this confusion.
Future considerations
The current model of pharmacovigilance in Canada raises questions of improvement worthy of further contemplation. First, should the reporting of suspected drug-related adverse events be mandatory? Although this would likely increase the number of reported adverse events, another important consideration is enforcement. Would the cost of ensuring compliance exceed the potential gains? Furthermore, increased reporting of adverse events does not necessarily translate into better patient safety. The sheer volume of reported events may paradoxically make it more difficult to identify rare adverse effects due to the increased workload. Further detailed evaluation of such a strategy is necessary. Second, is the current system for drug approval in Canada rigorous enough to determine whether a drug is associated with a rare but serious adverse effect? In other words, should a drug ever be approved based on 1 or 2 clinical trials? Health Canada is attempting to address this issue by introducing progressive licensing for new drugs.18 This initiative is aimed at providing an ongoing evaluation of the benefits and risks of a drug throughout its life cycle, which will aid in the detection of rare adverse effects and will improve the transparency of how drugs are approved for use in Canada. However, this does not address the issue of safety in certain patient populations who were underrepresented or excluded from the clinical trials. Physicians will frequently extrapolate the evidence from these trials and apply it in an “off-label” fashion to a broader range of patients—how does one quantify the potential risk in these patients? Third, are clinicians providing patients with sufficient information regarding potential adverse drug reactions? When discussing drug therapy with a patient, it can be challenging to balance the potential benefits and risks. The sheer number of possible adverse effects of drug therapy (although most occur in less than 1% of patients) can elicit patient concern and can negatively affect adherence to therapy. So how much information is enough to allow the patient to make an informed decision without being overwhelmed? There appears to be no way to circumvent this issue—patients need to know all the potential risks of drug therapy, including new suspected adverse effects, to make a truly informed decision.
The role of the pharmacist
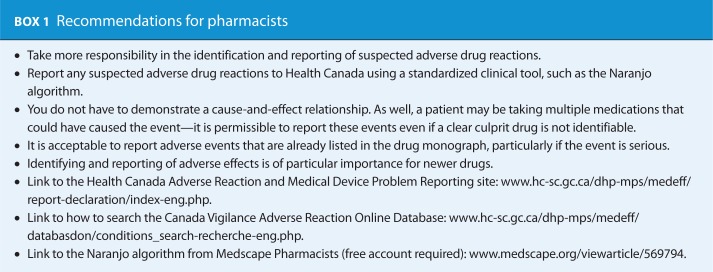
Pharmacists are ideally situated to play a key role in the identification and reporting of suspected drug-related adverse effects due to our accessibility and knowledge of drug therapy (see Box 1). As stated, the reporting of suspected adverse drug reactions does not mandate that a direct cause-and-effect relationship be established. All that is required is to document the reaction itself and the circumstances around how it occurred (relevant history, investigations, concurrent medications, etc.). In 2012, pharmacists submitted only 10% of Health Canada adverse drug reaction reports, which is unacceptably low. As a profession, we need to accept responsibility to ensure this activity is performed systematically and consistently for all suspected adverse drug reactions.
Conclusion
The identification and reporting of suspected adverse drug reactions through pharmacovigilance is an important patient safety activity that is the responsibility of all clinicians. Pharmacovigilance is particularly important for newer drugs, as rare adverse effects are not always identified in clinical trials and the prescribing of medications in the “real world” often yields new drug-related safety concerns. The most important lesson we can learn from the ill-fated existence of rofecoxib is that it is unlikely to remain an isolated example. As long as our drug approval process in Canada remains unchanged, rofecoxib will not be the last “blockbuster” drug to be removed from the market due to safety concerns. ■
Footnotes
Author Contributions:Dr. Barry initiated the project, wrote the draft of the manuscript and revised the final manuscript. Dr. Koshman contributed to the writing of the manuscript and revised the final manuscript. Dr. Pearson contributed to the writing of the manuscript and revised the final manuscript.
Declaration of Conflicting Interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Neilan T. Merck pulls Vioxx painkiller from market, and stock plunges. The New York Times. 2004. September 30 Available: www.nytimes.com/2004/09/30/business/30CND-MERCK.html (accessed December 21, 2013).
- 2. MedEffect™ Canada. Health Canada website. Available: www.healthcanada.gc.ca/medeffect (accessed August 7, 2012).
- 3. Bombardier C, Laine L, Reicin A, et al. Comparison of upper gastrointestinal toxicity of rofecoxib and naproxen in patients with rheumatoid arthritis. N Engl J Med 2000;343:1520-8. [DOI] [PubMed] [Google Scholar]
- 4. Bresalier RS, Sandler RS, Quan H, et al. Cardiovascular events associated with rofecoxib in a colorectal adenoma chemoprevention trial. N Engl J Med 2005;352:1092-102. [DOI] [PubMed] [Google Scholar]
- 5. Lexchin J. Drug withdrawals from the Canadian market for safety reasons, 1963-2004. CMAJ 2005;172:765-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. World Health Organization. Pharmacovigilance. Available: www.who.int/medicines/areas/quality_safety/safety_efficacy/pharmvigi/en/index.html (accessed February 17, 2012).
- 7. McMorran M, McEnaney J. Adverse reaction and incident reporting—2012. Canadian Adverse Reaction Newsletter 2013;23:2-5. Available: www.hc-sc.gc.ca/dhp-mps/alt_formats/pdf/medeff/bulletin/carn-bcei_v23n3-eng.pdf (accessed August 8, 2013). [Google Scholar]
- 8. Naranjo CA, Busto U, Sellers EM, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther 1981;30:239-45. [DOI] [PubMed] [Google Scholar]
- 9. The Uppsala Monitoring Centre. The use of the WHO-UMC system for standardised case causality assessment. Available: http://www.who-umc.org/Graphics/26649.pdf (accessed August 7, 2012).
- 10. Køber L, Torp-Pedersen C, McMurray JJV, et al. Increased mortality after dronedarone therapy for severe heart failure. N Engl J Med 2008;358:2678-87. [DOI] [PubMed] [Google Scholar]
- 11. Connolly SJ, Camm AJ, Halperin JL, et al. Dronedarone in high-risk permanent atrial fibrillation. N Engl J Med 2011;365:2268-76. [DOI] [PubMed] [Google Scholar]
- 12. Rigotti NA, Pipe AL, Benowitz NL, et al. Efficacy and safety of varenicline for smoking cessation in patients with cardiovascular disease: a randomized trial. Circulation 2010;121:221-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Singh S, Loke YK, Spangler JG, Furberg CD. Risk of serious adverse cardiovascular events associated with varenicline: a systematic review and meta-analysis. CMAJ 2011;183:1359-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Prochaska JJ, Hilton JF. Risk of cardiovascular serious adverse events associated with varenicline use for tobacco cessation: systematic review and meta-analysis. BMJ 2012;344:e2856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mills EJ, Thorlund K, Eapen S, et al. Cardiovascular events associated with smoking cessation pharmacotherapies: a network meta-analysis. Circulation 2014;129:28-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Institute for Safe Medication Practices. Signals for dabigatran and metoclopramide. QuarterWatch 2011; January 2012. Available: www.ismp.org/quarterwatch/pdfs/2011Q1.pdf (accessed August 7, 2012).
- 17. Uchino K, Hernandez AV. Dabigatran association with higher risk of acute coronary events. Arch Intern Med 2012;172:397-402. [DOI] [PubMed] [Google Scholar]
- 18. Health Canada. Progressive licensing. Available: www.hc-sc.gc.ca/dhp-mps/homologation-licensing/index-eng.php (accessed December 21, 2013).